SIR: We recently imaged a 13-year-old boy with Tourette's syndrome (TS) and obsessive-compulsive disorder (OCD) who demonstrated a basal ganglia lesion on MRI.
At 6 years of age, J.M. developed tics, which involved twitching, vocalizations, head turning, throat clearing, and eye blinking. He later also developed signs of OCD, including obsession with order, ritualistic arranging, and repeated performance of tasks. With the exception of tics, his neurological exam was normal.
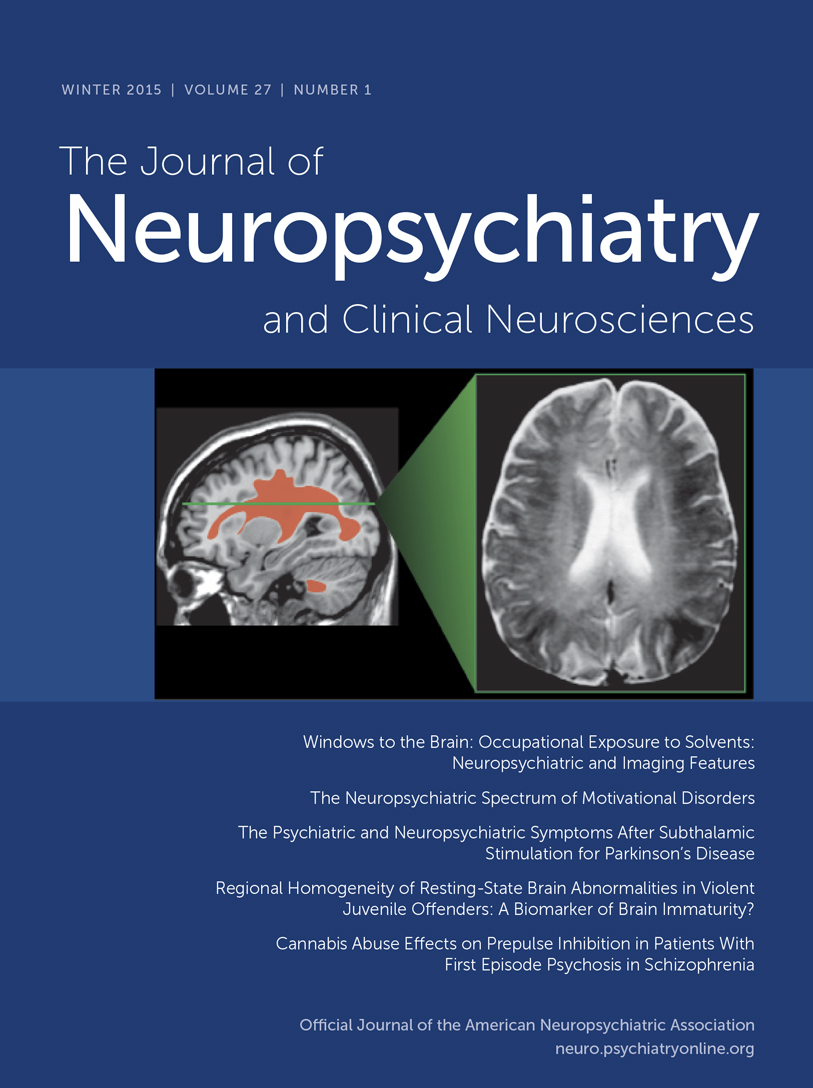
An MRI was performed using a 1.5-tesla GE Signa scanner. A 5-mm×3-mm focus of high signal intensity was seen on both T1- and T2-weighted images in the medial aspect of the left globus pallidus. There was no edema, mass effect, or enhancement with gadolinium. No abnormality was present in the right basal ganglia. A CT scan was performed using a third-generation Picker scanner. Thin overlapping slices through the basal ganglia, with and without contrast, were normal. The metabolic workup was normal, and the exact nature of the lesion remains indeterminate.
Dating back to Gilles de la Tourette's original description of the disorder, an association between TS and OCD has been hypothesized. This hypothesis is supported by the high incidence of OCD in patients with TS, estimates of which average around 50%.
1 Furthermore, various focal lesions and structural abnormalities of the basal ganglia have been implicated in the pathophysiology of both disorders.
2,3Functional imaging studies have implicated the corpus striatum and corticolimbic system in the etiology of TS by demonstration of decreased metabolism in these regions when compared with control subjects.
4 With respect to OCD, SPECT studies have shown abnormal blood flow in the basal ganglia,
5 and functional studies with PET have resulted in similar findings, including abnormally high activity in the orbital frontal cortex and the caudate.
6Morphometric studies have resulted in findings that complement the functional studies by demonstrating reduced size of the various components of the basal ganglia in individuals with TS
7 and derangements in caudate nucleus volume
8 and asymmetry of T
1 relaxation time in the caudate nuclei of individuals with OCD.
9It appears that the association between TS, OCD, and basal ganglia pathology is gaining credence; additional references are available but are beyond the scope of this brief report. We submit this case to the body of literature to illustrate the comorbidity between OCD and TS and add support to the possibility of basal ganglia pathology underlying these disorders. It is important to be aware of the high comorbidity of these disorders and their presumed pathophysiologic mechanisms so that we may give special attention to the basal ganglia in the imaging of these patients.