Current neurobiological models of obsessive-compulsive disorder (OCD) involve dysfunctions in the orbitofrontal and anterior cingulate cortices, as well as the striatum and thalamus.
1 Neuropsychological studies have been consistent with subtle deficits involving these structures, reporting deficits in visuospatial abilities, nonverbal memory, and executive functions in the presence of intact language, verbal memory, and intellectual abilities.
2An important question is whether those findings can be extended to subjects who do not meet diagnostic criteria for OCD. The study of subclinical samples, selected on the basis of self-administered instruments, has permitted investigation of the neuropsychological correlates of obsessive-compulsive (OC) phenomena; this approach has the potential benefit of overcoming some of the methodological limitations associated with clinical samples, such as medication or symptomatic state effects that may affect neuropsychological performance.
3,4 The results of those studies in subclinical samples have been consistent with current models of OCD. For example, a recent study reported that subclinical OC subjects show difficulties in solving the Tower of Hanoi puzzle, a measure of executive functioning that requires manipulation of spatial information.
4Fluency tasks are measures of executive functioning that are sensitive to the functioning of the frontal lobes.
5 There is evidence that performance on
design fluency tasks may be particularly sensitive to right frontal cortical functions
6 and that
verbal fluency may be especially sensitive to left frontal functions.
5The present study systematically examined the verbal and design fluency abilities of a subclinical OC sample in order to further characterize the neuropsychological profile associated with nonclinical obsessive-compulsive phenomena. On the basis of previous neuropsychological studies of OCD, we predicted that subclinical OC subjects would show reductions on design fluency, as well as on verbal fluency tasks involving a set-shifting component. Such results would provide support for a dimensional model of obsessive-compulsive phenomena with an assumed continuity between normal and abnormal obsessions and compulsions.
METHODS
Following the methodology from previous studies,
3,4 we recruited an independent cohort of 52 subjects from a new pool of 476 undergraduates at the Universitat de Barcelona on the basis of their scores on the Spanish version of the Padua Inventory (PI), a well-validated measure of OC symptoms.
7 Completing the present study were 25 subclinical obsessive-compulsive subjects (21 women, 4 men; mean age=18.7±0.7 years; 4 left-handed) who scored higher than 1 standard deviation above the mean (PI≥86; mean=101.4±13.8) and 27 noncompulsive control subjects (23 women, 4 men; mean age=19.1±1.3 years; 1 left-handed; 33≤PI≤55; mean=41.9±14.2; means and standard deviations). Exclusion criteria were history of OCD or other psychiatric disorders. Three subjects met DSM-IV criteria for OCD and hence were excluded from the OC group; 1 subject was excluded from the control group because of missing data. Groups did not differ on gender or handedness. Preliminary analyses showed no effect of those variables on the overall results, and they were not further examined.
Three fluency tests were administered to the sample: two verbal fluency tests and one design fluency test. In the FAS test,
8 the subjects were asked to generate as many words as possible beginning with the letters F, A, and S for 90 seconds. In the Category Alternation Test (CAT), following Newcombe's
9 procedure, subjects had to name as many different items as possible from two categories of objects (animals and fruits) for 90 seconds. The Design Fluency Test (DFT), based on the test developed by Jones-Gotman and Milner,
6 consists of two conditions. In the
free condition, the subjects had to invent drawings that are not actual objects or nameable abstract forms (e.g., geometric shapes). Subjects were given 4 minutes to make up as many different kinds of such drawings possible. In the
fixed condition, subjects were asked to generate as many different figures as possible, each contained in two vertical parallel lines, for 4 minutes.
In addition, the subjects were given the Raven's Advanced Progressive Matrices (RAPM) as a measure of general nonverbal intelligence. The State subscale of the Spielberger State-Trait Anxiety Inventory (STAI) and the Beck Depression Inventory (BDI) were also administered to control for anxiety and depression at the time of testing. Subjects were tested by two trained neuropsychologists. Blindness was assessed by asking the raters to guess the subject's group membership. Kappas were low (0.02 to 0.1).
Statistical analyses included multivariate analyses of covariance (MANCOVAs) comparing the two groups with the four fluency tasks as dependent variables and the state measures (STAI, BDI) as covariates; one-way analyses of variance; Mann-Whitney U-tests; and Pearson correlations.
RESULTS
The OC and control groups did not differ on the RAPM (means±SD: OC: 23.2±6.2; control: 22.4±4.7; F=0.24, df=1,50, not significant). OC subjects tended to be more anxious (STAI: 23.08±11.5) and depressed (BDI: 9.7±6.9) than control subjects (STAI: 16.6±5.4; BDI: 5.6±5.9) at the moment of the testing (STAI: Mann-Whitney U=238, P=0.06; BDI: F=5.24, df=1,50, P=0.02).
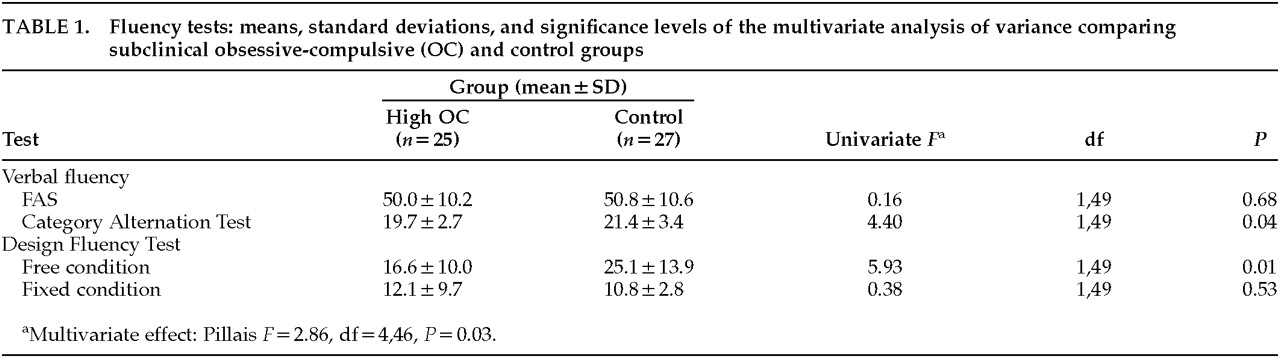
MANOVA with the four fluency tasks as dependent variables revealed a significant multivariate effect (
Table 1). Univariate
Fs showed that between-group differences were due to performance on the CAT and the
free condition of the DFT. However, introduction of the STAI and the BDI as covariates in the model reduced group differences on the CAT to nonsignificance (
F=1.98, df=1,47, not significant) because of the effect of state anxiety (β=–0.35,
t=–2.3,
P=0.02). The multivariate effect, however, became more pronounced (
F=3.17, df=4,44,
P=0.02), as did the univariate
F for the DFT
free condition (
F=9.91, df=1,47,
P=0.003). The PI total score was significantly negatively correlated with the DFT performance (Pearson
r=–0.35,
P=0.01, two-tailed), but not with the CAT (
r=–0.17, not significant).
DISCUSSION
As previously reported in both subclinical and clinical samples,
4,10 no differences were found on the phonemic fluency task (FAS). As predicted, subclinical OC subjects showed a reduced fluency on the Category Alternation Test, which involves set-shifting abilities in addition to verbal fluency. However, those differences disappeared when state anxiety was controlled as a covariate. Moreover, the CAT performance was not significantly correlated with obsessionality but was correlated with state anxiety. Reduction in semantic category alternation in OCD was reported by Harvey,
11 but not in a better-controlled study by Head et al.
12 It is possible that category alternation performance is mediated by state anxiety and does not constitute a basic cognitive deficit in OCD.
The results confirmed the hypothesis of a reduced design fluency in subclinical OC subjects. Design Fluency Test performance was significantly negatively correlated with obsessionality. The fact that only the DFT
free condition showed between-group differences is consistent with recent findings suggesting that OCD patients have special difficulties in organizing nonstructured material.
13 Furthermore, the
fixed condition is less sensitive to frontal dysfunction than the
free condition.
5The finding of a reduced design fluency may suggest a subtle dysfunction of the right corticostriatal systems in subclinical OC subjects. An alternative interpretation of the data, although the two are not mutually exclusive, is that the differences in performance between groups might reflect differences in cognitive style rather than deficits in those systems. The results are consistent with the current neurobiological models of OCD
1 and provide further support for a dimensional model of obsessive-compulsive phenomena that assumes a continuity between normal and abnormal OC behavior.
ACKNOWLEDGMENTS
This work was partially supported by Grants FISss 94/0908 and DGICYT PM95/104. The first author's work was funded by the Spanish Ministerio de Educación y Ciencia.