Apathy is a neuropsychiatric symptom that is prominent among patients infected with human immunodeficiency virus (HIV). Apathy refers to a reduction in cognitive, emotional, or motor behavior.
1 The point prevalence and lifetime prevalence of apathy among HIV-infected individuals have not been determined, but the frequency is believed to be greater than that observed among the general population. The symptoms of apathy are similar to symptoms of depression, but the two can be reliably distinguished.
2–4 In addition, apathy, unlike depression, may reflect a direct consequence of the infection on the brain function. Damage to subcortical regions of the brain parenchyma among seronegative individuals frequently results in increased apathy, a finding that has been reported across patient populations.
5–6 Increased apathy following damage to subcortical pathways presumably occurs due to disruption of information transfer between frontal cortex and the striatum. Since HIV resides in greatest concentration in deep subcortical nuclei,
7–8 it is possible that reciprocal circuits between the frontal cortex and subcortical structures are affected by the presence of the virus in the brain.
Two previous studies have reported significant correlations between apathy and cognitive dysfunction in HIV, an observation that provides support for the position that apathy may be a direct manifestation of CNS disturbance. In one study, Castellon et al.
9 assessed apathy in multiple groups of HIV patients with varying levels of disease severity. High ratings of apathy were strongly correlated with ratings of depression and poorer performance on a measure of working memory, but not with cluster designation 4 (CD4) count. The relationship between cognitive performance and apathy was most evident among individuals with AIDS and more severe cognitive dysfunction. In a second study, Castellon et al.
10 again found strong correlations between ratings of apathy and performance on a dual-task reaction time task and the interference trial of the Stroop test. Importantly, these effects were not mediated by disease severity, suggesting that apathy may be an important marker of CNS disturbance even among patients with less severe disease.
In contrast to the findings above, Rabkin et al.
11 did not find significant relationships between ratings of apathy and performance on measures of neuropsychological function. Rabkin et al. examined apathy in a large cohort of HIV-infected men and women with advanced disease. In agreement with the findings of Castellon et al.,
9–10 ratings of apathy and depression were strongly correlated in this study. However, ratings of self-reported apathy correlated significantly with only one measure of cognitive function among the female sample, and there were no significant relationships between apathy and performance on any of the cognitive tests for the sample of males. The authors concluded that the absence of a significant relationship between cognition and apathy indicates that apathy may not represent CNS disturbance in this population.
The inconsistent findings described above are difficult to reconcile because apathy was measured using different methods. Castellon et al.
9 assessed apathy using a very brief clinical interview, whereas Rabkin et al.
11 assessed apathy using a self-report measure, albeit a measure with very good psychometric properties. Furthermore, individuals included in the studies conducted by Castellon et al.
9 evidenced greater cognitive impairment compared to the individuals included in the study by Rabkin et al.
11 The purpose of the present study is to clarify the relationship between apathy and cognitive function in patients with HIV. We administered a reliable and valid measure of apathy to a sample of patients and a sample of comparison subjects. We predicted that apathy would be significantly elevated in patients with HIV, and that ratings of apathy would be inversely correlated with cognitive performance. By contrast, we predicted that severity of depression would not be associated with cognitive function.
METHODS
Subjects
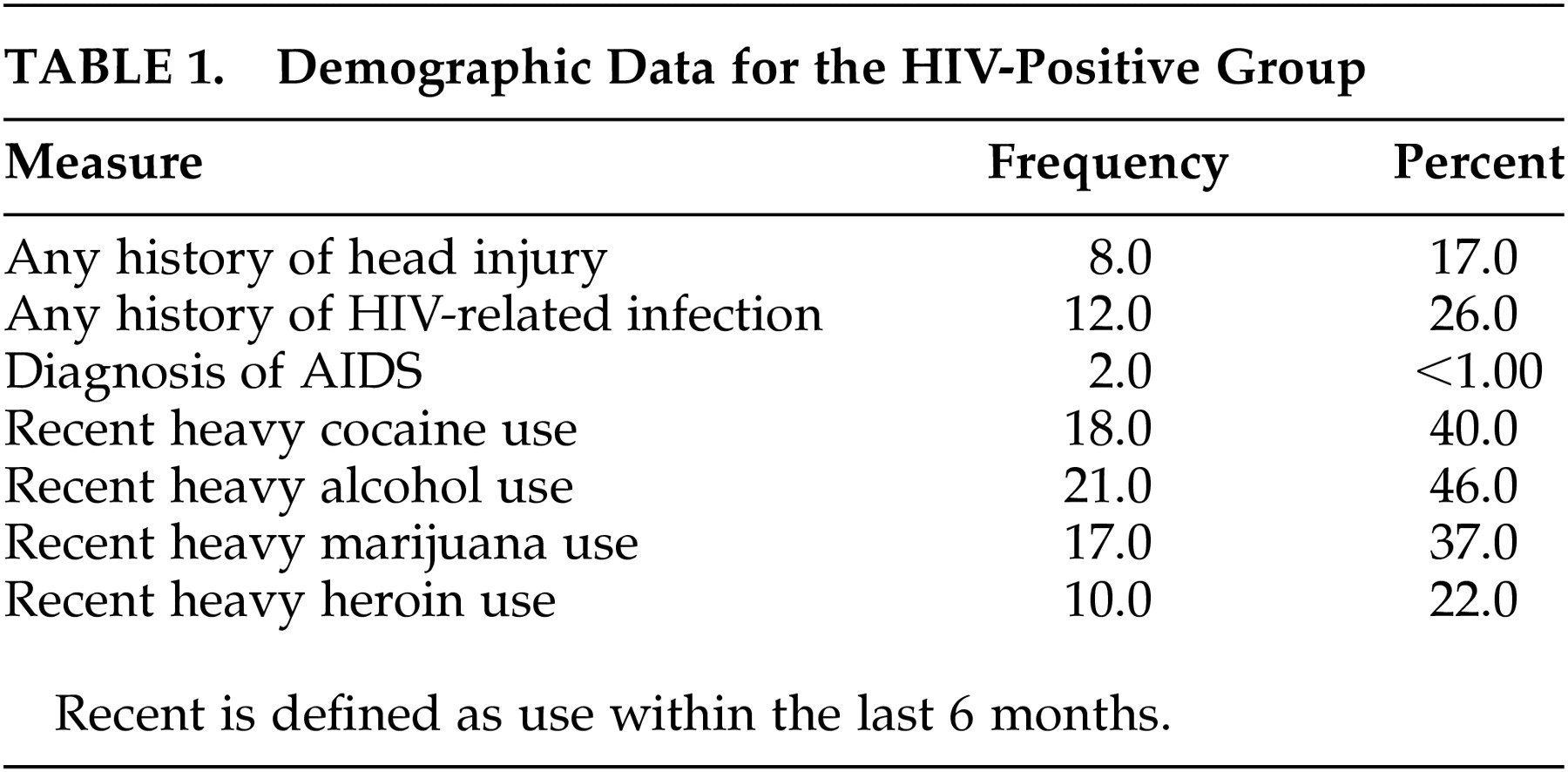
A total of 45 individuals diagnosed with HIV were recruited from the Immunology Clinic at Miriam Hospital, Providence, Rhode Island. Diagnosis of HIV was based on ELISA blood assay and Western blot. Patients with a history of major psychiatric disorder (schizophrenia, bipolar disorder), neurologic disorder, learning disability, or developmental disability were excluded from the study. Patients were not excluded if they reported a history or recent substance abuse or if they reported clinically elevated depression. The patients averaged 42.7 (5.7) years of age, 12.5 (2.7) years of education, 95.5 (63.7) months since diagnosis. The median CD4 cell count was 310. A total of 13 patients were taking a protease inhibitor, 31 patients were taking a nucleoside reverse transcriptase inhibitor and 15 were taking a nonnucleoside reverse transcriptase inhibitor. All patients were taking a combination of the medications consistent with highly active antiretroviral therapy (HAART).
Twenty-two comparison subjects were recruited from the community (e.g., relatives of the patients, hospital employees). Comparison subjects were required to meet the same exclusion criteria described above and averaged 38.6 (10.7) years of age and 15.8 (2.2) years of education. All participants received financial compensation for participation in the study. Written informed consent was obtained prior to enrollment.
Procedure
All participants completed demographic questionnaires and self-report measures of apathy and mood. All participants were administered a battery of cognitive tests sensitive to HIV-associated neuropsychological impairments. A trained research technician administered the neuropsychological tests. All measures were administered and scored according to standard procedures.
Neuropsychiatric Measures
Apathy.
The Apathy Evaluation Scale–Self-report version (AES
1) was administered to measure apathy. The AES is a brief self-report measure of apathy behavior that has good validity and reliability.
1 The measure consists of 18 questions, and subjects were required to respond to their degree of agreement with each question using a Likert scale where 1=not at all and 4=extremely. Higher scores reflect greater apathy. The dependent measure was total score.
Mood.
Mood was assessed with the Chicago Multicomponent Depression Inventory (CMDI; Nyenhuis et al.).
12 The CMDI is a 42-item self-report inventory that assesses three aspects of depression including mood, self-evaluative, and somatic symptoms, and separate subscales measure these three areas of mood. The Affective Subscale, Evaluative Subscale, and Vegetative Subscale consist of 14 items each. Subjects are required to circle the answer that best describes how they feel using a 5-point Likert scale. Each scale has strong reliability and validity, and correlates very highly with clinical measures of depression.
13–14 The Affective Scale is particularly useful in this population as it is not confounded by the vegetative symptoms of immune diseases.
14Cognitive Measures
Symbol Digit Modalities Test (SDMT).15
The oral version of the SDMT was administered as a measure of information processing speed. This test required subjects to substitute numbers for symbols using a key that remained in constant view. Number of correct substitutions in 90 seconds served as the dependent variable.
The Trail Making Test.
The Trail Making Test consists of two measures: Trails A and Trails B. Trails A is a test of psychomotor speed that requires subjects to connect numbers in ascending order. Trail Making Test B is a measure of combined visual search, psychomotor speed, and cognitive flexibility. Part B of the Trail Making Test assesses the shifting and maintenance of response set by requiring individuals to sequentially alternate between alpha-numeric sequences (e.g., 1-A-2-B-3-C).
Hopkins Verbal Learning Test–Revised (HVLT–R).16
The HVLT-R is a standard clinical measure of learning and memory. The test involves three learning trials of a list that consists of 12 words. The learning trials were followed by an uncued long-delay recall trial and a recognition trial. For the purpose of this study, total recall across the three learning trials was used as the dependent measure.
Brief Visual Memory Test-Revised.17
The BVMT-R is a visual analogue to the HVLT-R. The test consists of three learning trials, a delayed free recall trial, and a recognition trial. On the learning trials, the subjects are presented with six geometric designs. After 10 seconds of presentation, the designs are removed from sight and the subject is required to reproduce both the shape and the location of each design. The dependent measure was the total correct across the three learning trials.
Grooved Pegboard Test.
On this test, subjects were required to manipulate small pegs into holes on a board. The orientation of the holes in the board varies, and therefore subjects are required to manipulate the pegs using only one hand. Each hand was tested and time to completion for the dominant hand served as the dependent variable.
Statistical Analyses.
Performance on the cognitive measures, apathy scale and mood scale was compared between the two groups (healthy comparison and HIV-positive individuals) using a MANCOVA with age and education entered as covariates. Univariate comparisons were then examined to contrast the two groups on the individual measures. Correlational analyses were performed separately for each group to examine the association between apathy, mood disturbance, performance on the cognitive tests, and CD4 cell count.
RESULTS
Cognitive Performance
The healthy comparison group was significantly younger (F (1,65) = 4.2, p<0 .05) and more educated than the HIV group (F(1,65) = 24.0, p<0.05). Results of the MANCOVA to contrast cognitive function revealed a significant difference between the two groups (Wilks’ lambda = 0.77, (F = 2.78), p<0.05). Univariate comparisons revealed that performances on the cognitive measures differed between the two groups on the Trail Making B test (F (1,61) = 5.0, p<0 .05) and learning trials across the BVMT-R test (F (1,61) = 15.9, p<0 .01). On each of these comparisons, the HIV-positive group performed more poorly than the healthy comparison group.
Apathy and Depression
The HIV-positive group also reported significantly greater apathy (F (1,61) = 7.9, p< 0.05) and depressive symptoms (F (1,61) = 7.3, p< 0.05) compared to the healthy comparison sample. Among the HIV-positive group, the correlation between apathy score and rating of mood disturbance on the mood subscale of the CMDI was not significant (r = 0.07, p>0.05). Similarly, the correlation between apathy and CD4 cell count (r = −0.07, p>0.05) was not statistically significant. By contrast, apathy did correlate strongly with disease duration (r = 0.41, p<0.05), with greater apathy reported among individuals with longer disease duration.
Relationship Between Cognitive Performance and Neuropsychiatric Status
Correlational analyses revealed that severity of apathy was associated with poorer performance on the BVMT-R total learning (r = −0.30, p<0.05), HVLT–R total learning (r = −0.43, p<0.05), and Trail Making B (r = 0.31, p< 0.05). By contrast, apathy was unrelated to total score on the FAS task, Grooved Pegboard, or Symbol Digit task (rs < 0.27). Severity of depression correlated significantly with performance on BVMT-R total learning (r= −0.30, p<0.05) but not with any other measure. CD4 cell count was related to cognitive function on the Symbol Search task (r = 0.39, p< 0.05) but not any other measure.
DISCUSSION
Disruption of frontostriatal structures and circuitry is believed to underlie the expression of cognitive dysfunction in patients infected with HIV. Apathy is also common among HIV-infected adults, and previous studies have suggested that cognitive impairment and apathy may share common neurophysiological substrates. The results from our study provide some additional, though still indirect, support for this position. We observed a significant relationship between severity of apathy and cognitive performance in a sample of patients with both elevated apathy scores and subtle cognitive impairment. The severity of depression was associated with performance only one cognitive test and ratings of depressed mood did not co-vary with ratings of apathy. The latter finding indicates that the two can be dissociated in this population. This finding is contrary to previous reports.
9 The fact that depression and apathy were dissociated in this sample likely reflects the use of the CMDI Affective Scale to measure mood disturbance. This subscale provides a relatively "pure" assessment of mood disturbance, which is not confounded by physical symptoms, and therefore it may provide a more accurate estimate of mental health in this population compared to other measures.
In previous studies,
9–10 the presence of apathy was strongly related to poorer performance on measures of working memory and response inhibition. These findings were interpreted to represent preliminary evidence that apathy and neuropsychological impairment in HIV may evolve from similar neuropathological mechanisms. Results from our study revealed a significant association between apathy and poorer performance on a measure of cognitive flexibility and measures of learning efficiency. Since frontostriatal systems subserve performance on these tests,
18 our findings provide additional evidence that apathy and cognitive dysfunction in HIV may share common neurophysiological susbtrates. An important caveat to consider, however, is that not all measures of cognitive function were associated with higher ratings of apathy in our study, and the magnitudes of the correlation coefficients were not exceptionally strong. Clearly other factors not directly measured in this study influence the expression of both apathy and cognitive function in patients with HIV.
Contrary to the findings reported in this study, Rabkin et al.
11 did not observe significant associations between apathy and cognitive function. The discrepancy is interesting because both studies administered similar cognitive tests and the same measure of apathy in both studies. One important difference between the two studies is the severity of cognitive impairment reported for the HIV-positive samples. In the study reported by Rabkin et al.,
11 only 9/75 HIV-infected men and 26/58 women exhibited cognitive impairment compared to healthy comparison subjects. Also, that study included individuals with complications that may have influenced their cognitive status independent of HIV (e.g., learning disability, special education). These findings in conjunction with those reported by Castellon et al.
9–10 suggest that significant relationships between apathy and cognitive function exist predominately among individuals with significant cognitive difficulties compared to healthy comparison subjects.
Interestingly, we found that apathy was significantly associated with disease duration, but not with CD4 cell count. The implications of this finding are not entirely clear, but it is important to recognize that CD4 cell count fluctuates acutely, and therefore it may not provide an optimal marker of CNS dysfunction at the time that cognition is examined. By contrast, disease duration may offer a useful index of disease impact since previous studies have demonstrated that the virus enters the brain within weeks of initial infection. If apathy in HIV develops secondary to CNS dysfunction, it would make sense that duration correlates with severity of apathy. This, however, does not explain the lack of an association between disease duration and cognitive function.
The observation that cognitive function and apathy are correlated provides only indirect information regarding potential underlying mechanisms, and the nature of these mechanisms will remain speculative until a more direct link is established. One approach that would be extremely informative is to incorporate functional neuroimaging. Magnetic resonance spectroscopy (MRS) and diffusion tensor imaging (DTI) provide indices of neuronal integrity, and they are sensitive to abnormalities,
19–21 even among asymptomatic individuals. It would be of interest to examine the relationship between abnormalities observed on functional neuroimaging, cognitive function, and ratings of apathy both in the early and later stages of disease activity. Evidence of a strong relationship between neuronal abnormalities and increased apathy would provide more compelling data to support the relationship between CNS involvement and this common neuropsychiatric symptom.
ACKNOWLEDGMENTS
This study was funded in part by grants from the National Institute of Drug Abuse and the National Institute of Mental Health to Dr. Robert Paul.