Pharmacological treatment of aggressive and impulsive behavior is complicated, and no standard “best practice” exists. A variety of guidelines has been proposed, some based on theoretical constructs related to putative neurotransmitter disturbances
8 and others relating to aggression associated with specific clinical presentations.
9 Several classes of drugs have been evaluated for their effectiveness in controlling aggression and impulsivity, including lithium, selective serotonin reuptake inhibitors, anticonvulsants, beta-adrenergic receptor antagonists, antipsychotics, and stimulants.
9–11 Most placebo-controlled trials have revealed superiority of these agents over placebo,
10 though it is difficult to predict what agent may be most effective for each individual patient. As a consequence, high doses of medication, polypharmacy, and frequent “prn” medications are often used. More recently, clozapine has shown promise in reducing aggression in patients with schizophrenia
11–13 and in patients with borderline personality disorder and psychosis.
14Here, we report a case series of diagnostically heterogeneous, persistently violent patients who responded to treatment with clozapine. All of these patients failed to respond adequately to multiple prior medication trials. We propose that clozapine is a viable pharmacological treatment option for violent behavior, regardless of the underlying psychiatric diagnosis.
RESULTS
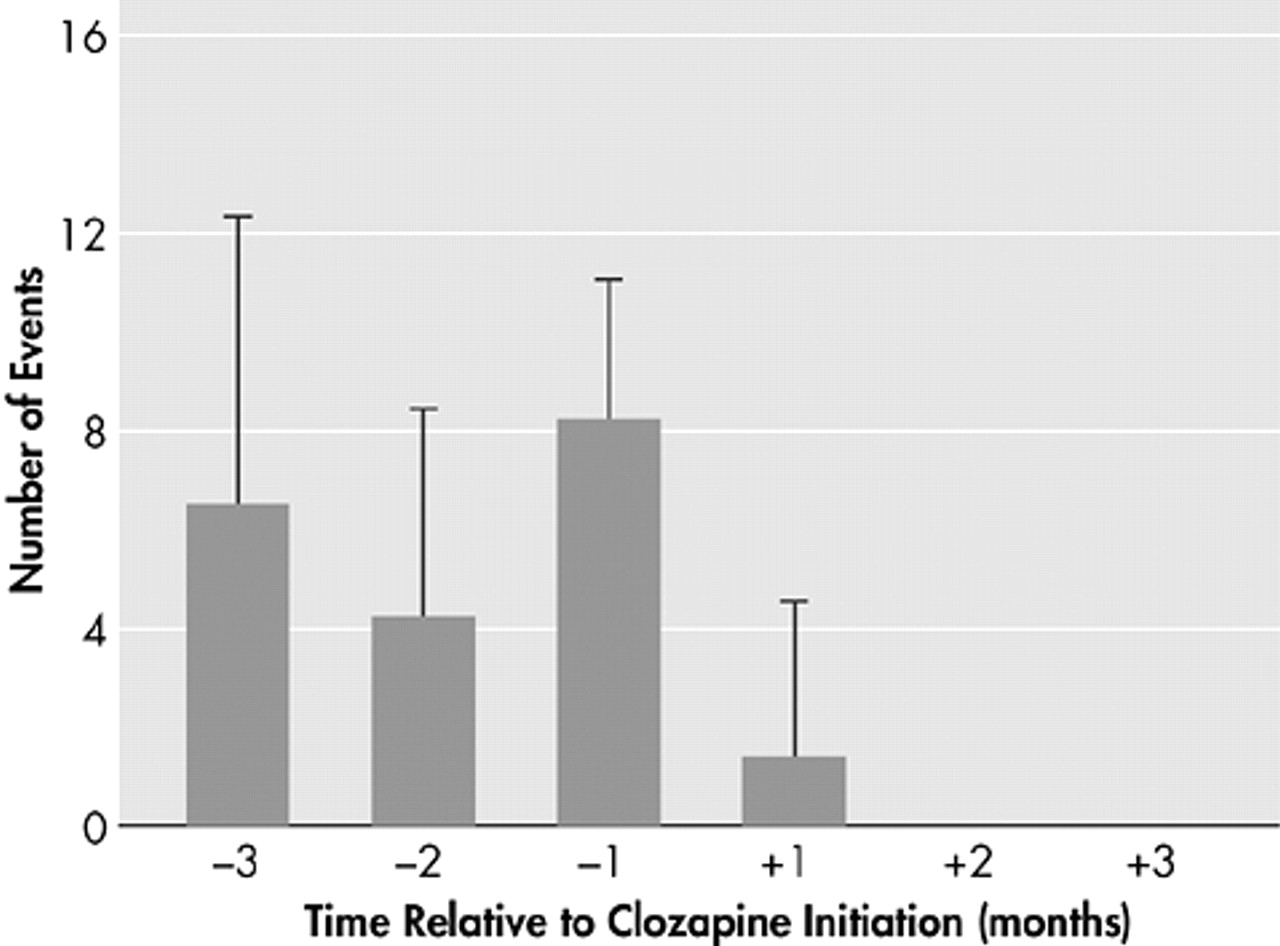
Figure 1 shows the cumulative effect of clozapine treatment on the number of violent events in five persistently violent patients who met inclusion criteria as defined in the methods section. Analysis of variance revealed significant differences in the number of violent episodes as a function of time relative to clozapine treatment (p=0.003). Post hoc analysis revealed that the number of events 1 month prior to treatment was significantly greater than the number of events 1 month (p=0.039) and 2 months (p=0.009) after treatment. Comparison of average number of total violent events in the 3 months before (mean=6.4 events, SD=4.3) and 3 months after (mean=0.5 events, SD=1.9) clozapine treatment showed a highly significant effect of clozapine treatment (p<0.001, two-tailed Student’s t test).
What follows are brief clinical summaries of each of the five patients whose pooled data are shown in the Figure. These summaries provide qualitative details of clinical care, as well as the diagnoses of the patients treated.
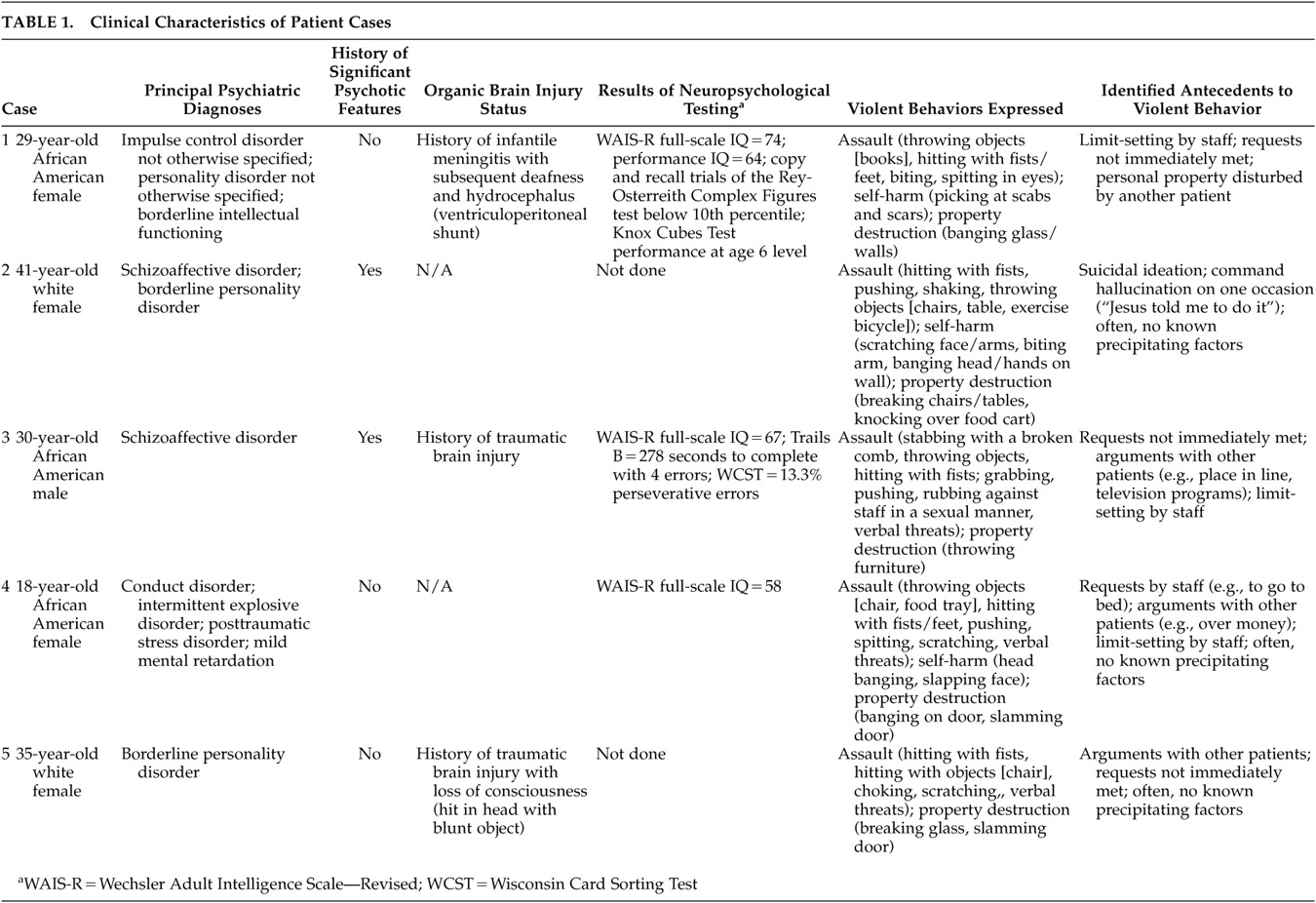
Table 1 provides further information on the clinical and behavioral aspects of these cases.
Case 1. Ms. A was a 29-year-old African American female who presented to the hospital from the county jail. The patient was sent to the hospital as she was deemed incapable of proceeding to trial due to her mental illness (charges were related to an assault). Her past history was remarkable for infantile meningitis which resulted in permanent neurological damage, including deafness and hydrocephalus (requiring ventriculoperitoneal shunting). The patient had four prior admissions to our hospital and had received an axis I diagnosis of impulse control disorder not otherwise specified and axis II diagnoses of personality disorder not otherwise specified (with antisocial and borderline traits) and borderline intellectual functioning. Wechsler Adult Intelligence Scale, Revised, revealed an IQ of 74. Psychological testing disclosed that the patient’s “intellectual and developmental functioning are significantly below average.” She had a long history of violent behavior, including multiple episodes of violence during prior hospitalizations. Indeed, during her last hospitalization, she had “brutally battered a sign interpreter to near unconsciousness.” She never reported psychotic features but had a history of treatment with multiple antipsychotics due to persistent aggression. Her medications at intake included divalproex sodium, clonazepam, haloperidol decanoate, and ziprasidone. Ziprasidone was dosed at 80 mg twice daily (the maximum recommended dose). In the 2 months prior to the initiation of clozapine, the patient displayed characteristic aggressive behavior including six episodes of assault against others, six episodes of self-injurious behavior, and six times where she required restraints for safety. She often required one-to-one observation. Three weeks into her admission, ziprasidone was discontinued and topiramate was begun; there was no significant benefit, and topiramate was subsequently discontinued. On the 58th day of hospitalization, because of persistent aggression, clozapine was begun. Ms. A had a rapid and sustained response to clozapine. While on clozapine, she had no further episodes of assault or self-injurious behavior, and there was no further need of seclusion or restraint. Her final total daily dose of clozapine was 275 mg with a serum level of 303. After 3 months of treatment on clozapine, she had been changed to routine observation, was participating in off-unit groups, and efforts were being made to have her legal charges dismissed so that she could be placed in a structured community setting.
Case 2. Ms. B was a 41-year-old white female who presented from an outside hospital secondary to exacerbation of her schizoaffective disorder and suicidal ideation. In addition to the axis I diagnosis of schizoaffective disorder, she carried a diagnosis of borderline personality disorder. The current was the third admission for this patient to our hospital, though she had multiple prior hospitalizations in the community. She had previously been treated with a variety of medications, including several conventional antipsychotics and the atypical antipsychotics risperidone, olanzapine, and quetiapine. Her prior admissions had been characterized by violent behavior, including an attempt to burn herself. The initial psychiatric assessment for the current admission was performed while the patient was “in seclusion, yelling and crying.” She appeared to be attending to internal stimuli and endorsed auditory hallucinations of “God calling me evil and bad.” Her medications at intake included quetiapine, venlafaxine, and, as needed, lorazepam and typical antipsychotics. Her hospitalization was greatly complicated by violent behavior, and she frequently required short-term transfer to the high-management crisis unit. The patient required one-to-one and, at times, two-to-one levels of observation. Several sequential pharmacological interventions were made in an attempt to decrease violent behavior, including valproic acid, chlorpromazine, haloperidol, droperidol, and ziprasidone. Nine months into her hospitalization, she attempted to harm herself by jumping off a balcony. In the 3 months prior to initiation of clozapine, she required seclusion or restraint 17 times, committed eight acts of assault, engaged in self-injurious behavior twice, and destroyed property three times. Her medications just prior to clozapine included divalproex sodium, clonazepam, haloperidol (30 mg/day total dose), and ziprasidone (160 mg/day total dose). Almost a year after her admission, haloperidol, ziprasidone, and divalproex sodium were tapered off and clozapine was begun. Ms. B had a rapid and sustained response to clozapine treatment. She no longer required seclusion or restraint, nor were there any further episodes of assault against others or self-injurious behavior. Her final dose of clozapine was 200 mg/day, augmented by haloperidol 15 mg/day. While on clozapine, her level of observation was changed to routine, she earned campus passes, and she participated in off-unit groups. After 3 months of clozapine treatment, Ms. B was given a 4-day pass to visit family during the Christmas holiday. After 6 months of clozapine treatment, Ms. B was discharged from the hospital and has remained in the community for more than 6 months.
Case 3. Mr. C was a 30-year-old African American male who presented to the hospital on petition secondary to medication noncompliance and aggression toward other clients at the group home where he had been living. Mr. C had been diagnosed with schizoaffective disorder in adolescence and had multiple prior hospitalizations. He was considered treatment refractory in that he had persistent delusions and thought disorganization even with optimal treatment. He had a prior trial of clozapine but did not have significant improvement in his positive symptoms of psychosis and was ultimately switched to a potentially less toxic medication. At the time of the current admission, his antipsychotic medications were haloperidol decanoate 100 mg intramuscular every 4 weeks, oral haloperidol 5 mg each evening, and ziprasidone 80 mg orally twice a day. For mood lability, divalproex sodium 1500 mg orally each evening had been prescribed. Mental status examination on admission was notable for paranoia (e.g., the medications were poison), delusions (e.g., the patient believing he was a psychiatrist and was married to a billionaire), disorganization of thought and behavior, and his attending to internal stimuli. He was also described as “slightly belligerent” and “uncooperative.” Early in his admission, Mr. C required forced medications due to persistent medication refusals. His ziprasidone was discontinued but haloperidol and divalproex sodium treatment continued. The oral dose was increased to haloperidol 5 mg twice a day, and haloperidol decanoate was increased to 150 mg every 4 weeks. Mr. C required seclusion and restraint on multiple episodes and had several transfers to a high-management crisis unit. Six weeks into his hospitalization, haloperidol was increased to 10 mg orally twice a day. Four months into his hospitalization, Mr. C still required episodes of forced medication secondary to noncompliance and aggressive behaviors. In the 3 months prior to clozapine treatment, he had nine episodes of violent behavior and required seclusion and restraint nine times. These episodes included hitting staff with a chair and attempting to stab staff with a broken comb. Coinciding with his violent behavior were increased sexual preoccupation and associated hypersexual behavior. Mr. C experienced penile soreness secondary to excessive masturbation. Just prior to clozapine treatment, Mr. C assaulted a nurse, grabbing her buttocks, pushing his body into hers “belly to belly,” and “grinding” his groin into her. Mr. C was again transferred to the high-management crisis unit and clozapine was started the following day, while haloperidol was discontinued. His final dose of clozapine was 175 mg/day with a serum level of 356. While on clozapine, he did not have further violent episodes nor did he require seclusion and restraint. He was able to leave the high-management unit and return to the general hospital population. Along with improvement in his violent behavior, his sexual preoccupation diminished greatly, and he was no longer medication noncompliant. Despite the improvement in these target behaviors, he remained delusional with moderate to severe thought disorganization. However, he improved enough behaviorally to be discharged to a group home in the community.
Case 4. Ms. D was an 18-year-old African American female who presented to the hospital under involuntary commitment after voicing suicidal ideation (“I tried to kill myself by running in front of a police car”). Ms. D had also been refusing her medication. She had been discharged from the hospital only 5 days before. The current represented the fourth admission to our hospital, but the patient had had multiple admissions to a number of other hospitals. She carried diagnoses of psychotic disorder not otherwise specified (due to infrequent reports of auditory hallucinations), conduct disorder, intermittent explosive disorder, and posttraumatic stress disorder (she had witnessed her mother being shot). Presentations to the hospital were usually preceded by aggressive behavior, suicidal ideation, and/or depressive symptoms. Ms. D had been followed by the community mental health center since age 6, and she required placement in an alternative school secondary to recurrent aggressive behavior. Eighteen months before the current admission, Ms. D was diagnosed with mental retardation, with a full-scale IQ of 58. Her medications at admission included risperidone (4 mg/day total dose), divalproex sodium (2000 mg/day dose), propranolol, clonazepam, and fluoxetine. Medications were used primarily to target persistently aggressive behavior as the patient denied any symptoms of psychosis. Early in her hospitalization, Ms. D had multiple episodes of aggression and at times required droperidol and restraints to control dangerous behaviors. In her first month of hospitalization, she required restrictive interventions 10 times and transfer to a high-management crisis bed. Because of her unpredictable behavior, she often required one to one observation. During the first 6 weeks of hospitalization, risperidone was titrated to a total dose of 12 mg/day without benefit. At 6 weeks, risperidone was discontinued and haloperidol 10 mg/day total dose was begun. At 12 weeks, the patient was again transferred to a high-management crisis bed, this time for 10 days. At 3 months, haloperidol decanoate 150 mg IM was given. At 4 months, haloperidol was discontinued due to adverse effects (galactorrhea), although Ms. D experienced relatively stable behavior while on this medication. Her aggressive behaviors again increased, including assault against a staff member and multiple occasions where Ms. D required restraint. At 5 months into the hospitalization, clozapine was begun and was ultimately titrated up to 150 mg with a serum clozapine level of 280. Ms. D had neither aggressive incidents nor behaviors requiring seclusion and restraint while taking the clozapine. Her guardian felt that Ms. D was doing “the best I’ve seen her in years.” Plans were made to discharge Ms. D to a group home. However, approximately 2 months after clozapine was started, it had to be discontinued secondary to an absolute neutrophil count of 1079. Ms. D did poorly after the clozapine was discontinued, and within 2 weeks she required restraints for aggressive behavior.
Case 5. Ms. E was a 35-year-old white female who presented to the hospital under involuntary commitment. She voiced suicidal and aggressive ideation, stating “I feel like I’m about ready to collapse.” The patient had 15 prior admissions to the hospital and had been discharged 15 days previously to a group home. Her medications on admission were risperidone (4 mg/day dose) and paroxetine. Ms. E’s primary diagnosis was borderline personality disorder, which was complicated by a history of closed-head injury. The patient had been in the hospital approximately 3.5 years prior to clozapine treatment. During these years, she displayed persistently violent behavior and required transfer to the high-management crisis bed on two occasions. Medication changes, including anticonvulsants and benzodiazepines, were not effective in controlling aggressive behavior. Trials of quetiapine and olanzapine were also ineffective. In the 3 months prior to clozapine, Ms. E had 16 episodes of property destruction, assaultive behavior to other patients and staff, and required restraints on several occasions. Due to persistently violent behavior, clozapine was begun at a total dose of 25 mg/day. Due to problems with orthostatic hypotension, the clozapine dose could not be titrated higher in the first 3 months of use. Despite the low dose, Ms. E’s behavior improved significantly. During the first month of clozapine use, she had 7 more episodes of violent behavior; these occurred primarily in the first 2 weeks following clozapine initiation. In the second and third month of clozapine treatment, there were no episodes of violent behavior. After 6 weeks of clozapine use, the patient was able to complete an overnight visit with family. After 8 weeks, she was able to successfully use a thrice weekly off-campus pass. At week 15 of clozapine treatment, she was discharged from the hospital to a group home. However, Ms. E returned to the hospital at week 16 after making threats at the group home. The patient denied aggressive intent, stating that her goal was to return to the hospital. On readmission, the physician described the patient as “appear[ing] to be happy to be back in the hospital.” Her clozapine was increased to 50 mg/day total dose, which Ms. E tolerated without adverse effect. Ms. E has displayed no episodes of violent behavior since readmission to the hospital, and attempts are currently geared toward finding an appropriate disposition in the community.
DISCUSSION
The main finding of this paper is that clozapine was effective in markedly decreasing the number of violent episodes in persistently violent patients, regardless of the underlying psychiatric diagnosis and even in the absence of psychotic symptoms. Indeed, only two of the five patients we described had a primary psychotic disorder. Our current findings are consistent with published reports of the antiaggressive properties of clozapine, although the populations in these earlier studies had psychosis and/or a primary psychotic disorder.
13–20 The rapidity with which clozapine treatment reduced significant violent episodes in our study was notable: four of the five patients had no further violent episodes immediately after treatment initiation. The fifth patient had no further episodes after 1 month of treatment. Chengappa et al.
13 have also demonstrated a rapid onset of clozapine’s antiaggressive effect in patients with schizophrenia or schizoaffective disorder. In their report, the number of seclusions per patient-month in a state psychiatric hospital was used as a proxy measurement of aggressive behavior. There was a significant and sustained reduction in seclusion within the first month following the initiation of clozapine treatment.
This rapid, antiaggressive effect of clozapine is in contrast to its antipsychotic effect, which may take several weeks to appear. Thus, the suggestion has been made that clozapine has specific antiaggressive effects not present in other antipsychotic agents.
11,18 This concept is supported by a double-blind, random assignment study comparing clozapine with olanzapine, risperidone, and haloperidol.
21 Clozapine had a significantly greater effect on the hostility item of the Positive and Negative Syndrome Scale than did haloperidol or risperidone and was the only antipsychotic to show superiority to haloperidol. Olanzapine and risperidone were not significantly different from haloperidol in this regard.
21 Our own clinical experience with the patients described in the present report suggests the superiority of clozapine over other antipsychotics in the treatment of aggression. All of the patients had trials of both typical and atypical antipsychotics that were either ineffective or only partially effective in the treatment of violent behavior. The use of ziprasidone in three of the five patients immediately prior to clozapine was not merely a coincidence; rather, these patients had failed all other atypical antipsychotics (save for clozapine), and ziprasidone had just been approved for use at the time of the study period. Therefore, in these cases, ziprasidone was used as a final agent prior to clozapine in these difficult to manage patients. Work by Meltzer and colleagues in the InterSePT study
22 adds further weight to the argument that clozapine has distinct antiaggressive properties. Here, clozapine was found to be superior to olanzapine in the prevention of self-aggression (i.e., suicide) in a cohort of patients with schizophrenia. This finding resulted in the recommendation that the U.S. Food and Drug Administration approve clozapine for the treatment of schizophrenia patients who display suicidal behavior.
Although speculative, the treatment with a single agent (clozapine) for a specific target symptom (violent behavior) in a group of patients with diverse diagnoses (mental retardation, impulse control disorder not otherwise specified, borderline personality disorder, schizoaffective disorder, intermittent explosive disorder, and organic brain injury) suggests that the neurobiological mechanism of aggression may possibly be the same across these patients despite their other psychiatric differences. The biological vulnerability to persistent violence may represent a disorder comorbid with other psychiatric disease (e.g., schizoaffective disorder, personality disorder) or a disorder unmasked by brain injury. Conceptualizing the need for the treatment of an “aggression disorder” independent of that of other comorbid disorders may be a useful strategy, particularly for persistently violent patients. For example, although Ms. B (case 2) had resolution of hallucinations with several antipsychotic agents, only clozapine effectively treated her violent behavior. Of interest, she had just one episode of violence that could be directly related to psychotic symptoms (command hallucination) (
Table 1). In contrast, Mr. C (case 3) remained with significant positive symptoms of psychosis, even though his aggressive behavior resolved with clozapine treatment. Importantly, none of his episodes of violence during the study period were related to antecedent psychotic symptoms (
Table 1). Thus, the identification and specific treatment of persistently aggressive behavior, regardless of diagnosis, become important objectives.
There are several limitations to this study, including the open, retrospective nature of the data collection and identification of persistently violent patients treated with clozapine. The majority of studies evaluating clozapine’s effect on aggression have been open and retrospective,
11 probably due to the severe psychopathology of these patients who ultimately require treatment with clozapine (i.e., informed consent for a prospective study would be difficult). The one randomized, double-blind trial
21 examining the effect of clozapine on hostility supports the conclusion from the open studies that clozapine is an effective antiaggressive agent. Although a well-designed study, these patients were not selected specifically due to violent behavior.
Another weakness is that the current study examined the effect of clozapine on only a small number of patients, though the effect was fairly dramatic (
Figure 1). The main reason for the small number of patients was the stringency of the inclusion criteria. Events considered significant were violent episodes that resulted in incident reports and/or the need for seclusion or restraint. Because of the inclusion criteria, patients with chronic “subthreshold” violent behavior could not be included. However, we chose these criteria such that an objective measurement was available as a proxy of violent behavior. Using these measurements, a determination of the effect of clozapine on violent behavior could be made. The authors were aware of approximately one dozen other patients for whom clozapine had a beneficial effect on violent behavior but for whom objective data of this effect were not available. Our review of individual patients revealed that save for significant violent events that resulted in assault or property damage, objective data documenting lower levels of aggressive behavior were lacking. Descriptive, narrative data were minimally helpful at best. As a consequence, we now complete the Overt Aggression Scale
23,24 for patients where aggression is or may be a concern. We anticipate that routine use of the Overt Aggression Scale will allow us to more readily identify persistently violent patients and to more specifically track responses to treatments, both pharmacological and psychosocial.
The use of incident reports is also a weakness, as these may not always be filled out by hospital staff as required.
25,26 However, our data and that of others suggest that staff is more likely to report the more significant violent events. The cases that we reported on were all well-known “notorious” patients that usually were on high levels of observation and were watched very closely by staff.
A fourth weakness of the paper is that all patients discussed in the cases were on several different pharmacological agents. Chief among these were mood stabilizers, benzodiazepines, and other antipsychotics. This polypharmacy represents the “real world” treatment of severely, persistently mentally ill patients who have multiple target symptoms (mood lability, anxiety, psychosis, etc.). However, the dramatic effect on violent behavior with the introduction of clozapine, where earlier drug therapies had failed, suggests a specific effect of clozapine. Likewise, the relapse to violent behavior following withdrawal of clozapine in Ms. D (case 4) further strengthens the role of this drug in controlling her aggression.
In conclusion, the current report adds to the growing body of literature suggesting that clozapine has a specific antiaggressive effect distinct from its antipsychotic effect. Our case series demonstrating that clozapine effectively reduces violent behavior in a heterogeneous diagnostic group further suggests that aggression may have a similar neurobiological substrate regardless of diagnosis, and may indeed represent a specific “aggressive” disorder. Given that aggression may require distinct pharmacological treatment, a trial of clozapine with the use of objective measurements of aggression to gauge treatment response (e.g., the Overt Aggression Scale) should be considered for persistently violent patients.