Three computerized executive tests were administered. 1) A computerized version of the Tower of London Planning Task,
6 which requires subjects to plan and execute a series of moves in order to change the position of balls hanging in billiard pockets to match a goal arrangement, was administered. The number of required moves on each trial varies between 3 and 5. The measure is the number of solutions (out of 12) solved in the minimum number of moves (perfect solutions). 2) A decision making task
7 in which subjects decided whether a token was hidden in a blue or red box was also administered. Subjects were given “odds” information (9:1, 8:2, 7:3, 6:4) to guide them. On each of 72 trials, they could also gain or lose points by betting according to their certainty of making a correct choice. The measures were the percent trials in which they chose the correct box (quality) and the percent accumulated points bet at each odd (risk). 3) A gambling task
4 in which subjects selected a card from one of four decks on each of 100 trials was administered. Each card turn was rewarded with points, but some cards subsequently demanded a penalty forfeit of points. The decks were arranged so that the cards in two of the decks resulted in higher points than cards in other decks, but they extracted higher penalties and were disadvantageous compared to the “good” decks in the long term. Memory was assessed using a computerized paired associates test.
8 Subjects needed to learn the position of six or eight patterns presented on the screen one at a time. They were reminded of their mistakes and had up to 10 attempts to correctly recall the position of each pattern. Measures were total number of errors (learning) and number of pattern location recalled correctly at the first attempt (memory). All subjects completed the computerized tasks except the decision making task, which was completed by all comparison subjects and 16 patients. Intelligence quotient (IQ) was estimated using the National Adult Reading Test,
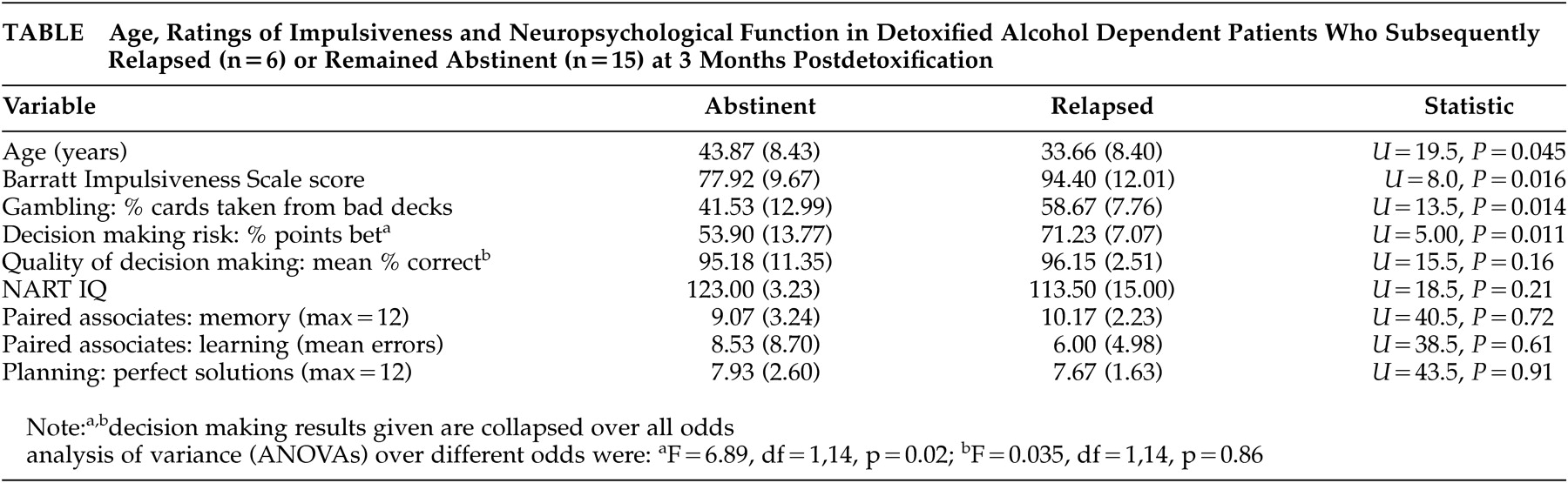
9 which was completed by 18 comparison and 16 patients. Other measures were: the Structured Clinical Interview for DSMIII-R, antisocial and borderline subscales; the Brief Psychiatric Rating Scale (BPRS); the Addiction Severity Index (ASI), which was completed by all patients; the Barratt Impulsiveness Scale (BIS) (34-item),
10 (
see Table) which was completed by 18 patients and 19 comparison subjects; and the Dimensional Assessment of Personality–Basic Questionnaire (DAPP-BQ),
11 completed by 20 patients and all comparison subjects.
Because of small numbers, group differences were analyzed using the Mann-Whitney U Test, except the decision making task, which was analyzed using analysis of variance (ANOVA) due to repeated measures. All probabilities are two-tailed.