General paresis is a clinical type of late-stage syphilis and neurosyphilis. Symptoms vary among patients and there is no gold standard to diagnose at present. Diagnosis of general paresis depends on clinical evaluation, serologic testing, and CSF examination. The criteria for diagnosis of neurosyphilis recommended by the Centers for Disease Control and Prevention is as follows: CNS or ophthalmic signs or symptoms; serologic evidence (positive nontreponemal and positive treponemal test results) for syphilis infection plus either positive venereal disease research laboratory CSF, increased CSF protein (>40 mg/dl), or increased CSF leukocyte count (>5 mononuclear cells/μL).
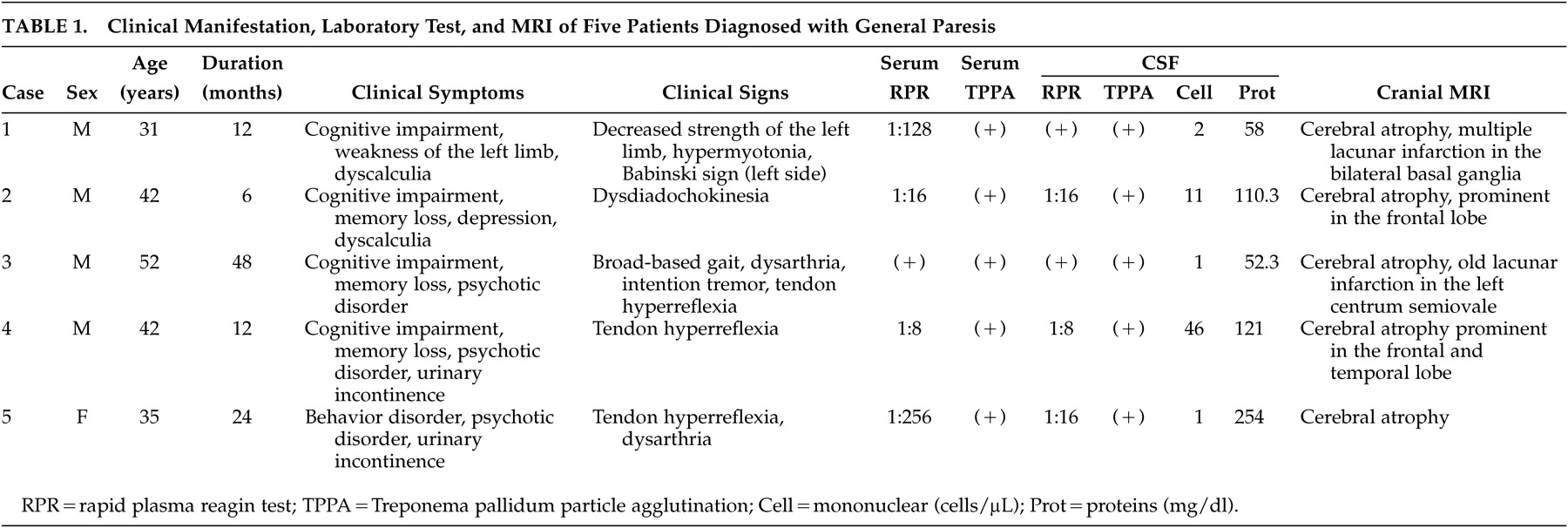
1 All five patients met the diagnostic criteria for general paresis. Clinical indications of the five cases were similar to those reported in recent literature, mainly exhibiting cognitive impairment, psychotic disorder, memory loss, and tendon hyperreflexia. There were two patients who displayed urinary incontinence, which is rarely reported in general paresis. Yet it can be seen in tabes dorsalis and may have hypocompliant detrusor hyperreflexia with detrusor-sphincter dyssynergia and postmicturition residual urine.
2 The cranial MRI of Case 1, who exhibited hemiparalysis, revealed both acute and old lacunar infarction in the bilateral basal ganglia. The 31-year-old patient presented with hemiparalysis after 1 year of cognitive impairment, so we inferred that the patient might have general paresis combined with meningovascular syphilis. Case 3 exhibited old lacunar infarction without related symptoms. The infarction could also be seen in general paresis in Kodama et al.’s
3 report. The longer the clinical course is, the more complicated the clinical manifestation and unfavorable prognosis. For example, Case 3, with 4 years of clinical course, presented with not only cognitive impairment and psychotic disorder, but also cerebellar signs such as intention tremor, broad-based gait, and glossopharyngeal paralysis. The cranial MRI revealed cerebral atrophy, primarily in the frontal and temporal lobe. It was reported that medial temporal lobe atrophy may be a poor prognostic sign in general paresis.
3 In this patient, the personality change and general dementia remained after the complete penicillin G treatment, and the outcome for social function was poor. After the patient was treated with intravenous penicillin G for 14 days, the basic medical examination, neurological examination, and intelligence testing were the same as during original hospitalization. The cranial MRI performed in all five cases showed cerebral atrophy. The neuroimages of neurosyphilis generally are not very specific and thus of little value in making a diagnosis. SPECT has been employed to study cases of general paresis
, as well as other natural mental disorders. The results of previous studies regarding the relationship between clinical status and CBF changes are still ambiguous. After 15 days of penicillin G treatment, the clinical symptoms had remitted, and laboratory results were improved, but the CBF still decreased. Kitabayashi et al.’s
4 study suggested that in cases of general paresis, rapid marked decrease of quantitative CBF counts after penicillin treatment reflects the disappearance of encephalitis. Moreover, their slow recovery over 1 year reflects the gradual improvement of IQ and overall level of function.
4 EEGs performed on four of the patients, three of whom had abnormal EEG manifestation, mostly revealed generalized arrhythmic slow activity. It is not specific and can be also seen in other diseases.
General paresis, the encephalitic form of neurosyphilis, typically presents as progressive dementia beginning 15–20 years after original infection (range 3–30 years). The clinical features of general paresis may include cognitive impairment, delusional or apathetic states, dysarthria, myoclonus, intention tremors, seizures, hyperreflexia, and Argyll Robertson pupils.
5 After a decade of decline, rates of primary and secondary syphilis again began to rise in the United States in 2001.
6 The increasing incidence among men who have sex with men in major cities accounted for the overall increase in incidence.
7 In San Francisco, the increased incidence in early syphilis has been accompanied by increasing rates of neurosyphilis,
8 and HIV infection also increases the risk of neurosyphilis.
9 Similar trends have also been observed in Canada and Europe.
10 At present, it is not known how many of those infected in recent syphilis outbreaks may go on to general paresis. A recent study showed that general paresis accounted for 25.6% of the 43 immunocompetent patients with neurosyphilis.
11 It is quite possible that the incidence of general paresis might also increase correspondingly with the increased incidence of primary and secondary syphilis. In China, since the sexually transmitted diseases (STDs) were recognized as a public health problem during the early 1980s, the incidence of syphilis has gradually increased.
12 General paresis increased correspondingly. The latter is considered to be a “treatable” dementia because it can be treated with antibiotics, mainly penicillin.
13 However, early diagnosis and treatment are very important.
Sexually transmitted diseases were common before and during the early period of the foundation of the People’s Republic of China in 1949. They were virtually eliminated across the country by 1964,
14 but reform and opening-up policies that started in 1978 have rapidly changed the situation, especially in the past 15 years. The number of STD cases reported has been increasing significantly since then. Similarly, syphilis incidence increased approximately 20 times during 1989 to 1998, at an average annual increase of 52.7%.
12 This introduced a big health risk for the population and has been noticed by Chinese and foreign health researchers. General paresis should be seriously considered as one of the most severe outcomes of syphilis by doctors. If there is cognitive dysfunction or cerebral atrophy of unknown cause, general paresis should be considered.