This systematic review aimed to investigate CBT-related neurobiological changes in anxiety disorders, detected through neuroimaging techniques, and to identify predictors of response to treatment. By gathering results of studies on the new findings in the area, we can eventually contribute with knowledge for the increase of therapy efficacy, either through the improvement of new therapeutic strategies or through the potentialization with drugs that facilitate the basic mechanisms of action. The understanding of the underlying neurobiological mechanism can eventually aid in the choice of the most indicated treatment for a particular patient.
METHODS
An electronic search was carried out on January 26, 2007, in the following databases: PubMed, PsychInfo, and Web of Science. The search strategies used are available upon request. Searches were also performed from the references of the systematic review articles on neurobiological changes and psychotherapy.
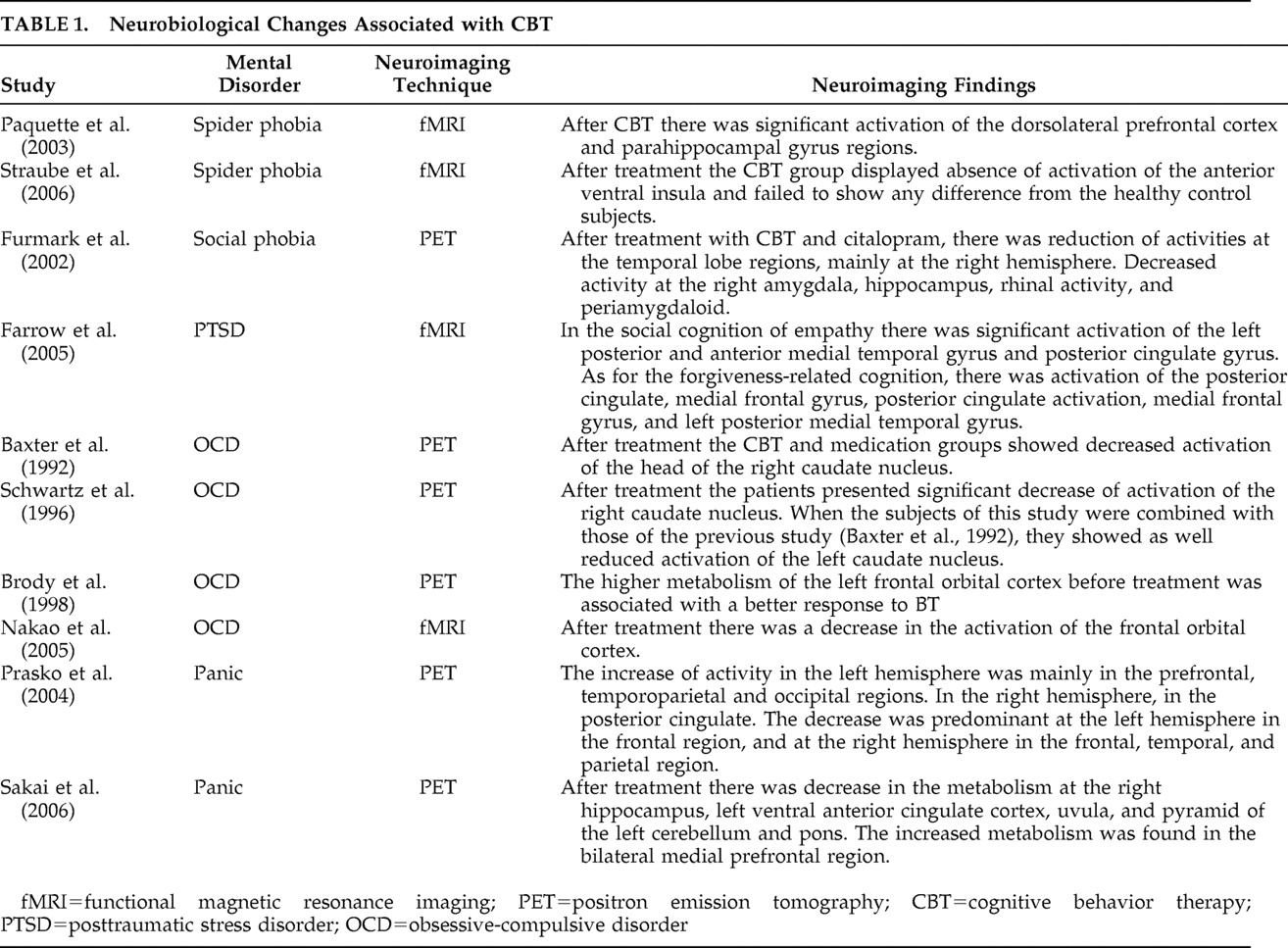
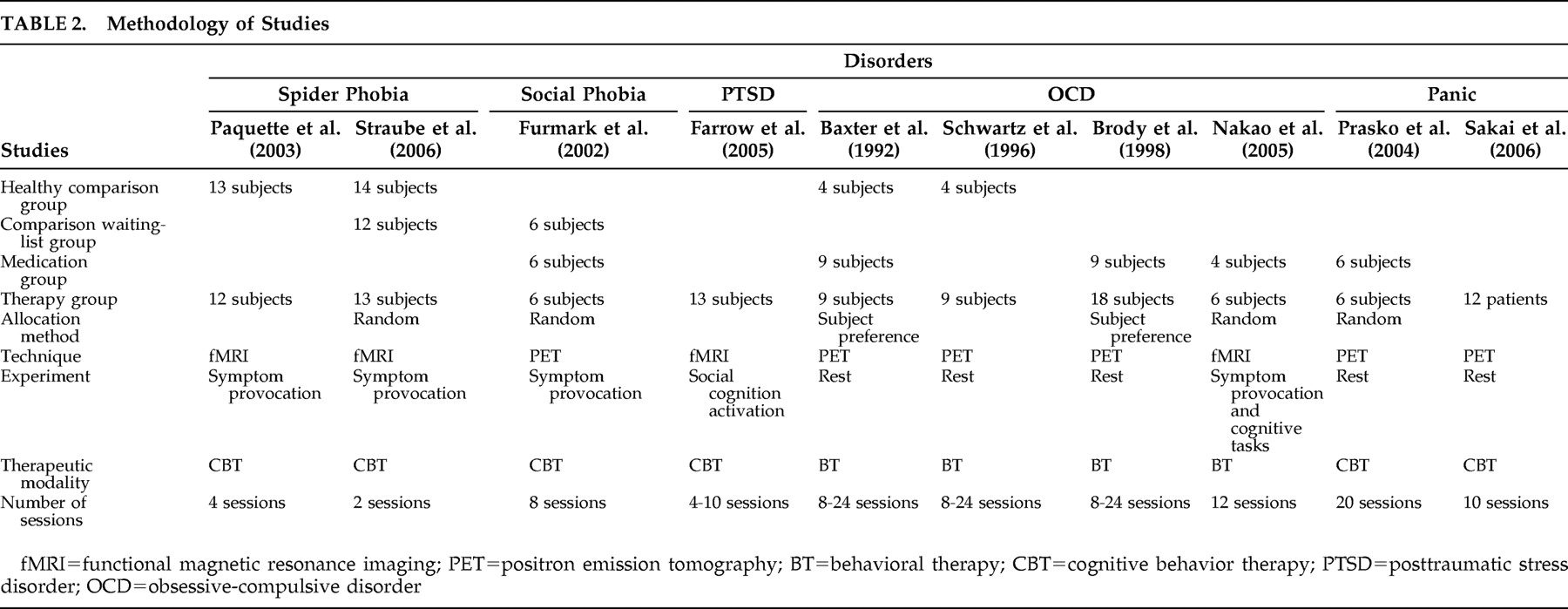
We included studies that evaluated neurobiological changes due to CBT through neuroimaging techniques and studies that involved adult patients with anxiety disorders. We excluded studies that used concomitant treatment besides CBT in the same sample of patients. Moreover, articles that dealt with subclinical anxiety were excluded. The outcome measures studied were the neurobiological changes resulting from CBT, assessed through neuroimaging techniques. Thirteen studies were found: five on patients with obsessive-compulsive disorder (OCD), three on posttraumatic stress disorder (PTSD), two on specific phobia, two on panic disorder, and one on social phobia. No studies were found for generalized anxiety disorder. Three studies were excluded because the patients were treated concomitantly with psychotherapy and medication (one from the OCD group and two from the posttraumatic stress disorder group). Thus, 10 articles met the selection criteria of this systematic review.
CONCLUSION
This systematic review aimed to investigate CBT-related neurobiological changes in anxiety disorders, detected through neuroimaging techniques, and to identify predictors of response to treatment. Although the number of studies considered in this review is small, they demonstrate that CBT is able to modify the dysfunctional neural activity related to anxiety disorders in the patients who responded to treatment. Such result confirms previous reviews of psychotherapy and neuroimaging,
1,
2,
4,
5 but the present review differs from the previous ones as it focus solely on CBT and anxiety disorders.
The studies by Straube et al.
11 and Furmark et al.
12 included in their methodology the randomization of patients for CBT and waiting-list group, thus evidencing that the neurobiological changes in the therapy group were a result of the CBT interventions rather than an effect of the passing of the time. The neuroimaging findings in studies by Paquette et al.,
10 Baxter et al.,
15 and Schwartz et al.
16 revealed that after treatment the patients presented activation similar to healthy comparison subjects.
As for the second aim of this review, the identification of treatment response predictors, Brody et al.
20 reported important results. They showed that OCD patients with particular patterns of brain metabolism can respond preferentially to a particular type of treatment. This is because the patients who responded to behavioral therapy presented a higher metabolism at the left frontal orbital cortex before the treatment. On the other hand, the lower metabolic activity at the left frontal orbital cortex was associated with better response to fluoxetine treatment. It should be highlighted that only one study was found concerning response prediction. The lack of studies about response prediction highlights the importance of future research in this area. The identification of treatment response predictors has great clinical importance, as knowledge of the pretreatment brain metabolism can eventually aid in the choice of the most indicated intervention for a given patient.
A particularly interesting aspect of the present review concerns the neuroimaging findings resulting from CBT treatment versus medication, revealing a common way of brain modification. Therefore, it suggests that psychotherapy with CBT and drug therapy may act in similar brain circuits.
12,
15,
18 Furmark et al.
12 pointed that the neural regions related to treatment with citalopram and CBT in social phobia converge to the amygdala, hippocampus, and adjacent cortical areas, and possibly mean a common way in the successful treatment of social anxiety. Baxter et al.
15 detected increased glucose metabolism in the right caudate nucleus in patients with OCD. After treatment with fluoxetine and behavioral therapy, the neuroimaging studies revealed decreased activity at this region in both treatments. Finally, Prasko et al.,
18 studying patients with panic symptoms, concluded that treatment with CBT and with antidepressants can activate the cortical temporal processing.
The study by Farrow et al.
13 stands out because of its distinct methodology. It proposed to identify the brain areas involved with social cognition in PTSD patients—specifically, the ability to forgive and experience empathy—and found attenuated activation of the related areas with the referred cognitive processes. It may be speculated that numbing symptoms related to the group could impair such abilities as empathy and forgiveness, as the individuals have difficulty feeling such emotions as intimacy and tenderness and feel disconnected from themselves. The study by Farrow et al.
13 showed that CBT can help in the remission of PTSD symptoms as well as promote the activation of brain areas related to social cognition of empathy and forgiveness. In their meta-analysis study, Etkin and Wager
21 underscore that PTSD is a more complex disorder than the other anxiety disorders, specifically social and specific phobia. This is because the patients with PTSD displayed a pattern of activation and hypoactivation that differed from those of other pathologies. The results revealed more frequent hyperactivity in the insula and amygdala in patients with social and specific phobia than in PTSD patients. Also, only patients with PTSD displayed hypoactivation of the dorsal and rostral anterior cingulate cortex and medial prefrontal cortex. For the authors, PTSD may be related to a dysfunction in the system of emotional regulation in which fear by itself is only an element of this system, while social and specific phobia would be related to a stage of intense fear and therefore would present greater activity of the insula and amygdala.
It should be mentioned that the heterogeneity of the studies presented here limits the possibility of direct comparison (
Table 2 ). In many of them, such as Baxter et al.,
15 Schwartz et al.,
16 and Brody et al.,
20 although the therapeutic modality was referred to as behavioral therapy, in the description of strategies there was reference to cognitive techniques, suggesting that it was CBT. The different number of sessions also made it difficult to compare them. The neuroimaging methods in the studies were also different, as four studies used fMRI and six used PET. Other considerations must be made as for the methods of the studies. Some studies used control groups while others did not. For evaluation of neurobiological alterations, three types of experimental paradigms were used—symptom provocation, cognitive tasks performance, and testing at rest. Most importantly, all the reviewed studies are small in sample size. This limitation restricts statistical power, enhances false negative results, and therefore has limited generalizability. To elucidate differences in brain changes resulting from cognitive behavior therapy, a larger number of patients must be examined before and after treatment. Further studies in this area need to be undertaken. Nakao et al.,
17 for instance, carried out a study with OCD patients, where the patterns of brain activation resulting from the comparison between behavioral therapy and fluvoxamine could not be statistically analyzed separately, due to the small number of participants. However, Schwartz et al.
16 combined results from a previous study
15 and were able to replicate the original findings. Despite these acknowledged limitations, it can be concluded that CBT may indeed promote neurobiological changes.
The investigation of changes in brain activity resulting from therapy is a new area of research which has major implications for better understanding the mechanisms of formation and maintenance of symptoms. Moreover, they can help reveal the biological mechanisms associated with the improvement of symptoms due to successful CBT treatment. After an analysis of studies we could propose plans for the performance of new clinical trials which can answer questions on neurobiological changes and psychotherapy. The methodology of studies should include randomized comparison groups for waiting list and a placebo group. We would thus have more evidence that the brain changes that occurred would be due to interventions with psychotherapy.
While Etkin and Wager
21 in their meta-analysis of structures related to disorders of specific and social phobia and PTSD found a common route for anxiety that would be the hyperactivation of the amygdala and insula, in the present systematic review we did not find such a model of activation. Possibly, this different result is related to the small number of studies that met the criteria for our review. Consequently, the inconsistency of results indicates the need for future research. However, the studies included in our systematic review pointed out in their neuroimaging findings structures that participated both in the brain circuits involved with extinction and in those involved with cognitive regulation of emotion. The results showed that CBT especially regulated the dysfunctional neural circuits involved with the regulation of negative emotions and fear extinction.
The literature shows that many mental disorders are involved with the inability to control fear
22,
23 and difficulty in regulating negative emotions.
24,
25 These data suggest that the conditioning of fear and the difficulty in regulating emotions play a major role in the formation and maintenance of anxiety disorders. Mocaiber et al.
24 highlight the research on neural circuits of extinction which has an important clinical implication. This is because anxiety disorders are in part characterized by resistance to the extinction of emotional reactions to anxiogenic stimuli and by avoidance behaviors.
It is important to highlight that CBT treatment contains specific techniques (exposure, distraction, and cognitive restructuring) which allow both the extinction of conditioned fear and the cognitive regulation of emotions.
Cognitive behavior therapy has proved to be effective in the treatment of various mental disorders, although the neurobiological effects of its action are little known. CBT favors the restructuring of thought, modification of feelings and behaviors, and promotes new learning. Consequently it involves synaptic changes.
26 This review had the aim of identifying the studies that have proposed to understand the brain alterations resulting from CBT. The investigation of changes in brain activity resulting from successful CBT treatment allows us to clarify the neural substrates underlying psychotherapy.
Neuroimaging studies provide a means to observe and characterize changes in brain functioning related to psychological and pharmacological interventions. Consequently, to understand how individuals process a stimulus can be an important piece of information for therapeutic response.
4The neuroscientific findings associated with the neuroimaging studies can enhance our knowledge of the neurobiological foundations of psychotherapies, as well as improve interventions in order to increase treatment efficacy.