Individual Findings
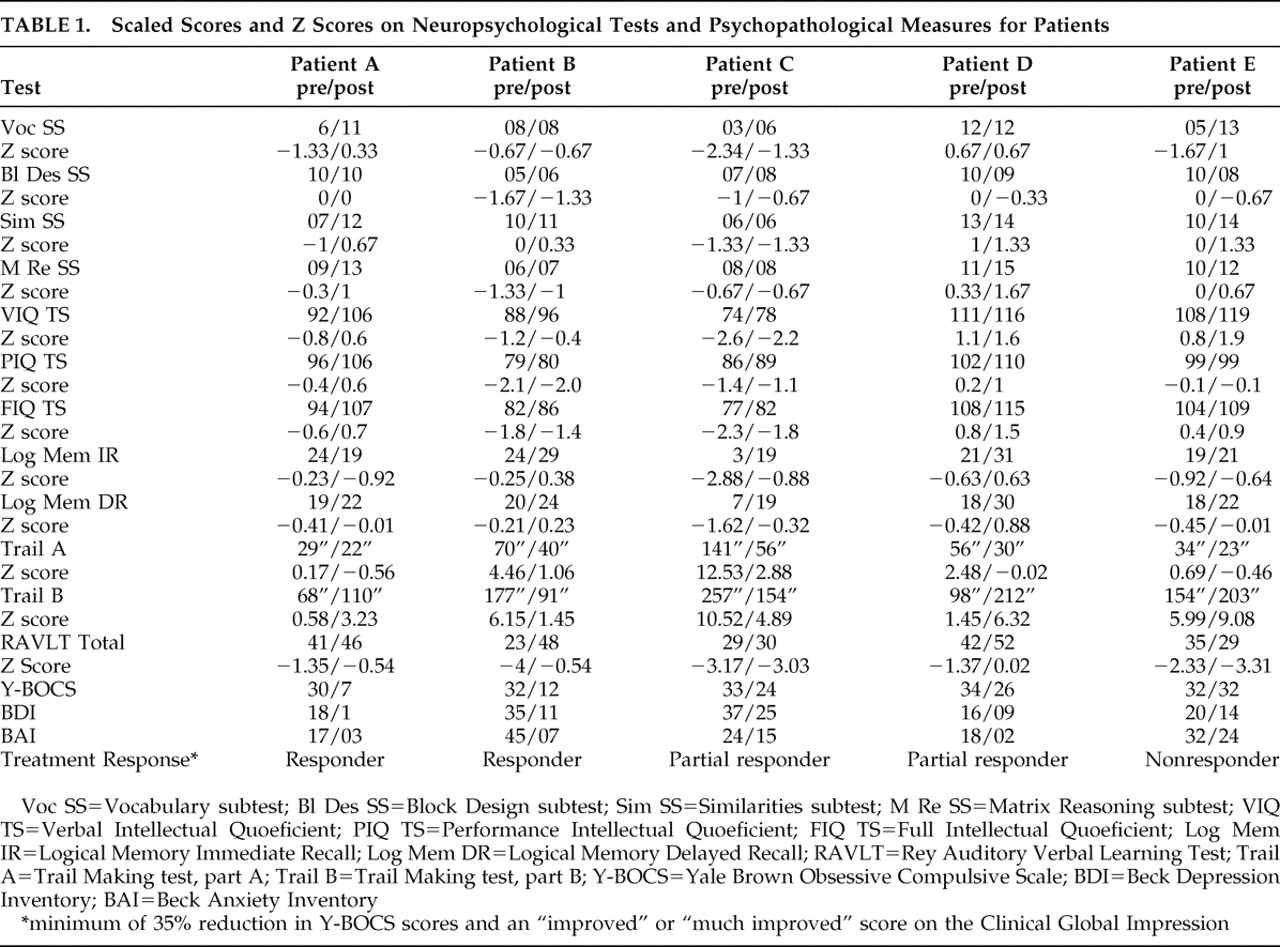
Table 1 shows the scaled scores and z scores on neuropsychological tests and psychopathological measures for the five patients submitted to ventral capsular/ventral striatal gamma capsulotomy.
Patient A, a 23-year-old man, met our response criteria and was still a responder 3 years after the procedure. Postoperatively, his Y-BOCS, BDI, and BAI scores decreased, suggesting improvement in obsessive-compulsive, depressive, and anxiety symptoms. He performed better on measures of full IQ, mainly due to improved performance on Vocabulary and Similarities subtests, and was slower on the Trail Making test, part B (divided attention).
Patient B, a 42-year-old woman, met our response criteria and was still a responder 3 years after the procedure. The psychopathological scale results suggested postoperative improvement in obsessive-compulsive symptoms, depressive symptoms and anxiety symptoms. She scored higher for sustained and divided attention (Trail Making test, parts A and B) as well as for verbal learning (Rey Auditory Verbal Learning Test).
Patient C, a 49-year-old woman, responded partially after 12 months. Clinically, the obsessive-compulsive symptoms presented a variable course, with minimal improvements in the depressive and anxious symptoms. In the third month of follow-up treatment, she was briefly hospitalized due to severe depressive symptoms. She improved in the second year and was still a responder 3 years after the procedure. At 12 months after the procedure, she performed better on attention measures, the Vocabulary subtest and memory tests (recall of contextualized information).
Patient D, a 36-year-old woman, responded partially after 12 months and was still a partial responder 3 years after the procedure. Although presenting only minimal improvements in her Y-BOCS score, her BDI and BAI scores increased 7 points after 12 months and 14 points after 9 months, respectively. She also improved on the sustained attention test, nonverbal reasoning (Matrix reasoning), memory, and learning scores. Nevertheless, her divided attention score dropped.
Patient E, a 25-year-old man, did not respond after 12 months and was still a nonresponder 3 years after the procedure. By postoperative month 6, his BDI score had dropped by 10 points, although his Y-BOCS score was unchanged, and after 3 months of treatment, his anxiety symptoms improved significantly, remaining constant for 2 years after the procedure. No obsessive-compulsive symptom improvements were observed, even when intensive inpatient CBT was administered during the second year of follow-up treatment. Although sustained attention, verbal IQ, vocabulary, similarities and recall of contextualized information improved, divided attention score and learning (total words recalled on the Rey Auditory Verbal Learning Test) worsened.
Group Findings
Intellectual Functioning
Although overall intellectual performance improved for the entire group, only one patient met our criteria for improvement. On the Vocabulary subtest, three patients demonstrated greater expressive vocabulary and answers that were more objective and “straight to the point,” as well as presenting fewer hesitations. Two patients (A and E) scored higher on the Similarities subtest, suggesting improved abstract verbal reasoning ability. On the Matrix Reasoning subtest, two patients (A and D) performed better, and three (patients B, C, and E) maintained the same results. There were no changes in the Block Design test results.
Attention
Postoperatively, four patients scored higher for sustained attention, completing the task faster, whereas three scored lower for divided attention.
Learning Abilities
Total words recalled on the Rey Auditory Verbal Learning Test increased in two patients (B and D), decreased in one (E), and remained unchanged in two (A and C).
Amnestic Functions
Recall of contextualized information (immediate and delayed recall) improved in two patients (C and D).