POSTER SESSION, MARCH 24, 2011, 3:45–5:15 PM
P1. The Relationship Between Cognitive Impairment and Placebo Response
C. Alan Anderson, M.D. Caitlin Dufault, M.D. David B. Arciniegas, M.D.
Background: The effect of cognitive impairment on placebo response is not understood fully. This information is needed to design and interpret treatment studies in cognitively impaired populations, including those with Alzheimer's disease. Objective: To evaluate the relationship between cognition and placebo response among subjects with Alzheimer's disease (AD) or mild cognitive impairment (MCI). Methods: Published placebo-controlled clinical trials evaluating pharmacotherapies for MCI or dementia due to AD were reviewed. Studies in this analysis included ≥ 30 placebo subjects in which baseline Mini-Mental State Exam (MMSE) scores (to stratify AD severity) and placebo-related changes in Alzheimer's Disease Assessment Scale - Cognitive Subscale (ADAS-Cog) scores were reported. These data were used to test the hypothesis that baseline ADAS-Cog score (covaried with treatment duration) predicts change in ADAS-Cog score in response to placebo treatment. Results: The model (baseline ADAS-cog score and treatment duration) was significant (F = 6.82, p <0.01), and accounted for 43.7% of the variance in ADAS-Cog scores following placebo treatment. Both predictor variables contributed significantly to the model. Baseline ADAS-Cog score alone accounted for 41.1% of the variance in placebo-related change in ADAS-Cog score (F = 9.10, p <0.01). Relative preservation of cognition at study entry (i.e., higher baseline ADAS-Cog score) was associated with larger placebo effects. Conclusions: Severity of cognitive impairment at baseline influences the degree of placebo effect, reflected in these studies as cognitive improvement and/or stabilization. Implications of this finding on clinical trial design and interpretation are discussed.
P2. Mini-Mental State Exam and Frontal Assessment Battery Scores Predict Inpatient Rehabilitation Outcomes After Traumatic Brain Injury
David B. Arciniegas, M.D., Kimberly L. Frey, M.S., CCC-SLP, Hal S. Wortzel, M.D., Peter J. Wagner, M.D., Jody Newman, M.A., CCC-SLP, C. Alan Anderson, M.D.
Background: Physicians are often called upon to opine on the relationship between early posttraumatic cognitive impairments and inpatient rehabilitation outcomes. The value of commonly used bedside cognitive assessments, including the Mini-Mental State Exam (MMSE) and Frontal Assessment Battery (FAB), for this purpose remains under-explored in this population. Objective: To evaluate the MMSE and FAB, independently and combined, as predictors of: 1) rehabilitation length of stay (RLOS); 2) Functional Independence Measure (FIM) score proximate to neuropsychiatric consultation; and 3) discharge FIM score. Methods: Medical records of 83 inpatients consecutively evaluated on a brain injury rehabilitation unit were retrospectively reviewed. Inclusion criteria were: TBI (non-penetrating) by American Congress of Rehabilitation Medicine criteria; age 20–89 years; primary language English; non-aphasic; neuroimaging demonstrating intracranial abnormality consistent with TBI. Data extracted from records of eligible subjects included: demographic information; TBI mechanism; MMSE, FAB, and FIM scores; and RLOS. Multiple regression modeling was used to investigate the proportion of variance in FIM scores and RLOS accounted for by MMSE and/or FAB Z-scores. Results: Fifty-five subjects were included. MMSE and FAB Z-scores independently predict RLOS and FIM at consultation and discharge. The combination of these measures accounted for a greater proportion of variance in all models than did either measure alone. Conclusions: Normatively interpreted MMSE and/or FAB scores inform usefully on duration of inpatient rehabilitation hospitalization as well as functional status proximate to consultation and inpatient rehabilitation discharge. Prospective study of these measures as predictors of short- and long-term rehabilitation outcomes in this population is warranted.
P3. Neuropsychiatric Sequelae of Hypoxic-Ischemic Brain Injury: A Pilot Study
Beatriz Castaño, M.D., Alberto García-Molina, M.Sc., Montserrat Bernabeu, M.D., Teresa Roig-Rovira, Ph.D., David B. Arciniegas, M.D.
Background: Hypoxic-ischemic brain injury (HI-BI) is a common consequence of conditions that compromise cerebral oxygenation, cerebral perfusion, or both. However, few studies describe the neuropsychiatric sequelae of HI-BI. Objective: To describe the neuropsychiatric characteristics of a pilot sample of persons with HI-BI evaluated at a neurorehabilitation center. Methods: Medical records of 20 individuals (10 inpatients, 10 outpatients) with HI-BI were reviewed retrospectively. Demographic, clinical, and neuropsychological data, as well as Glasgow Outcome Scale ratings were extracted. A population-specific adaptation of the 12-item Neuropsychiatric Inventory guided neuropsychiatric symptom identification. Results: Subjects were 41 ± 11 years of age and 26.9 ± 46.2 (median = 6) months post-injury. Injury causes included cardiovascular events (80%), respiratory compromise (15%), and hypovolemia (5%). Disturbances of orientation (90%), verbal memory (85%), visuoperceptive abilities (50%), attention (45%), language (45%), and praxis (20%) were observed. Apathy was predominant neuropsychiatric symptom (85%). Irritability, sleep disturbances, anxiety, emotional lability, restlessness, depression, and aggression occurred in ≥ 40%. Aberrant motor behavior, impulsivity, agitation, appetitive disturbances, disinhibition, visual hallucinations, and delusions were present in ≤30%. Five general profiles of neuropsychiatric disturbances were observed: 1) apathetic; 2) depressive; 3) aggressive-impulsive; 4) anxious-labile; and 5) agitated-psychotic. Cognitive-neuropsychiatric correlations included: 1) attention and language impairments with apathy; 2) verbal memory impairments with emotional lability and delusions; 3) orientation disturbances with irritability; and 4) apraxia with depression. Conclusion: Neuropsychiatric symptoms are common subacute and late consequences of HI-BI. Prospective studies of the types and functional implications of neuropsychiatric symptoms in this population are needed.
P4. Initial Treatment Retention in Psychogenic Non-Epileptic Seizures
Gaston Baslet, M.D., Eric Prensky, M.D., Angela Roiko, M.D., Amanda Uliaszek, M.D., Pavan Prasad, M.D.
Background: Treatment referrals to psychiatrists and psychologists are common practice in the management of psychogenic non-epileptic seizures (PNES). There is lack of knowledge about patients' pattern of adherence to the recommendations made after a neuropsychiatric assessment and discussion of treatment options take place. Objective: The following study evaluated the initial treatment retention pattern of 103 individuals diagnosed with PNES. Methods: After a neuropsychiatric evaluation, patients and their families attended a feedback session where the diagnosis and treatment recommendations were discussed in detail. We analyzed how many patients followed the recommendations as suggested during the feedback session. Clinical variables were analyzed to determine if they differed based on the pattern of adherence. Results: Of the 103 patients with PNES, 4 patients never returned for a feedback session. Of the 99 patients who attended the feedback session, 68 were offered full treatment (psychotherapy and, when indicated, psychiatric management) at the same institution and 16 patients were offered psychiatric management at our institution and psychotherapy treatment elsewhere. Fifty one percent of the patients who were offered full treatment and 31% of the patients who were offered divided treatment followed the initial recommendations. Both subjective cognitive complaints and current exposure to antiepileptic drugs were more common among the patients who did not follow the initial recommendations. Conclusion: Initial treatment retention in PNES is higher when full treatment is offered at the same institution, in which case it reaches 51%. Individuals with cognitive complaints and exposure to antiepileptic drugs have more difficulty following recommendations.
P5. Cyclosporine Reduces Alcohol Consumption Independent of Sucrose Consumption in C57BL Mice
P. H. Wu, T. Fay, N.J. Serkova, T.P. Beresford
Background: The calcineurin inhibitor cyclosporine (CsA) is an immunosuppressant routinely prescribed after liver transplant. Previously, we hypothesized that CsA reduces alcohol consumption and reported positive results in C57BL mice. Whether this 1) occurs from an anhedonic effects, and 2) is dose related is not known. To answer these questions, we measured the dose-dependent effects of CsA, hypothesizing that alcohol drinking is independent of sucrose consumption. Methods: 1) In a modified limited access paradigm, C57BL mice (n=30) received PO alcohol consumption training, starting with 0.6% and increasing to 10% alcohol solution. Following this, each mouse received vehicle (0.2 ml, IP) for 5 consecutive days and one of three CsA doses (10, 30, or 50 mg/kg in 0.2 ml, IP) for 5 consecutive days, in random order, before each 2 hour limited access session. Imbibed EtOH quantities were measured and recorded as g/kg per animal. 2) To assess the anhedonic effect of CsA on the consumption of sucrose, a separate test group (n=12) of C57BL mice were trained to drink 30% sucrose solution. The mice were then given vehicle (0.2 ml, IP) or CsA (50 mg/kg or 100mg/kg in 0.2 ml, IP) 30 minutes before limited access to the 30% sucrose solution. CsA concentrations in the brain were measured using LC-MS technique. Results: CsA exposure at each of the three doses (10, 30, 50 mg/kg) reduced alcohol intake significantly (Student's t-test): from 2.26±0.10 to 0.91±0.10 g/kg (p<0.001,), from 2.49±0.17 to 0.68±0.07 g/kg (p<0.001), and from 2.55±0.16 to 0.74±0.05 g/kg of alcohol solution (p<0.001), respectively. In contrast, CsA (50 mg/kg) increased the level of consumption of 30% sucrose solution from 5.47±0.75 g to 8.72±0.95 g (p<0.023). The CsA brain levels were 59.77±15.56 n/g (n=4) and 323.90±72.04 ng/g (n=5) in mice treated with 50 mg/kg and 100 mg/kg CsA respectively. Conclusions: These data suggest that CsA can selectively and dose-dependently reduce voluntary alcohol consumption through a mechanism other than that producing a drive to reduce sucrose intake. The selective reduction in alcohol choice occurs at lower doses than previously thought and may be related to CsA concentrations in the brain. Characterizing specific mechanisms of action will occupy the next steps in this line of investigation.
P6. Experience With the Severity of Ethanol Withdrawal Scale (SEWS) in Recognizing Early Withdrawal: A Contrast With the CIWA-A
T.P. Beresford, B. Schmidt, B. Pitts, K. McFann, M. Anderson
Background: The clinical danger of ethanol withdrawal can be mitigated when recognized early. Five of the ten items rated by the CIWA-A, commonly used as a withdrawal measure in healthcare settings, aim at late withdrawal. We devised the Severity of Ethanol Withdrawal Scale (SEWS) in order to focus on early withdrawal weighted by six of eight items. We report here our first experience with systematic application of the SEWS, in a setting where no withdrawal scale had been used before, and compare that to CIWA-A data, from regular use in a separate setting in our hospital, all in an effort to assess the quality of care in alcohol withdrawal treatment at our institution. Methods: The SEWS was made available to the nursing and medical teams of the Intensive Care Units at our federally supported hospital; prior to its use ethanol withdrawal recognition was done clinically by team members. The CIWA-A was in concurrent use on a psychiatric ward in the same hospital. Computerized versions of each were administered by nursing personnel when admitting patients to the respective sites. With institutional approval the de-identified cross-sectional data for serial admission during the same four month period were recovered, recorded, and stored for analysis. Independently, the SEWS (n=84) and CIWA-A data (n=165) underwent factor analysis performed by a statistician at our affiliate institution. Results: The SEWS data yielded a two-factor solution with Promax rotation to allow for correlated factors: most items loaded on Factor 1. Analysis of the CIWA-A suggested three factors, indicating that more than one construct was being measured. Early symptoms loaded on Factors 1 and 3, while late symptoms loaded primarily on Factors 2 and 3. Further factor analysis results with early versus late symptoms on the CIWA-A showed no clear relationship between factors and symptom onset. The same comparison on the SEWS, however, found that five of the six early symptoms, all except clinically evident agitation, loaded primarily on Factor 1 while the late symptoms of disorientation and hallucinations loaded on Factor 2. Conclusions: These early experience data suggest that the SEWS may be more effective in recognizing early alcohol withdrawal clinically. Prospectively designed research methods can test the hypothesis generated from this experience and may lead to improved treatment of ethanol withdrawal.
P7. Four-Dimension (4D) Change in Brain Substructure Volumes Among Alcohol-Dependent Subjects
Thomas P. Beresford, M.D., David B. Arciniegas, M.D., Dinggang Shen, Ph.D., Christos Davatzikos, Ph.D.
Introduction: Mechanisms of brain healing after heavy, dependent alcohol use remain to be defined. This study hypothesized that brain substructures would increase in size after 6 months of ceasing alcohol exposure. Method: Heavy drinking, alcohol-dependent subjects (n=14) provided brain data acquired on a dedicated 3T MRI scanner at baseline and again after 6 months of verified abstinence including disulfiram maintenance. These data underwent 4D automated volumetric analysis. Paired t-test of the means for each substructure tested change over time with alpha less than 0.05. Results: Baseline to follow-up comparisons of 93 brain substructures revealed that only 19 increased in volume, none significantly. Statistically significant structural loss appeared in 17 substructures. These included medial front-orbital gyrus right, middle frontal gyrus right, pre-central gyrus right, medial frontal gyrus left, angular gyrus right, temporal pole right, inferior occipital gyrus left, anterior limb of internal capsule left, superior occipital gyrus left, lateral occipito-temporal gyrus right, entorhinal cortex right, lingual gyrus right, parahippocampal gyrus right, middle occipital gyrus left, medial occipito-temporal gyrus right, and occipital pole left. Conclusion: These preliminary data suggest that a tendency toward significant structural volume lessening may characterize the first six months of abstinence. Further analysis should target individual variations and a longer period of prospective study.
P8. Three-Dimension (3D)-to-Four-Dimension (4D) Comparisons in Measuring Brain Volumes Among Alcohol-Dependent and Control Subjects
T. Beresford; D. Arciniegas; D. Shen; C. Davatzikos
Background: Automated volumetric analysis of magnetic resonance images offers a potentially useful tool in understanding the effects of heavy ethanol exposure on brain structures. In working with this, we compared two automated methods: 3-dimensional (3D) and 4-dimensional (4D), hypothesizing that the two would yield statistically identical results when applied to hippocampal volumes. Method: The study compared right, left, and total hippocampal volumes, using both methods in 1) heavy drinkers at baseline and after 6 months of abstinence (n=13), and 2) light-drinking controls at baseline (n=8). Student's t-test of paired sample mean volumes, with alpha at 0.05, tested the effects of chance between the two methods. Results: The drinkers' hippocampal volumes using the 4D method averaged 5.5% greater (range: 4.8% to 6.3%) than using the 3D method. The differences were significant in 5 of the 6 MRI study means (range: p=0.013 to 0.128). By contrast, hippocampal volumes in the light drinkers averaged 3.6% greater (range: 2.4% to 4.9%), using the 4D over the 3D method, and only the total hippocampal mean volume reached significance (p=0.036) between the two. Conclusions: Although 4D automated analysis appears to offer increased resolution and therefore precision in brain substructure volume measurement, direct comparisons with previous 3D methods may include a 5% chance of error due to the differences in analysis methods themselves.
P9. The Course of Neuro-Endocrine Healing From Alcohol Dependence
Thomas P. Beresford, M.D., David Arciniegas, M.D., Mark Laudenslager, Ph.D.
Background: A lifetime alcohol dependence (AD) diagnosis applies to 20% to 50% of patients in public and university general hospitals, many of whom require psychiatric consultation. Subtle early brain healing processes may involve changes in the neuro-endocrine stress system that can affect both cognition and decisions about treatment options. Method: To test whether neuro-endocrine healing occurs in frequent, heavy drinkers, this study 1) compared AD test subjects (n=16) with light-drinking control subjects (n=15) at baseline and then 2) assessed the test subjects prospectively at 3 and 6 months of supervised, disulfiram-assisted abstinence. The subjects provided diurnal salivary cortisol samples on waking, waking +30 minutes, noon, and 4 P.M. for each of the follow-up time-points. Significance required alpha = 0.05. Results: Baseline test-group cortisol means were significantly higher than control levels (p <0.04 to 0.003), with a notable absence of the morning cortisol response. The 3-month average diurnal curve suggested an exaggerated morning response (p<0.038), whereas the 6-month average curve approximated to the baseline control values. Conclusions: These data indicate that neuro-endocrine healing may take up to 6 months to reach its full potential. This suggests the possibility that 1) neuro-endocrine effects may impair complex cognition and decision-making early in the healing course; and 2) neuro-endocrine healing late in the course may account for the often unrealistic sense of well-being that occasions alcohol relapse. Focused treatment may serve to expedite healing and add to the likelihood of sustained remission.
P10. Catechol-o-Methyltransferase Genotype in Respect to Depression and Adaptation in Cancer Patients
Brook McConnell, M.D., Thomas Beresford, M.D.
Background: Depression is a common problem among cancer patients; however, despite multiple studies addressing psychotherapy and antidepressant medications, no definitive treatment recommendations have been made. A potential reason for this continued confusion is the role of underlying genetic abnormalities that may contribute to a patient's susceptibility to depression, or their ability to respond to treatment. One possible genetic culprit is the catechol-o-methyltransferase (COMT) gene. A polymorphism exists such that some individuals exhibit faster or slower dopamine metabolism, depending on their genotype. Method: The authors investigated a potential relationship between COMT polymporphisms and depressive symptoms and coping skills as assessed by the Beck Depression Inventory and the Defense Style Questionnaire, respectively. This study included 90 Stage 3 and Stage 4 cancer patients. Results: COMT genotype was not significantly related to either depression (p=0.0996) or coping skills (p=0.7940). Conclusions: These results indicate that depressive symptoms and ego defense mechanisms in cancer patients are not related to underlying genetic differences, but more likely related to the acute psychological trauma of their cancer diagnosis.
P12. Impulsivity, Habit and Addiction in Online College Gamblers
D. William Jolley, Ph.D., Deborah N. Black, M.D.
Background: Although impulsivity is a significant risk factor for gambling and other addictions, factors governing the transition from habit to addiction are less understood. Objective: Authors used the Iowa Gambling Task (IGT) in a virtual internet-gambling casino among college undergraduates to test our hypothesis that impulsivity, measured by the IGT, moderates the transition from habitual to pathological gambling. Methods: Students completed the IGT when they registered for e-CasinoLand. Slot machines were experimentally modified to vary return and payoff ratios. Results: N =146 students, 80% male. The median IGT score of -2.0 was lower than the population norm of 10, but expected in these young and predominantly male players. Nonparametric t-tests showed no association between IGT score and addiction, defined by betting frequency, amounts wagered or lost, and duration of play. Structural-equation modeling showed that, among the least impulsive players (highest quartile above median IGT score), gambling frequency and amount bet accounted for 85% of the addiction construct. In the most impulsive players (lowest IGT quartile), gambling frequency and amount bet accounted for only 58% of the addiction construct. Conclusion: IGT score robustly moderates the prediction of online gambling addiction among the least impulsive players, but the relationship was less robust for the most impulsive players. The “reward deficiency” hypothesis” may account for this paradoxical finding: Highly impulsive individuals may require stronger stimuli to develop a persistent habit. Including more exciting games may validate our hypothesis of an inverse relationship between IGT score and risk of addictive gambling.
P13. Possible ADHD in a Child With Agenesis of the Corpus Callosum
Adam B. Bloom, Glen E. Getz, Hannah Schofield
Background: Agenesis of the corpus callosum (ACC) is associated with a wide range of emotional, behavioral, and cognitive presentations. Studies have consistently demonstrated slowed processing speed, weaknesses in complex problem-solving, and typically depressed IQ scores in ACC. Furthermore, although a wide range of comorbid neuropathies occur in this population, there are limited studies examining psychiatric comorbidity beyond pervasive developmental disorders. The current clinical case presentation examines possible attantion-deficit hyperactivity disorder (ADHD) in a child with ACC. Case History/Results: This right-handed 8-year-old girl with ACC presented to a psychiatric outpatient clinic for a neuropsychological evaluation. A clinical interview, review of available medical information, a 5-hour battery of neuropsychological tests, and behavioral rating scales completed by her mother were obtained, and data will be presented. Attention deficits were observed in this child consistent with previous studies of ACC. The patient demonstrated intact cognitive functioning in numerous areas, including academic achievement, despite overall borderline IQ. She also demonstrated impaired performance in areas of executive functioning, visual memory, visual-motor, and constructional abilities. She demonstrated limitation in terms of attention and hyperactivity/impulsivity on objective measures, her mother's report on rating scales, and per behavioral observations. Conclusions: Although it remains unclear whether her collection of symptoms could be completely accounted for by ACC, treatment for ADHD may be warranted. ADHD has been related to other structural changes in the brain, which pharmacological intervention has been thought to help normalize, indicating a possible place for pharmacological treatment in ACC children, as well.
P14. Aricept Withdrawal Syndrome Treated with Lexapro
Brad Bobrin, M.D.
Background: Aricept is frequently prescribed for dementia and off-label for cognitive deficits for other disorders, but a withdrawal syndrome is infrequently described and its treatment has not. The author thus reports on a possible treatment for Aricept withdrawal syndrome. Case History: A 53-year-old bipolar patient with borderline personality disorder with memory and executive deficits was placed on Aricept up to 10mg, with report of positive results. However, her insurance would no longer cover the Aricept, and it was abruptly stopped. After 24 hours off the Aricept, she developed an acute constellation of symptoms, consisting of feelings of confusion, insomnia, tearfulness, memory loss, and severe decrease in her level of functioning. The literature speaks of a previously recorded syndrome with the same symptoms occurring with Aricept withdrawal or switching, but no mention of treatment. With the recognition that the symptoms were similar to SSRI withdrawal, Lexapro was chosen as a potential treatment. Within 48 hours of starting the Lexapro, the symptoms abated, although the cognitive benefits of the Aricept were lost. Further literature review shows laboratory evidence that serotonin can enhance acetylcholine release. Conclusion: This is the first encountered case of an SSRI treating Aricept withdrawal. The temporal onset of the symptoms after the abrupt discontinuation of the Aricept and the abrupt disappearance of symptoms after starting the Lexapro lend credence to the interpretation that the patient had a withdrawal syndrome and that it was treated by the Lexapro.
P15. Frontal-Temporal Dementia Presenting With Psychotic Depression, Polydipsia, Hyponatremia, and Pathological Lying
Brad Bobrin, M.D.
Background: Frontal-temporal dementia (FTD) presents with many different psychiatric presentations. The author presents an unusual case of FTD, which presented with psychotic depression, polydipsia with hyponatremia, and pathological lying. Further research on such unusual symptoms may help to increase the diagnosis of FTD. Case History: A 70-year-old patient presented with multiple somatic preoccupations, weight loss, anhedonia, psychomotor agitation, and SI. These were successfully treated with ECT. However, the patient had polyuria and polydipsia with hyponatremia and was placed on fluid restriction. However, he maintained polyuria. He was subsequently caught on multiple occasions drinking from the sink, the water fountain, or taking liquid from other patients' trays. He persistently either denied surreptitious drinking or minimized the amount he drank. This was accompanied by a noted change in his personality and comportment per his wife, perseveration and obsession, and word-finding difficulties. Neuropsyhological testing revealed predominant executive deficits with persevered visuospatial function. A diagnosis of FTD was made. He never recovered the insight into his polydipsia and lying and felt victimized. He was discharged to assisted living. The literature does not mention this combination of symptoms as being often found in FTD. We do note that the polydipsia was due to delusion about his bowels. Conclusion: We hope that the recognition of such symptoms will lead to further research into the prevalence of these symptoms in FTD and that the recognition of such symptoms in the young-old will lead to the consideration of FTD when such patients present to psychiatric wards.
P16. The Effect of Odor Cues on Declarative Memory in Adolescents
John J. Campbell, M.D., Liam James Campbell
Background: Research into human memory functioning has shown that memory may be enhanced by the use of cues. This study attempts to determine the effect of odor cues on declarative memory as tested by the Hopkins Verbal Learning Test - Revised (HVLT-R). Method: Thirty adolescent subjects (15 male and 15 female) were administered the HVLT-R while exposed to either vanilla extract, white-wine vinegar, or an odorless control (water). After a delay, subjects were re-exposed to the original odor and were then tested for recall. Results: Subjects exposed to vanilla extract were significantly more likely to recall information after a 5-minute delay than either the vinegar or control group (p=0.03). Conclusion: These results suggest that declarative memory can be enhanced by an odor cue.
P17. PTSD After TBI: Neural Mechanisms, Neuropsychiatric Manifestations, and the Diagnostic Consequences of Proposed DSM-5 Criteria
Christopher M. Davidson, M.D., David Whaley, M.D.
Background: Should PTSD (posttraumatic stress disorder) and TBI (traumatic brain injury) be considered mutually exclusive phenomena? Controversy exists over the brain's ability to form new memories in the context of a brain injury with resultant loss of consciousness. Due to the resultant loss of consciousness and amnestic periods related to violent impacts that twist and damage neuronal tissue, some authors opine that the development of PTSD from an accident involving TBI is not likely. Case Histories: Three TBI cases with different PTSD presentations, including military and civilian patients, are described yielding perspectives on neuropsychiatric symptomatology. These cases highlight the theory of subthreshold PTSD and the lack of consistency in defining TBI. Alteration in ability to form memories may actually play a protective role in diminishing the likelihood of reexperiencing the traumatic event. Some literature suggests that the greater the extent of the loss of consciousness of an accident victim the less likely that victim is to develop PTSD. In addition to amnesia for the traumatic event, TBI and PTSD may share other symptoms, including abnormalities of sleep, mood, executive function, and cognitive processing, making differentiating these syndromes difficult. Adding to the diagnostic challenge are overlapping symptom clusters existing in other neuropsychiatric syndromes, including MDD (Major Depressive Disorder), depression being the most common psychiatric disorder associated with TBI. Conclusion: This presentation reviews the neural mechanisms and neuropsychiatric manifestations of traumatic brain injury with resultant PTSD. Diagnostic challenges are highlighted and comparison made of ICD-10, DSM-IV-TR, and proposed DSM-5 criteria for the diagnosis of PTSD.
P18. Correlative Neuropsychiatric Symptoms With Anterior Cingulum Lesions Demonstrated by Diffusion Tensor Imaging
Yazmín De la Garza-Neme, Sarael Alcauter, Lourdes Martínez Gudiño Ma, Valente Cedillo
Background: Anterior cingulum (AC) abnormalities have been demonstrated in bipolar disorder by diffusion tensor imaging (DTI) and in postmortem studies. All of these previous studies have implicated the important role of the AC cortex and its connections with behavior and affect. Authors describe two cases of young men who had no family history of psychiatric illness and developed manic-depressive episodes under similar circumstances, with frontal lesions that involved the AC region. Case Histories: Case 1 is a 22-year-old man who presented a depressive episode 1 year before admission. He was hospitalized because of a sudden change in mood. He was noted to be getting increasingly irritable, hyperactive, and talkative, displaying flight of ideas. He also had decreased need for sleep, psychotic symptoms, misjudgment of conduct, and hypersexual behavior. The neurological exam revealed prominent frontal release signs. MRI showed a left frontal cavernoma. Case 2 is a 28-year-old man with a mild depressive episode 3 months before admission. He was admitted after several episodes of increased irritability and intentional activity, decreased need for sleep, talkativeness, aggressiveness, suspicious attitude, and delusional ideas. The neurological exam was normal. An MRI at admission showed an extensive area of left frontal encephalomalacia. In both cases, the neuropsychological testing demonstrated left prefrontal dysfunction and altered insight, and the DTI with tractography showed lost of continuity, thinning, and abnormal anisotropy values of the left AC. Conclusions: Disregarding the nature of these two different lesions, the disruption of the frontolimbic circuits in each case resulted in decreased prefrontal modulation of the anterior limbic network. This mood dysregulation was manifested as manic symptoms in both patients.
P19. Crossed Aphasia in a Dextral Patient With Logopenic/Phonological Variant of Primary Progressive Aphasia
Asli Demirtas-Tatlidede, Hakan Gurvit, Oget Oktem-Tanor, Murat Emre
Background: Crossed aphasia in dextrals is a rare phenomenon, with a prevalence of 1%–2% among all right-handed patients. Two patients with a nonfluent variant of primary progressive aphasia (PPA) have been previously reported. Logopenic aphasia (LPA) is a relatively newly-defined third variant of PPA, which clinically and anatomically differs from the other variants, progressive nonfluent aphasia and semantic dementia. This report aims to document for the first time the occurrence of crossed LPA in a dextral patient. Case History: A 57-year-old monolingual female patient presented with word-finding difficulties. She was strongly right-handed, had no clinical history for trauma or brain damage to the left hemisphere, and her family exhibited a tradition for right-handedness. Family history was positive for neurodegenerative diseases. Her language comprised simple, grammatically correct sentences, with a fluctuating speech rate and intermittent word-finding pauses. Rare phonological errors were noted. Sentence repetition tasks showed impairments with longer sentences. Comprehension was intact, as were writing and reading. Neurological examination was normal except for a positive Myerson sign and occasional coarse tremor in the left hand. The language disability remained isolated for 3 years. Cranial MRI scan pointed to symmetrical atrophy in the inferior parietal cortices, whereas SPECT perfusion imaging demonstrated hypoperfusion in the right parietal cortex, indicating right-hemisphere dominance for language. Conclusion: This clinical picture expands upon the previous literature that PPA may show reversed asymmetry for language and highlights the significance of incorporating functional neuroimaging into the diagnostic work-up for characterization of neurodegenerative diseases presenting with language impairments.
P20. Attention Deficit (Hyperactivity) Disorder: The Effect of Psychostimulants With or Without Atypical Neuroleptic Use on Comorbid Anxiety
B.M. DiVito, E.C. Bakken, D.D. Duane
Background: Many studies suggest a relationship between attention deficit (hyperactivity) disorder (AD[H]D) and anxiety (Anx). Among the controversies, however, is whether psychostimulants cause an increase in anxiety. Whereas some studies have investigated the effect of psychostimulants on anxiety, none have studied whether anxiety increases versus pre-psychostimulant use. Objectives: Authors investigated changes in Achenbach Child Behavioral Checklist (CBCL) anxiety T-scores pre- and post-administration of psychostimulant therapy; and observed whether atypical neuroleptic concomitant medication therapy has an effect on anxiety. Methods: Retrospective chart analysis of 134 (M-98/F-36) referred students (mean age: 10.2 years ±3.4) diagnosed with AD[H]D by DSM-IV behavioral and cognitive measures with parent completed CBCL both before and after treatment with a psychostimulant at least 4 months apart. A comparison was made on frequency of anxiety with those subjects in whom a concomitant neuroleptic was co-administered. Results: Psychostimulant only: N=80; Anx initial T score >65 =24; 20 (83%) dec T score to <65; Initial score <65 = 56; 3 (5%) inc T score to >65; Psychostimulant + Atypical Neuroleptic: N=54; Anx initial T score >65 = 15; 7 (47%) dec T score to <65; Initial T score <65 = 39; inc T score >65 = 12 (31%). Conclusion: Anx is a prevalent comorbid Dx in AD[H]D. Anx is not necessarily aggravated by stimulant Rx. Atypical neuroleptic co-administration does not necessarily protect against increase in Anx.
P21. Structural Differences in Emotional Brain Centers Associated With Joint Hypermobility: A Vulnerability Phenotype to Anxiety Disorders
Jessica A. Eccles, Felix D.C. Beacher, Marcus A. Gray, Catherine L. Jones, Ludovico Minati, Neil A. Harrison, Hugo D. Critchley
Background: Individuals with joint hypermobility are markedly overrepresented across panic and anxiety populations; however the neurobiological substrates underpinning this constitutional predisposition are currently unclear. Objective: Authors tested the hypothesis that vulnerability to psychological symptoms is related to constitutional differences in brain structure between people with and without hypermobility. Methods: Authors studied 72 healthy participants, using voxel-based morphometry (VBM) to explore associations between joint hypermobility, anxiety, and regional gray-matter volumes. Results: Hypermobile individuals (N=36) had significantly larger amygdala volumes bilaterally than people without joint hypermobility. Hypermobility scores were negatively correlated with gray-matter volume within the right superior temporal gyrus/sulcus and bilateral inferior parietal regions. On questionnaire ratings, hypermobile individuals also scored higher on measures of interoceptive awareness, a trait marker for anxiety vulnerability. Conclusion: Our findings provide important empirical support for the proposal that hypermobility represents one observable feature of a broader multi-system phenotype. By identifying, in a non-clinical sample, an association with the structural integrity of emotional brain centers, we provide insight into neural mechanisms that are likely to mediate the clinical expression of neuropsychiatric symptomatology across joint hypermobility syndromes. Moreover, our observations strengthen the case for differential characterization of anxiety phenotypes with implications of individualized treatment approaches.
P22. Challenging Neuropsychiatry: Case of Depression, Hallucinations, TBI, Alcohol Dependence, and Cognitive Impairment
Donald Eknoyan, M.D.
Background: This is a challenging neuropsychiatry case presentation of a patient with depression, auditory hallucinations, suicidal ideation, homicidal ideation, traumatic brain injury (TBI), alcohol dependence, and cognitive impairment. This clinical case will highlight the challenges of diagnosing and treating neuropsychiatric disorders. Case History: The clinical case is a 54-year-old left-handed man who presented for his first psychiatric hospitalization with symptoms of depression, hyper-religiousity, and hearing a voice telling him to harm himself and his family. He had significant cognitive impairment, scoring 19/30 on MoCA. Neurologic exam was significant for left hemifield visual defect. Head CT was significant for mild right parietal lobe atrophy and periventricular white-matter changes. His past history was significant for alcohol dependence (in recent remission) and mild traumatic brain injury. Because of persistent depression with hallucinations, he had ECT, with resolution of depression and hallucinations but continued cognitive deficits. Author will present the results from neuropsychiatric testing, PET scan, and video interview to enhance the presentation and discuss the challenges of diagnosing and treating neuropsychiatric disorders, and will also elicit feedback from the audience on alternative approaches and treatment of this patient. Conclusion: In many cases, longitudinal assessment and careful monitoring of treatment responses are needed to clarify obscure neuropsychiatric diagnoses. The use of neuroimaging and neuropsychiatric testing are helpful in establishing a differential diagnosis. However, sometimes clinical symptoms are what drive treatment when the etiology is likely multifactorial.
P23. EEG and Quantitative EEG Data as an Adjunct to Clinical Assessment Predicts Response to Atypical Treatment Options
W.H. Emory, M.L. Shatsky, C.G. Wells
Background: Depressive disorder affects up to 14.8 million U.S. adults. First-generation antidepressants are underutilized because of perceived toxicity and side effects, but are as effective as second-generation agents. Selegiline is indicated for treating Parkinson's disease, but because of dietary concerns, it is infrequently used in treating depression. Despite evidence for biomarker use in the treatment of depression, medication selection is typically guided by subjective information rather than objective data. Utilization of EEG data as guidance for therapeutics has been noted since the 1970s and has shown efficacy in predicting response to typical and atypical medications. To guide the selection of medication in this case study, both a visual electroencephalogram (EEG) and a quantitative electroencephalogram (qEEG) were obtained. Case History: A 42-year-old woman presented with a DSM-IV-TR diagnosis of Depressive Disorder, NOS, a failed trial of citalopram, and only slight benefit from buproprion. The qEEG showed deficiency in alpha magnitude and an excess beta trend, which together indicated a positive selegiline response. A comparison of baseline qEEG and qEEG on selegeline showed improvement in functional brain activity. Follow-up over 6 years revealed no side effects or need for dietary restriction. Conclusion: Selegiline monotherapy was the initial intervention selected and for 6 years, we observed the excellent clinical outcome of 3 out of 4 on a modified CGI. This example raises the possibility that qEEG can provide objective evidence for selecting atypical medications that otherwise may be overlooked.
P24. Delusional Parasitosis
Richard Ferrell, M.D., Thomas McAllister, M.D.
Background: Delusional parasitosis (DP) is a rare but agonizing disorder that occurs in an idiopathic form and a secondary form associated with other neuropsychiatric disorders. Etiology is obscure, but psychopharmacotherapy often helps. Case History: An 82-year-old woman sought help for a chief complaint of “bugs.” An infestation with head lice was previously treated. Although in good general health, she had discontinued citalopram and become depressed before delusional symptoms occurred. She developed an unshakable monosymptomatic delusion of infestation of her body with insects and mites. She believed that she ingested these organisms, and that they passed undigested through her alimentary tract. She self-treated with vinegar mouthwash. She showed us erythematous skin lesions that she attributed to mites; her husband asserted that they were caused by self-abrasion. She removed “specimens” with tweezers and saved them. She suffered great mental anguish. Skin examination did not reveal arthropods. No other psychotic symptoms were present. The MMSE score was 30/30. CT of the head showed mild cerebral atrophy and periventricular white matter hypoattenuation. DP responded to treatment with risperidone 0.5 mg. twice daily and resuming citalopram for depression. The skin lesions cleared. Dermatology literature tends to view the syndrome termed Morgellons disease, which includes fatigue and cognitive dysfunction, as a form of DP. Persons who think they have Morgellons disease disagree, believing that they have an infectious disease. Conclusions: The case shows an example of therapeutic efficacy for risperidone for DP in the context of resumed treatment of depression with citalopram. A CDC study is currently investigating Morgellons disease.
P25. Traumatic Brain Injury and Meditation
Roger N. Fox, M.D., David B. Arciniegas, M.D., Hal S. Wortzel, M.D.
Background: Traumatic brain injury (TBI) yields impairment across the spectrum of neuropsychiatric domains; many survivors remain symptomatic and limited in function despite engaging existing therapies. New treatments for TBI symptoms and optimizing function are needed. A small but growing body of literature suggests that various neuropsychiatric disorders may benefit from mediation practices. However, there remains very little exploration of the potential beneficial effects of meditation in TBI patients. Objective: To compare the convergence between the phenomenology, neuroanatomy, and neurochemistry in TBI with that of meditation. Methods: A PubMed search anchored to “meditation” was performed. Studies reporting clinical benefit from, or neuroanatomical and/or neurochemical correlates of, meditation were reviewed. Clinical and neurobiological findings were compared with those for TBI. Results: Interpretation of the meditation literature is complicated by the various techniques captured under the term “meditation” and the existence of few well-designed studies. However, mediation has been reported to be helpful in a number of neuropsychiatric domains: cognitive dysfunction (impaired attention, processing speed, memory); emotional problems (affect dysregulation, depression, anxiety); behavioral problems (aggression, impulsivity); and physical problems (sleep, pain, headache). Meditation appears to engage and augment function in specific brain regions (frontal, temporal lobes) via particular neurotransmitters (serotonin, dopamine, GABA). Conclusion: Meditation appears to recruit brain regions and augment neurotransmitter function in a manner that overlaps substantially with the neurobiology of TBI. Also, meditation has been reported to target neuropsychiatric symptoms that commonly cause impairment after TBI. Meditation may represent a novel therapeutic approach to TBI; further research is indicated.
P26. A Case of HIV Dementia
Mandy Garber, M.D, Emily Vaughn, M.D., G. Getz, M.D.
Background: Clinically significant neuropsychiatric disease typically occurs in late-stage AIDS. Approximately 15% of HIV+ individuals will develop dementia. As HIV infection becomes a chronic disease, the prevalence of related neuropsychiatric illness will increase.
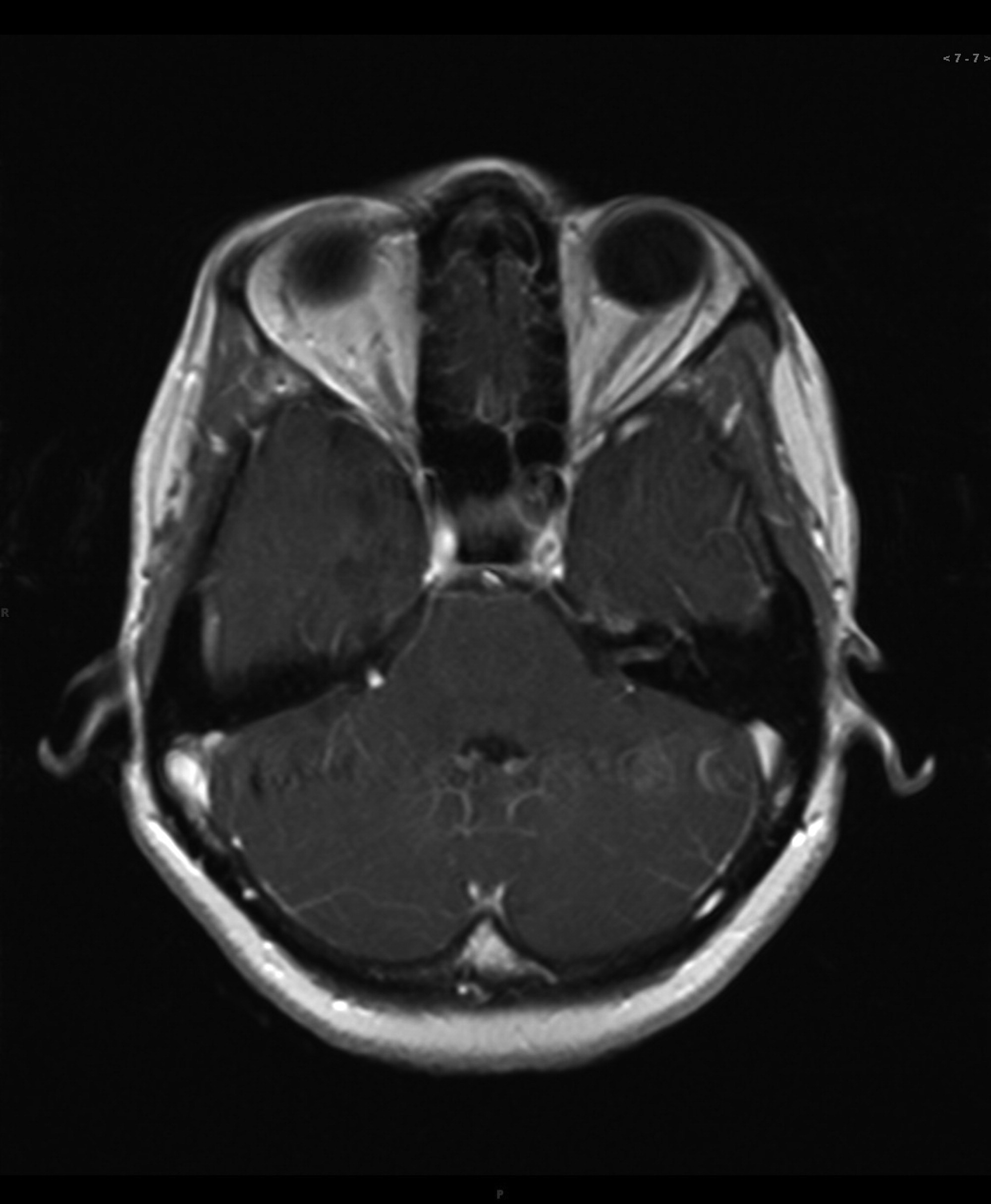
Case History: The patient is a 45-year-old, college-educated, South African immigrant, HIV+ since 1999, who presented in 2005 with a CD4 count of 103, viral load of 110,000, and was started on antiretroviral therapy. A year later, with CD4 of 188, and undetectable viral load, she experienced weakness and loss of balance. MRI showed diffuse signal abnormality, pial enhancement of CNVII, CNVIII, and right superior temporal gyrus (see
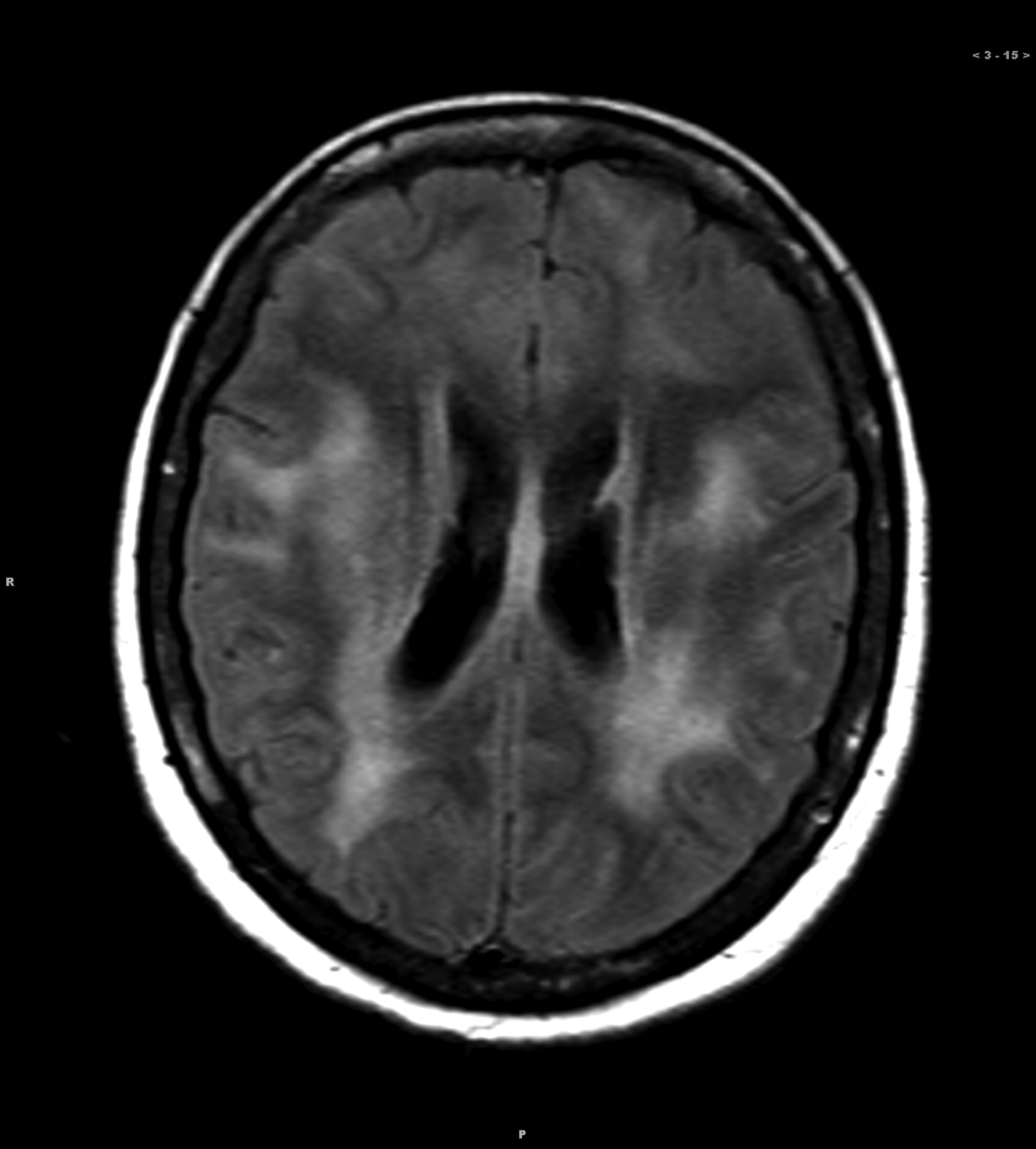
Figure 1). Differential diagnoses included encephalitis, lymphoma, PML, and vasculitis. Three months later, she was again hospitalized for mental status changes and seizures. MRI showed white-matter and brainstem abnormality, with patchy enhancement (
Figure 2). All CSF studies, MRA, and brain biopsy were normal. Neuropsychological status was followed over the ensuing years. In 2010, follow-up evaluation indicated CD4 of 535, undetectable viral load, and a halting gait. She was oriented to person and demonstrated marked cognitive decline.
Conclusion: Acute mental status changes may have been caused by an undiagnosed opportunistic infection. Treatment challenges include immigrant status, limited social support, and neuropsychiatric limitations.
P27. Primary Progressive Aphasia in a Bilingual Female: Dissociation Between Primary and Secondary Language Degradation
Eric D. Gausche, M.D., Neil H. Pliskin, Ph.D., Moises Gaviria, M.D.
Background: Bilingual patients with diagnoses of PPA have been previously reported in the literature, with the second language being either equivalently affected or more affected than the primary language. In general, little research has been conducted on bilingual/multilingual patients with neurodegenerative disorders, with the main exception being dementia of the Alzheimer's type. Case History: The authors present the case of a 78-year-old, dextral, well-educated, bilingual Hispanic woman who was fully fluent in both Spanish (her primary language) and English. Her initial presentation involved expressive language difficulties, primarily in English, which became so severe that she stopped speaking in English altogether and communicated exclusively in Spanish, which was relatively well preserved. She was eventually diagnosed with PPA. CT/PET fused scanning revealed decreased FDG metabolism in several areas, most prominently in the left inferolateral posterior temporal cortex (Z = –2.6) and left parietotemporal cortex (Z = –2.3) that was correlated with left perisylvian volume loss on the CT. Neuropsychological testing showed that, although she had deficits in Spanish, her deficits in English were more severe. Conclusions: This patient's pattern of language degradation may represent a feature of PPA in the bilingual patient, and differs in what has been reported in some studies on language function in Alzheimer's disease and Parkinson's disease populations.
P28. A Volumetric and Diffusion Tensor MRI Study of APOE ε4 in Multiple Sclerosis
Omar Ghaffar, M.D., M.Sc., FRCPC; N. Lobaugh, Ph.D.; M. Reis, M.D., FRCPC; P. O'Connor, M.D., FRCPC; A. Feinstein, M.Phil., M.D., Ph.D., FRCPC
Background: Evidence linking the ε4 allele of APOE to more severe brain MRI abnormalities in multiple sclerosis (MS) has been conflicting and limited to studies of lesion load and whole-brain atrophy. Objective: To determine whether the ε4 allele of APOE is associated with more structural and diffusion tensor MRI-demonstrable brain pathology in MS. Method: Using a Case–Control design, 43 MS patients with the ε4 allele (ε4+) and 48 ε4 negative (ε4–) MS patients underwent 3T MRI and diffusion tensor imaging (DTI). Hypo- and hyperintense lesion volume, atrophy (brain parenchymal fraction), and DTI parameters: fractional anisotropy (FA) and mean diffusivity (MD) in normal-appearing white matter, normal-appearing grey matter, and lesions were compared between the groups in the whole-brain and in medial-temporal regions. Results: ε4+ and ε4– MS patients were well-matched in demographic characteristics, disease variables, proportion receiving disease-modifying therapy, and presence of the APOE ε2 allele. ε4+ and ε4– patients did not differ in any MRI or DTI measure: hypo- and hyperintense lesion volumes, atrophy, and mean FA and MD in normal-appearing brain tissue and lesions. These findings applied equally to the whole-brain and medial-temporal regions. Conclusion: Contrary to several previous studies, this work does not support a role of the ε4 allele in MRI abnormalities in MS. These data also extend previous work by employing DTI and by specifying analyses to the medial-temporal regions in addition to the whole brain.
P29. Relationship Maintenance in Couples With a Partner Who Has Attention-Deficit Hyperactivity Disorder
Rachel Gilbert, Psy.D., Kim Gorgens
Background: Attention-deficit hyperactivity disorder (ADHD) in adults has been correlated with problems in relationships. ADHD has been associated with relationship inequity, in that a person with ADHD receives a greater perceived benefit from a relationship than his or her partner who does not have ADHD. Inequitable relationships are marked by a decreased use of relationship-maintenance behaviors, which are behaviors that support the relationship and help it to continue. Objective: The goal of the present study was to determine whether adults in relationships in which at least one partner had ADHD would perform fewer relationship-maintenance behaviors than those in relationships in which neither partner had ADHD. Method: The clinical sample consisted of 36 adults in committed romantic relationships. Participants were people with ADHD and people who reported that their romantic partners had ADHD. Data were collected with anonymous questionnaires, which collected information on demographic variables and relationship-maintenance behaviors, as assessed by the Relational Maintenance Strategy Measure. Data from the clinical sample were compared with those of a normative group. Results: As hypothesized, participants in relationships with at least one partner who had ADHD performed significantly fewer maintenance-behaviors than participants in the normative group. Conclusion: The decreased utilization of relationship-maintenance behaviors in the couples with at least one partner who had ADHD may have been due to possible comorbidity of other psychiatric disorders with ADHD, the negative influence of ADHD symptoms on relationship functioning, or insecure romantic attachment styles that may be prevalent in people with ADHD.
P31. Successful Use of Mirror Therapy for Phantom Limb Pain in the Intensive Care Unit
Colin J. Harrington, M.D., FANPA, Nicholas H. Carter, B.A.
Background: Phantom limb pain (PLP) after amputation is often poorly controlled by traditional therapies. Numerous pharmacologic, electrical, and surgical interventions have been used to address PLP, with limited success. Mirror therapy for PLP involves positioning a mirror to reflect the corresponding intact limb of an amputee so as to generate a visual and somatosensory experience of a normal limb in place of the amputated extremity. Numerous cases and a randomized, controlled trial have reported alleviation of PLP using mirror therapy; for some patients the effect has been immediate. Mirror therapy has been employed predominantly on an outpatient basis. Successful mirror therapy for PLP in the critical care setting has not previously been reported. Case History: A 24-year-old woman with a history of SLE and an associated hypercoagulable state underwent several revisions of a lower-extremity amputation. She experienced episodic “shock-like” PLP and phantom itch. Pneumonia, sepsis, bilateral pneumothoraces, and pericardial tamponade resulted in a protracted stay in the intensive care unit. An array of pharmacologic therapies failed to significantly reduce her PLP. The neuropsychiatry consultation service initiated mirror therapy and observed immediate reduction in PLP and itch. The patient used the mirror daily and reported consistent decrease in PLP and complete resolution of phantom itch. Conclusions: The efficacy of mirror therapy in treating PLP has bolstered new theories regarding the origin of phantom sensations. Mirror therapy is a low-risk, inexpensive intervention that can be effective against PLP even in the intensive care unit.
P32. Acupressure's Efficacy as a Non-Pharmacological Intervention for Traumatic Brain Injury (TBI)
Kristina L. McFadden, Ph.D., Kyle M. Healy, B.A., Miranda L. Dettmann, B.A., Jesse T. Kaye, B.S., Tiffany A. Ito, Ph.D., D. Frank Distel, Nathan Faes, Theresa D. Hernández, Ph.D.
Background: Acupressure is a complementary and alternative medicine (CAM) treatment using fingertips to stimulate acupoints on the skin. Although suggested to improve cognitive functioning, acupressure has not been previously investigated with a controlled design in traumatic brain injury (TBI) survivors, who could particularly benefit from a non-pharmacological intervention for cognitive impairment. Objective: Authors hypothesized that active acupressure treatments would confer greater cognitive improvement than placebo treatments, perhaps because of enhanced relaxation response induction and resulting stress reduction. Methods: A randomized, placebo-controlled, single-blind design assessed the effects of acupressure (8 treatments over 4 weeks) on cognitive impairment and state of being after mild TBI in 42 participants, including assessment of event-related potentials (ERPs) during Stroop and auditory oddball tasks. Results: Significant treatment effects were found comparing pre- to post-treatment change between groups. During the Stroop task, the active group showed greater reduction in both P300 latency (p = 0.010; partial η2 = 0.26) and amplitude (p = 0.011; partial η2 = 0.26), as well as a reduced Stroop effect on accuracy (p = 0.008; partial η2 = 0.21) versus the placebo group. Also, the active group improved more than placebo on the Digit Span test (p = 0.043; Cohen's d = 0.68). Conclusion: Together, these results suggest an enhancement in working memory function associated with active acupressure treatments. Since acupressure emphasizes self-care and can be taught to novice individuals, it warrants further study as an adjunct treatment for TBI.
P33. Biomarker-Positive and -Negative Subjects in the Alzheimer's Disease Neuroimaging Initiative: Clinical Characterization
Richard Kennedy, M.D., Ph.D.; Lon Schneider, M.D.; Gary Cutter, Ph.D.
Background: The Alzheimer's Disease Neuroimaging Initiative (ADNI) is intended to set standards for brain imaging and biomarkers for diagnosis and treatment trials. Recent expert recommendations have advocated that CSF and other biomarkers be used as entry criteria into clinical trials to improve efficiency. Objective: To characterize any clinical differences between biomarker-positive and -negative MCI (mild cognitive impairment) subjects based on proposed CSF Aβ1-42 cutoffs. Methods: The 400 MCI subjects in the ADNI database downloaded on July 27, 2010 were grouped based on whether individuals did or did not undergo lumbar puncture (LP), and the former was subdivided into high and low Aβ1-42 based on the published cutoff of 192. Groups were compared by t-tests or Wilcoxon tests. Results: Subjects who underwent LP did not differ significantly from those without LPs on any demographic and clinical data. However, subjects with low Aβ1-42 were significantly worse at baseline than those with high Aβ1-42 on a variety of measures, including the Logical Memory II Delayed Recall, the Alzheimer's Disease Assessment Scale-Cognitive (ADAS-Cog), and FAQ. Conclusions: Although LP does not appear to introduce a selection bias in the ADNI dataset, individuals with low Aβ1-42 showed not only greater cognitive and functional impairment than those with high levels that may require statistical adjustment in analyses, but also high rates of AD. However, if more severe cognitive impairment is associated with poorer treatment response, the use of biomarker-positive selection criteria may introduce confounding with poor response that cannot be corrected statistically.
P34. From Clinical Research to Clinical Practice: Neuroimaging in Dementia
Jillian Kowalski, Moises Gaviria, M.D., Sandra Horowitz, M.D.
Background: Dementia is largely a clinical diagnosis made after cognitive decline. Research has developed new neuroimaging techniques that could lead to earlier diagnosis with the hope of preventing/slowing the progression of dementia. However, imaging available in clinical practice lags behind what is available in clinical research. Objective: To compare neuroimaging techniques available in clinical practice for Alzheimer's disease (AD) and vascular dementia (VaD) and those being investigated in clinical research. Method: PubMed literature search. Results: Images of each technique will be displayed with their advantages/disadvantages, reimbursable by insurance status, and what future implications each have in clinical practice. One AD imaging technique, fluoroxyglucose positron emission tomography, shows decreased metabolism in the parietal temporal lobes and hippocampus in AD. This is available clinically and is covered by some insurance plans. Newer PET ligands that bind beta-amyloid plaques (Pittsburgh compound B, florbetapir) are more specific to AD and may establish earlier diagnosis. However, few centers carry such compounds, and they are not FDA-approved for clinical use. Neuroimaging of VaD is less researched. One study found diffuse tensor imaging to be more reliable and sensitive in early detection of cognitive impairment in patient with vascular disease than standard MRI. Lastly, continuous arterial spin labeling determines decreased blood flow noninvasively and shows promise for both AD and VaD. Conclusion: A gap exists in neuroimaging between developments in clinical research and what the clinician can utilize for the patient's benefit. This leaves the discussion of who should be responsible for bridging this gap.
P35. A Population-Based Investigation of the Association of Hippocampal Volume With Depressive Symptoms: Striving Toward a Definitive Answer
Yingying Kumar; Yonas E. Geda, M.D.; Stephen Weigand; Scott Przybelski; Kejal Kantarci, M.D.; Ronald Petersen, M.D., Ph.D.; Clifford Jack, M.D.
Background: The hippocampus is the epicenter of the memory circuit, and it has extensive reciprocal connections with structures implicated in emotional regulation. Studies that reported associations between depression and hippocampal volume were either of relatively small sample size (N < 100) or were conducted in clinical settings. The field needs to definitively address this question by using a large sample derived from a population-based setting. Objective: To determine the association between depressive symptoms and hippocampal volume, white-matter hyperintensity, and whole-brain volume. Methods: We conducted a cross-sectional study involving 1,385 cognitively normal elderly persons (47% women, mean age [SD] = 79.4 [5.2]), derived from the population-based Mayo Clinic Study of Aging (MCSA) in Olmsted County, Minnesota. Inclusion in this study required magnetic resonance imaging (MRI) of the brain within 120 days of administration of the Beck Depression Inventory (BDI). “FreeSurfer” was used to measure hippocampal volume, “Grinder” to measure whole-brain volume, and “RegionGrow” to measure white-matter hyperintensity. Non-parametric spearman rank-order correlation was used to examine association between BDI score and brain volume. Results: After adjusting for age, sex, education, and Clinical Dementia Rating, we observed the following: There was no correlation between BDI and hippocampal volume (r=0.01; p=0.79) or white-matter hyperintensity (r=0.03; p=0.36). There was a small but significant trend toward negative association with whole-brain volume (r = –0.05; p=0.06). Conclusion: There was no association between depressive symptoms and hippocampal volume in this large, population-based study.
P36. Diagnostic and Treatment Challenges in Patients With Traumatic Brain Injury
Margo D. Lauterbach, M.D.; Paula Notarangelo, R.N.-B.C., M.S.; Vassilis E Koliatsos, M.D.
Background: Traumatic brain injury (TBI) can lead to subsequent mood and behavioral problems that may pose treatment challenges. Such presentations can be conceptualized as diagnostic dilemmas that drive treatment choices. For example, the diagnoses of mood disorder due to TBI and personality change due to TBI are frequently used and can warrant different treatment approaches. Objective: Given the paucity of case-derived data available within the TBI patient population, this case series serves to demonstrate how several TBI patients in the authors' clinic have been diagnosed and subsequently treated. Methods: A retrospective case study was conducted on adult traumatic brain-injury patients that regularly attend an outpatient neuropsychiatry clinic. All subjects had sustained a moderate-to-severe head injury and have been followed regularly for ongoing neuropsychiatric follow-up and treatment. Results: Each case is analyzed according to the patient's demographic information, injury site, diagnosis(es), impairments (cognitive, behavioral, mood, and thought disorders) and psychopharmacological treatments utilized. Of those studied, a wide variety of diagnoses have been made. More than 80% of patients are prescribed mood stabilizers, 1/3 of which take valproic acid specifically. Other psychopharmacological agents include antipsychotics (around 50%), antidepressants (around 33%), benzodiazepines (around 10%), and others. Conclusion: Psychopharmacological treatments of mood and behavioral disorders that result from traumatic brain injury include a wide range of agents that require focused symptom-management. Prescribing trends are highlighted in this case series, and they attempt to exemplify the complex art of neuropsychiatric psychopharmacology.
P37. Catatonic Behavior in Dementia With Depression
Eliot Licht, Joan Scheibel, Mario Mendez
Background: Clinicians do not fully understand the mechanisms of catatonic behaviors. Patients with depression complicating dementia may be predisposed to catatonic behaviors. Objective: To report two patients with catatonic behavior in dementia with depression and discuss the potential pathophysiology. Methods: Authors describe patients with catatonic behavior who were admitted to a psychiatric inpatient service, and the literature is reviewed. Results: A patient with dementia and depression, with previous suicide attempts, was admitted because of agitation and subsequently became totally unresponsive. His exam revealed catatonic rigidity with waxy flexibility, which abated with intramuscular lorazepam. Addition of aripiprazole to citalopram improved the underlying mood disorder. The second patient had a similar history of agitation. He became apathetic and akinetic, with limited verbal output and minimal physical activity, and resisted eating or drinking. The symptoms appeared more prominent after discontinuation of neuroleptic treatment. The behavioral changes resolved after citalopram was increased. A review of the literature indicates that patients suffering from depression on a background of cognitive impairment may be particularly predisposed to the range of catatonic behaviors. Conclusions: Among patients with dementia, catatonic behaviors, ranging from catalepsy to akinetic mutism, may be expressions of depression. Cognitive impairment, possibly with frontal-executive deficits, may facilitate catatonic behavior, which should be distinguished from the similar abulia, mitgeghen, and mitmachen behaviors of frontally-predominant dementias.
P38. Neurological Lesions Associated With Pedophilic Behavior
Mario Mendez, M.D., Jill Shapira, M.D., Ronald Saul, M.D.
Background: Child molestation or other pedophilic behavior may result as a consequence of a brain disorder. Yet the mechanisms of this behavior are unclear. Objective: To investigate the relationship and mechanisms of brain disease and pedophilic behavior. Method: Authors report on eight patients with pedophilic behavior as a manifestation of their brain disorder and review the literature. Results: All eight developed sexual behavior toward prepubescent children in mid- to late-life, coincident with the development of a neurological disorder. Five had limited insight, anxiety, or concern for their behavior and tended to have frontal lobe executive deficits. Most of this group had frontally predominant disorders. Two others retained insight and concern in the context of marked hypersexuality. This second group had treated Parkinson's disease that resembled reports of pedophilic behavior from subcortical lesions. The further presence of right temporal lobe-amygdala involvement may have predisposed to specific sexual preoccupation in some patients. Conclusions: Brain disorders may release a predisposition to sexual attraction to children through disinhibition, with frontal disease, sexual preoccupation, with right temporal disease, or hypersexuality, with subcortical disease in non-motor basal ganglia, hypothalamus, or septal nuclei. Differentiating these mechanisms of pedophilic behavior caused by brain disease could facilitate targeted interventions.
P40. Innate Immune Activation in Pediatric Autoimmune Neuropsychiatric Disorders Associated With Streptococcal Infections (PANDAS)
T.K. Murphy, M.M. Longley, M.J. Dorsey, E.E. Perez, P. Sriaroon, J.W. Sleasman
Background: Children with PANDAS develop severe behavioral changes, with obsessive-compulsive disorder (OCD) or tic symptoms, associated with group A streptococcal infections (GAS). Cross-reactive antibodies to basal ganglia is a proposed link between infection and this disorder; sCD14 is released after TLR2 and TLR4 ligation by bacterial peptidoglycan and lipopolysaccharide, respectively. N-acetylglucosamine, present in bacterial peptidoglycan, is a dominant epitope of GAS and the neuronal cell surface molecule GM1. Antibodies to N-acetylglucosamine have been linked to PANDAS-related conditions. Objective: To investigate the role of macrophage activation in PANDAS, authors measured sCD14 as a surrogate marker of immune activation. Methods: sCD14 ELISA was performed on samples from pediatric healthy subjects (n=22) and PANDAS patients (n=21; mean age 10.2 years, 11M/10F) who met strict criteria after extensive neuropsychiatric evaluation. Demographic data were collected, including clinical presentation, therapy, and presence of comorbid conditions. Consent for all subjects was obtained using IRB-approved protocol. Results: sCD14 in PANDAS patients was increased significantly (mean: 6,359 ng/ml ± 1,187) versus healthy donors (mean: 1,777 ng/ml ± 1,051; p <0.0001). sCD14 correlated positively with ASO titers (r=0.5314; p=0.0192). History of maternal autoimmune disease was present in 6 of 21 patients with PANDAS (28.6%). Conclusions: Elevated sCD14 levels reflect macrophage activation coinciding with acute neuropsychiatric presentations. Correlation with increased ASO titers supports a role for GAS autoimmunity. Together, these findings strengthen the link between innate immune activation and other immunological mechanisms involved in PANDAS.
P41. Immune-Related Risks in Children Presenting With OCD and Tics
Tanya K. Murphy, Susan Swedo, Kytja Voeller, Madeleine Cunningham
Objective: This presentation will examine the clinical immune history of children with tics and/or OCD to inform upon hypothesized etiology and risk factors in Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS) presentation. Method: Physical examination, laboratory measures, and diagnostic interviews obtained on these children will be discussed, highlighting characteristics that define this phenotype, immunologic assays (antibodies, immune functioning, and proposed biomarkers), and neurological signs. Results: Children best approximating the current criteria for PANDAS have evidence of a complex but specific neuropsychiatric presentation, show evidence of immune activation, and have neurological signs that occur more often in acute presentations. Treatment with immune therapies shows promise in alleviating this disabling condition. Conclusions: This presentation offers preliminary evidence for a relationship between PANDAS and clinical immunological risks. The identification of associated features should be informative about onset-related risks.
P42. Neuropsychological Implications of Attention-Deficit Hyperactivity Disorder in an Adult With Multiple Sclerosis and Mood Disorder
Allison Myers, John King
Background: ADHD presents with a large symptom overlap with other psychiatric diagnoses and sometimes can be mimicked by other common medical conditions. It can affect interpretation of neuropsychological results and diagnostic accuracy. This case study reports neuropsychological findings in a 57-year-old woman diagnosed with MS, ADHD, and suspected history of bipolar disorder. Case History: ADHD in adults is often unrecognized, underdiagnosed, and undertreated. It is a common comorbidity in bipolar disorder patients or is misdiagnosed as bipolar disorder. Diagnostic accuracy is limited by the different manifestations of ADHD symptoms. Research reports that not all adults with ADHD have executive functioning deficits on neuropsychological testing. Moreover, a neurological examination is often recommended to rule out soft neurological signs because of the high incidence associated with ADHD. In the current case study, the patient was referred by her neurologist because of memory complaints. Results: MRI scan of the brain revealed multiple T2 white-matter lesions in a periventricular, radially-oriented configuration. Neuropsychological testing assessed effort, intellectual, memory, executive, language, motor, attention, and personality functioning. Examination showed impairments among perceptual reasoning, processing speed, working memory, attention, memory, executive functioning, motor functions, and symptoms of depression and anxiety. Conclusions: Overall, concomitant neurological and psychiatric features are likely responsible for the patient's impairments across cognitive domains. Results of this study highlight the difficulty in determining the cognitive sequelae of MS in the context of baseline impairments (ADHD) and in determining appropriate mood etiology. These findings illustrate the importance of diagnostic vigilance and the clinical interview.
P43. Neurotherapy of Attention Deficit/Hyperactivity Symptoms
David V. Nelson, Mary Lee Esty
Background: Neurobehavioral interventions, including brainwave-based treatments (e.g., EEG, biofeedback), have demonstrated some effectiveness in treating ADHD-like symptoms. Recent developments in neurotherapy suggest that more specific electromagnetic (EM) stimulation of brainwave activity may be beneficial. Objective: To conduct a pilot investigation of the efficacy of the Flexyx Neurotherapy System (FNS) that uses minute EM pulses to subliminally stimulate the EEG for the treatment of ADHD-like symptoms. Methods: 69 participants (children, adolescents, and adults; median age = 18 yrs) with attention deficit/hyperactivity symptoms referred to the Brain Wellness and Biofeedback Center of Washington were treated with an adaptation of FNS (median: 15; range: 4–49 sessions). Individual-session 0–10 ratings of most bothersome symptoms (attention/concentration, motivation/initiation difficulties, organizational difficulties, hyperactivity, distractibility, mental fog, procrastination, mood issues, racing brain, memory problems) were completed by each participant at the beginning of each treatment session. Results: Linear trend analyses indicated significant negative slopes (betas with all ps <0.001) in evidence for decreases in all symptom ratings over the course of individual treatment. Conclusion: FNS is a potentially effective treatment for attention deficit/hyperactivity symptoms and related dysfunction. A randomized, controlled trial with long-term follow-up is warranted to further verify these highly suggestive findings.
P44. Neurocognitive Discrepancies Between Autism and Asperger's: Beyond Language
Pravesh Basnet, Chad A. Noggle, Aman Mahjan, Johnathan Yost, Aghaegbulam Uga, Trinadha Pilla, Raymond S. Dean
Background: Cognitive discrepancies between autism and Asperger's syndrome remain the primary differentiation between the two presentations. However, this remains primarily fixated on differences in verbal development and functioning. Although other differences have been discussed, few have sought to determine what, if any, differences exist beyond those potentially attributable to the aforementioned verbal differences. Objective: The current study sought to investigate differences in the underlying cognitive profiles of a sample of individuals with autism or Asperger's that remained after controlling for differences in language functioning in the form of verbal comprehension, as this represents the most noted difference between the presentations. Methods: Participants included 12 individuals diagnosed with autism and 15 individuals diagnosed with Asperger's. Participants underwent standardized cognitive assessment. Standard scores were calculated, and statistics were run. Results: A multivariate analysis of covariance revealed that, as expected, groups differed significantly in their verbal comprehension capacity (p<0.007), favoring individuals with Asperger's over autism. Of interest, after controlling for this difference, significant discrepancies remained between groups; individuals with autism performed significantly worse than those with Asperger's in visual-auditory learning and memory for words. No difference was found between groups in spatial relations, concept-formation, visual matching, numbers reversed, incomplete words, picture recognition, and analysis-synthesis. Conclusions: Findings are consistent with previous results that demonstrate group differences in the core domain of verbal comprehension. Beyond this, the study extends our understanding of the neuropsychological differences between groups by showing that differences exist even beyond those explained by the aforementioned language differences.
P45. Relative Impact of Comorbid Depression and/or Anxiety After Closed Head Injury
Aghaegbulam Uga, Chad A. Noggle, Trinadha Pilla, Gaurav Jain, Subodh Jain, Lokesh Shahani, Raymond S. Dean
Background: Neurological insult such as closed head injury (CHI) is known to increase the risk of comorbid psychiatric manifestations, with depression and anxiety being the most commonly occurring. Although it is also suggested that such presentations further exacerbate cognitive deficits arising from the neurological presentation itself, further research is warranted. Objective: The current study investigated whether the presence of comorbid depression or anxiety negatively affected performance in a sample of children, adolescents, and young adults with history of CHI versus a similar sample with no documented or noted depression or anxiety. Methods: Participants included 192 individuals with a history of CHI without comorbid psychiatric features and 184 individuals with of CHI and comorbid psychiatric features. Participants completed a neurocognitive assessment. Scores were entered into a data-set, and statistics were run. Results: A multivariate analysis of variance revealed that significant differences existed between groups. By way of a discriminant-function analysis, subtest/domain-specific discrepancies were noted. Specifically, participants with comorbid psychiatric features performed significantly worse on tests of concept-formation, which involved abstract reasoning and novel processing; visual matching, which requires rapid visual scanning and attention, and numbers reversed, which looks at sustained attention/working memory. Conclusions: Findings are seen as additional support of the idea that neurocognitive functioning after CHI is further impeded by the presence of comorbid psychiatric features. As such, practitioners must remain vigilant in identifying psychiatric features and properly treating them to achieve the best recovery.
P46. Is There Such a Thing as Pseudo-Mild Cognitive Impairment? Exploring Cognition in Middle-Aged Depression
Subodh Jain, Chad A. Noggle, Lokesh Shahani, Pravesh Basnet, Aman Mahjan, Johnathan Yost, Raymond S. Dean
Background: Neurocognitive deficits have commonly been associated with depression; however, this has most prominently been noted in late adulthood. In comparison, fewer studies have focused on the middle-adulthood population, which raises questions from a practice-based standpoint, given the rise in interest of Mild Cognitive Impairment (MCI), which is diagnosed at a relatively similar time and thus expands the pseudodementia discussion. Objective: This study sought to determine what, if any, neurocognitive deficits would arise in relationship to depression in middle adulthood and how they may differ from those seen in or associated with MCI. Methods: Middle-aged adults (N=108) diagnosed with depression, who had completed the cognitive measures of the Dean-Woodcock Neuropsychological Battery, were extracted from an archival data-set for statistical analysis. Outcomes across seven separate neurocognitive domains were compared with the normative sample. Results: Focal decline in an aspect of long-term memory and retrieval, as evidenced by performance on the visual-auditory learning subtest of the WJ-III-Cognitive was noted (t[107] = –3.587; p=0.001), while sparing other domains (i.e. verbal comprehension, spatial relations, sound-blending, concept formations, visual matching, and numbers reversed) was found. Conclusions: Findings not only demonstrate the deficits associated with depression in middle adulthood but also carry implications for clinical practice. In particular, the areas of deficiency are similar to those affected by MCI, suggesting a potential for diagnostic error, and thus emphasizing the importance of expanding investigations into the differentiation of these entities in a similar way as has been done with depression and Alzheimer's disease.
P47. Methotrexate-Induced Toxicity Plus or Minus Cerebral Radiation: A Qualitative Comparison of Two Pediatric ALL Cases
Chad A. Noggle, Gaurav Jain, Subodh Jain, Lokesh Shahani, Pravesh Basnet, Aman Mahjan
Background: Research has demonstrated potential negative side effects of both radiation and chemotherapy on neurocognition. When used in conjunction, the impact can be escalated, which can be life-changing when this treatment is received in early childhood. Objective: The study sought to compare qualitatively two children with relatively similar medical backgrounds, aside from the fact that one child required preventive whole-brain radiation in addition to his chemotherapy regimen of methotrexate, whereas the other patient only required the latter. The idea was to evaluate the potential additive negative effect of radiation on cognitive development beyond that associated with chemotherapy. Methods: The patients were a 12-year-old girl and a 15-year-old boy. Both were treated between the ages of 4 and 5 for ALL with a regimen of methotrexate. In both instances, toxicity was experienced, resulting in seizures and leukodystrophy. The boy was also treated with cerebral radiation. Results: Across all domains of neurocognitive functioning, the boy presented with significantly greater impairments than both the girl and normative, grade- and age-equivalent samples. The girl demonstrated deficits in cognitive efficiency, executive control, mathematics, reading comprehension, sustained attention, and working memory. Similar deficits were noted in the boy, although to a greater extent. In actuality, his deficits were so significant and widespread that he presented as mildly mentally retarded, although adaptive skills were not similarly impaired. Conclusions: Although not quantitatively sensitive, the comparison demonstrates the traumatic impact of cerebral radiation can have when used in combination with chemotherapy and when utilized during early development.
P48. Memory Functioning in a Sample of Referred Patients with Fibromyalgia: An Exploratory Approach
Lokesh Shahani, Chad A. Noggle, Pravesh Basnet, Aman Mahjan, Johnathan Yost, Aghaegbulam Uga, Jon C. Thompson
Background: Patients with fibromyalgia will commonly report short-term memory loss, but few studies have sought to fully dissect memory functioning in these patients through standardized means. Consequently, a broader array of deficits is often noted, thus questioning whether memory deficits may go beyond just short-term impairments. Objective: The current study sought to investigate the emerging memory profiles of a group of patients with fibromylagia in comparison to the normative sample through an exploratory means. Methods: Participants included 35 individuals diagnosed with fibromyalgia who were assessed across measures of immediate and delayed memory to determine the pattern of performance. All participants had normal neuroradiological and electrophysiological work-ups. Measures of effort were used to screen for validity and remove those who performed below acceptable levels. Scores were calculated and converted into standard scores for comparison. Bonferroni corrections were used to control for inflation of family-wise error rate. Results: Results demonstrated significant impairments (p<0.002) across both immediate learning and delayed memory tasks in patients diagnosed with fibromyalgia as compared with the normative sample. These deficits were seen in immediate learning of unrelated as well as contextually-based information, delayed recall of both visual and verbal information, and even delayed recognition of verbal information. Conclusions: Findings suggest a far broader impact of memory in relation to fibromyalgia then has been previously proposed. Such findings in the absence of significant findings on neuroimaging and/or EEG are consistent with the remainder of the presentation in that a physiological correlate is not yet defined.
P49. Does Sex Affect the Risk of Psychiatric Symptoms Emerging After Neurological Insult? An Exploratory Analysis
Trinadha Pilla, Chad A. Noggle, Gaurav Jain, Subodh Jain, Lokesh Shahani, Pravesh Basnet, Anya Mazur-Mosiewicz, Beth Trammel, Raymond S. Dean
Background: Neurological diseases and presentations have been long seen as risk factors for psychiatric manifestations. What is not known is whether various demographic factors mediate the risk of this comorbidity. Objective: The current study investigated whether biological sex was associated with different relative risk rates of psychiatric manifestations after neurological insult. Methods: Participants included 915 individuals referred to an outpatient neurology clinic and eventually diagnosed with either brain tumor, cerebrovascular disease/accidents, hypoxia, multiple sclerosis, cerebral palsy, epilepsy, TBI, dementia, or Parkinson's disease, after neurological and neuropsychological work-up; 386 were diagnosed with a neurological disorder and no comorbid psychiatric disorder; 529 were diagnosed with both a neurological and a psychiatric disorder after standardized evaluation. Men and women were grouped, and statistics were calculated with comparisons made against sex-based prevalence rates for mental illness in the normal population listed by the CDC. Results: For both men and women, cerebrovascular disease, multiple sclerosis, TBI/CHIs, dementia, and Parkinson's were linked with increased risk. No such increase was found with a history of brain tumor or epilepsy. Only women demonstrated increased risk with hypoxia and cerebral palsy. Overall, both sexes were at relatively equal increased risk. Conclusions: Although findings are seen as additional support of the idea that a positive neurological history puts an individual at higher risk of psychiatric residuals, when controlling for reported premorbid differences, no differences emerge between men and women, suggesting equality in the capacity to adjust to disease and the potential functional alterations associated with it.
P50. Covariance of Sensory-Motor and Cognitive Profiles in a Sample of Pervasive Developmental Disorders
Johnathan Yost, Chad A. Noggle, Aghaegbulam Uga, Trinadha Pilla, Gaurav Jain, Subodh Jain, Raymond S. Dean
Background: Asperger's syndrome and autism have both been associated with sensory and motor deficits of varying severity, predominately described as clumsiness, but little has been done to investigate whether this may, in fact, in some way related to overall CNS compromise and thus be related to or predictive of levels of cognitive functioning. Objective: The current study sought to determine whether the purported motor and sensory impairments that often exist within the context of these presentations are in any way predictive of the nature or extent of cognitive impairment seen on standardized assessment. Methods: Participants included 10 patients diagnosed with autism and 11 with Asperger's. All patients were diagnosed via neuropsychological evaluation. Participants completed a standardized sensory-motor examination and cognitive assessment. Results: Canonical correlation revealed that, in general, sensory-motor performance was most predictive of verbal comprehension outcomes both for individuals with autism and those with Asperger's. Palm-writing, object identification, simultaneous localization, finger-tapping, and cross-construction were significantly related to both verbal comprehension and visual-auditory learning in both groups. Romberg status was significantly related to verbal comprehension in both groups. Furthermore, left–right movements were linked with sound-blending. Differences emerged with Asperger's participants demonstrating a significant link between object identification and finger identification performance and all cognitive domains aside from sound-blending. Conclusion: Findings reiterate research that demonstrates a general link between sensory-motor functioning while also demonstrating the unique relationship of sensory and motor skills with cognitive domains in these disorders.
P51. Does the F-Scale of the MMPI-2 Predict Outcomes on Validity Measures in Neuropsychological Assessment? Links Between Cognitive and Psychiatric Malingering
Aman Mahjan, Chad A. Noggle, Johnathan Yost, Aghaegbulam Uga, Trinadha Pilla, Gaurav Jain, Jon C. Thompson
Background: Malingering has been discussed from both an exaggeration-of-cognitive-deficits standpoint and an over-reporting of psychiatric symptoms, but little has been done to determine their link. Objective: The current study investigated whether there is linearity in the relationship between outcomes on the F-Scale of the MMPI-2, which is a measure of symptom-exaggeration or feigning, and outcomes on cognitive-effort testing. Specifically, do individuals malinger in one domain and not the other, or does it occur in both arenas? Methods: Participants included 21 individuals who completed both the MMPI-2 and the Test of Memory Malingering as part of a comprehensive neuropsychological assessment. The MMPI-2 F-scale score was rendered as a by-product of the computer scoring software. The TOMM scale scores were calculated according to manual guidelines. Correlational analyses were run. Results: Canonical correlation showed a significant relationship between outcomes on the F validity scale of the MMPI-2 and the validity scales of the TOMM. Specifically, strong inverse relationships were revealed between the F-scale and both the first trial (r = –0.574) and second trial (r = –0.620) of the TOMM. Although significant, these results suggest that only 33%–38% of the variance is shared between psychiatric symptom validity and cognitive validity outcomes. Conclusions: Findings suggest that although there seems to be some relationship between both report-based and performance-based assessment, unilateral exaggeration of either psychiatric or cognitive symptoms remains plausible. Still, as individuals endorse more psychiatric symptoms, there is likely to be some related decline in performance on cognitive measures.
P52. Longitudinal Analysis of Fractional Anisotropy in Patients With Mild Cognitive Impairment and Alzheimer's Disease
Milap A. Nowrangi, Michelle Mielke, Kenichi Oishi, Gwenn Smith, Marilyn Albert, Susumu Mori, Constantine G. Lyketsos
Background: Diffusion Tensor Imaging is a method of assessing brain white-matter integrity. Specifically measuring fractional anisotropy (FA) and mean diffusivity has shown differences between normal controls (NC) and those with Mild Cognitive Impairment (MCI) and Alzheimer's Disease (AD) cross-sectionally. There have, however, been few attempts at characterizing changes in FA and its discriminatory ability longitudinally. Objective: The goal was to describe changes in FA over time in patients with MCI and AD, hypothesizing that reductions in FA in the anterior cingulum and fornix would discriminate between subject groups. Methods: A total of 75 subjects (25 NC, 25 amnestic MCI, 25 AD patients) received both imaging and clinical evaluations at baseline, 3, 6, and 12 months. For the analysis, eight regions of interest were generated a priori from four fiber tracts: fornix, cingulum bundle, splenium, and the cerebral penduncles (control region). Results: Mean FA was lower (p<0.05) in AD cases than NC in the anterior cingulum, fornix, and splenium, but not between NC and MCI or between MCI and AD at 3, 6, and 12 months. Decreases in FA within the AD group were most apparent in the fornix, but not the splenium or cingulum bundle. Conclusions: Cross-sectional relationships between FA and diagnostic group are consistent over time and appear to be able to discriminate NC from AD in specific white-matter tracts that are implicated in the known pathogenesis of AD. There was little longitudinal change within diagnostic groups. Additional analyses will need to focus on subgroups of converters/progressors.
P53. Changes in Motor Evoked Potentials Associated With Fatigue Are Related to Central Motor Initiation
Candace Palmer, William Triggs, M.D., Benzi Kluger, M.D., M.S.
Background: Previous research shows a transient decline in transcranial magnetic stimulation-induced motor evoked potential (MEP) amplitude after fatiguing motor activity. However, the specific neuroanatomical location and neurophysiological cause of this MEP amplitude change is unknown. Objective: To determine whether changes in MEP are specifically associated to task-related motor cortical areas and to assess whether task demands affect these changes, hypothesizing that MEP changes were related to repeated central initiation of motor commands in task-related cortex. Methods: Twenty healthy adults had MEPs measured from the dominant hand area of motor cortex before and after six different tasks: rest (no activity), contralateral fatiguing hand grip, ipsilateral fatiguing hand grip, contralateral finger-tapping, ipsilateral finger-tapping, and imagined hand grip (motor imagery). Changes in MEPs from baseline were assessed for each task immediately after the task and at 2-minute intervals until MEPs returned to a stable baseline. Measures of subjective effort and behavioral fatigue (change in grip force or tapping speed) were also recorded. Results: A statistically significant drop in MEP amplitude was noted only with contralateral finger-tapping and imagined grip. Changes in MEP amplitude did not correlate with subjective fatigue, effort, or objective changes in performance. There was no significant change in motor performance in the finger-tapping task despite the MEP change. Conclusion: This study extends our knowledge of observed decline in MEP after certain tasks. Our experiments suggest that central initiation of motor programs, particularly repetitive actions, may induce an MEP amplitude change even without objective fatigue.
P54. Prevention of Anxiety Disorder After Stroke
Robert G. Robinson, Katsunaka Mikami, Mijin Jang, Ricardo E. Jorge
Background: Anxiety disorders meeting DSM-IV symptom criteria for generalized anxiety disorder (GAD) are found in ∼22% of patients with acute stroke. In half of these patients, depressive disorder is comorbid with GAD. Anxiety disorder, without depression, occurs in ∼10% of patients with acute stroke. Objective: This study examined the ability of escitalopram or problem-solving therapy (PST) to prevent new onset of GAD. Methods: Patients within 3 months of an index stroke not meeting DSM-IV diagnostic criteria for major or minor depression or GAD and without serious comorbid physical illness were eligible; 149 met inclusion criteria and were randomized to double-blind treatment with escitalopram (10 mg) for patients ≤65 years and 5 mg for patients >age 65; n=47) or placebo (n=49) or non-blinded PST (12 total sessions; n=54) over 1 year. At 3, 6, 9, and 12 months, patients were assessed for GAD, using the SCID for DSM-IV diagnosis. Results: There were no significant differences in background characteristics among the three groups. Using a Cox proportional-hazards model of time-to-onset of poststroke GAD, patients given placebo were 4.7 times more likely to develop GAD (9 cases) than patients given escitalopram (3 cases) after controlling for age, gender, previous history of GAD, and severity of impairments of activities of daily living (hazard ratio [HR]: 4.7; 95% confidence interval [CI]: 1.6–13.5; p=0.004). Patients given placebo were 4.2 times more likely to develop GAD than patients given PST (3 cases) after controlling for the same variables as the previous analysis (HR: 4.2; 95% CI: 1.8–9.8; p=0.001). Conclusion: Both escitalopram and PST were effective in preventing new onset of GAD during 1 year following stroke.
P55. A Case Report of Abnormally Small Hippocampi in a Patient With Mild Traumatic Brain Injury
David Ross, Alfred Ochs, Jan Seabaugh, Tim Henshaw
Background: Although group studies of patients with traumatic brain injury (TBI) have shown clearly that patients suffer brain atrophy after injury, traditional interpretation of MRI brain images by neuroradiologists have relied upon qualitative visual inspection of the images and often are read as normal or having nonspecific findings. Authors report on such a case in a patient with mild TBI who had volumetric analysis in addition to the traditional MRI interpretation. Case History: The patient was a 57-year-old man who was in a motor vehicle accident in June 2009, leading to mild TBI and musculoskeletal injuries. A 3.0-Tesla MRI was interpreted in the standard fashion (by visual inspection) as showing two nonspecific T2 white-matter hyperintensities in the left frontal lobe. NeuroQuant, an FDA-approved, commercially available software method, was used to analyze the MRI brain volume. Results: The results showed that the patient had abnormally small hippocampi (4.37 cm3; <1st percentile) as compared with normal controls. On neuropsychological testing, he had impaired performance on a test of immediate recall when an interference list of words was introduced (2nd percentile, as compared with normal controls). Conclusions: The patient had evidence for abnormally small hippocampi, detected with a quantitative volumetric technique, but not observed with traditional radiologic interpretation. The hippocampal atrophy was consistent with impaired immediate recall. NeuroQuant is a readily available and convenient technique for measuring brain volume, which complements traditional interpretation of MRI images, and, in some cases, it may provide the only available objective evidence of brain injury.
P56. Self-Administered Screening Uncovers Mild Cognitive Impairment and Dementia Among Community-Dwelling Seniors
D.W. Scharre, S.-I. Chang, A. Levin, H.N. Nagaraja
Background: The Self-Administered Gerocognitive Examination (SAGE), a cognitive assessment tool with four equivalent forms, is used to identify Mild Cognitive Impairment (MCI) and early dementia. Objective: To utilize the self-administered SAGE in community settings to quickly and simultaneously screen many seniors to detect MCI and dementia and enhance their recruitment into clinical trials. Methods: Subjects at a wide variety of community-outreach events completed the SAGE. Based on previously published validity data, SAGE test scores of 17 to 22 are suggestive of a normal condition; 15 and 16, of MCI; and <15, of a dementia condition. Participants were given their SAGE result with an explanation sheet. Further evaluation by a physician for scores <17 was recommended. Results: Of 654 individuals over 50 years old (mean age: 73) screened with SAGE, 70% were female, 10% minority, and 59% college graduates. Based on their SAGE score, 70% were classified as normal, 10% as MCI, and 20% as dementia. Higher age, lower education, history of stroke, and difficulties doing everyday activities due to thinking problems were associated with lower SAGE scores (all p<0.05). No association was noted between SAGE score and gender, subjective memory complaint, depression symptoms, personality changes, or different SAGE forms. Conclusions: Using SAGE, large numbers of individuals were screened very quickly in varied community settings. MCI and dementia were identified in 30% of these seniors. This may be tremendously helpful in promoting early evaluation and diagnosis by their primary-care physician and in assisting recruitment for cognitive research studies.
P57. A Rare Case of Breast Cancer in a Male Patient on Long-Term Atypical Antipsychotics
Lokesh Shahani, M.D.
Background: Breast cancer is an uncommon malignancy in men. Elevated prolactin level has been hypothesized to be the responsible for the increased risk of breast cancer in men. Atypical antipsychotics are currently used for long-term treatment in a vast number of patients with psychiatric illnesses. Endocrine abnormalities, including hyperprolactinemia, are commonly-encountered adverse effects. Prolactin elevation induces breast cancer cell proliferation and inhibits apoptosis. Case History: We report on a White male patient with schizoaffective disorder on various atypical antipsychotic agents for the past 5 years. During a hospitalization for his psychiatric condition, the patient complained of a painless mass in his right breast over the past 6 months. Breast ultrasonography revealed a right-sided 3.5-cm irregular mass with evidence of axillary adenopathy. The patient underwent a core biopsy of his breast mass, which showed invasive ductal carcinoma of the right breast. Conclusion: Studies show increased risk of breast cancer among patients on medications with dopamine-antagonist properties, such as antipsychotics and antiemetics. Breast cancer screening is sometimes ignored in patients with severe psychiatric illnesses. With increased risk factors such as antipsychotic agents, smoking, and obesity in this population, routine screening is required. This will contribute to the early diagnosis and treatment of breast cancer.
P58. Antibiotics-Induced Psychosis: Updates on Tetracycline
Lokesh Shahani, M.D.
Background: Antibiotics with good central nervous system (CNS) penetration are known for their neurological side effects. Psychosis is a severe CNS side effect and is associated with cephalosporin, macrolide, and fluroquinolone groups of antibiotics. Authors report on two patients who required hospitalization secondary to psychosis resulting from the use of the tetracycline group of antibiotics. Case History: The first patient is a 56-year-old woman who was prescribed doxycycline for mild cellulitis of her left forearm. The patient was bought to the emergency department by her husband with complaints of visual hallucinations 3 days after initiation of doxycycline therapy. The patient was admitted to the psychiatric unit, and doxycyline was discontinued. The patient spontaneously recovered within 24 hours of stopping doxycyline. The second patient is a 43-year-old man who was prescribed tigecycline for osteomyelitis of his left tarsal bone. The patient was discharged on the third day of antibiotic therapy. He presented to the emergency department with paranoid features the next day. The patient was admitted, and his tigecycline was switched to daptomycin. The patient required two doses of haloperidol, and his psychosis resolved on Day 3 of hospitalization. Conclusion: With the emergence of multidrug-resistant nosocomial pathogens, tetracyclines have started gaining importance. There has not been any published report of psychosis associated with the use of tetracycline antibiotics. Our cases contribute to the literature and should increase physician awareness of the side effects to monitor and the need to educate patients when prescribing tetracycline antibiotics.
P59. Temporal Lobe Epilepsy: Revisiting Gastaut-Geschwind Syndrome
Lokesh Shahani, M.D.
Background: Investigators have long recognized the neuropsychiatric symptoms that can arise from temporal lobe lesion. Epileptic patients with temporal lobe foci are disproportionately prone to the Gastaut-Geschwind syndrome. Disorders of sexual function, hyperreligiosity, hypergraphia, exaggerated philosophical concerns, and irritability form the kernel of this syndrome. Case History: Authors report on a 38-year-old White man who was transferred to the hospital for acute mental status changes. The patient had been experiencing symptoms of mania, such as feeling euphoric, having increased goal-directed activity, requiring minimal sleep, and having racing thoughts. He was also having auditory hallucinations of the voice of Jesus and, furthermore, feeling that Jesus would take care of all his problems. His wife was concerned about his increased religious involvement; he had been continuously reading the Bible for the past 2 weeks. Further history elicited that in the past 2 weeks the patient had experienced three seizure-like episodes, which were followed by a period of post-recovery confusion. Patient's neurological work-up failed to elicit any specific cause for his seizures and mental status changes. The patient was started on valproic acid along with an atypical antipsychotic. His mood symptoms improved, and he did not experience any more seizures while he was in the hospital. Conclusions: There have been reports of psychiatric problems that are associated with limbic auras in patients with epilepsy. These data support neuropsychiatric changes seen in patients with epilepsy. They highlight the significance of cortico-subcortical connectivity in the expression of abnormal emotional behavior.
P60. Utilization of a Comprehension Assessment to Confirm Informed Consent for Research in Depressed Patients Who Have Started Electroconvulsive Therapy
C.L. Sola, D.O., M.I. Lapid, M.D., L.R. Seymour, CCRP; E.J. Scilley, CCRP; M.A. Frye, M.D.
Background: Verification of consent comprehension is vital in depressed research patients receiving ECT, as both illness and treatment can hinder understanding. Objective: To ensure that depressed research patients demonstrated sufficient understanding of a study and could provide informed consent even after receiving ECT treatment. Methods: 22 subjects were medically cleared to participate in the IRB-approved study “Acceleration and Relapse Prevention with Triiodothyronine as an Adjunct to Electroconvulsive Therapy.” Subjects verified orientation, and answered six True/False questions to clarify understanding of the presence of a placebo control, the timing of study medication and visits, and risks and benefits of enrollment. Questions answered incorrectly prompted the query for clarification by asking “Can you explain what you mean?” The final two questions were interpreted correctly as either true or false, depending upon the explanation provided by the subject. All subjects demonstrated clear comprehension of the study details by answering all questions correctly. Results: 22 depressed subjects (13 women) were enrolled, 19 with unipolar depression and 3 with bipolar. The mean symptom severity score on the 24-item Hamilton Rating Scale for Depression was 32.91 (±7.68). Average motor seizure duration for the first ECT was 55.18 seconds (±41.03), with a mean EEG seizure of 75.91 seconds (±46.43). All 22 subjects completed the comprehension assessment with 100% accuracy. Conclusions: This comprehension assessment provided assurance of informed consent for even severely depressed patients already pursuing a course of ECT for unipolar or bipolar depression.
P61. OEF/OIF Veterans With Mild TBI Following Exposure to Primary Blast Forces: Neurological Soft Signs
Katherine H. Taber, Susan D. Hurt, Kimberly B. Gordon, Robin A. Hurley
Background: A recently published study of psychiatric inpatients evaluating the relationship between total score on a short neurological soft signs (NSS) examination and presence/absence of a history of mild traumatic brain injury (mTBI) reported a high sensitivity and specificity, and suggested that NSS might be useful in screening for mTBI in military personnel. Objective: Data from an ongoing blast injury study was used to test the potential usefulness of NSS in differentiating veterans with and without combat-related mTBI. Method: NSS examinations were compared from groups of post-deployment veterans who differed on presence/absence of psychiatric diagnoses and mTBI. Results: Veterans without TBI or any psychiatric diagnoses had an average total score of 1.3, and 22% of the group were abnormal on more than two items; veterans with PTSD but without TBI had an average total score of 1.4, and 23% of the group were abnormal on more than two items; Veterans with both PTSD and mTBI had an average total score of 2.3, and 33% of the group were abnormal on more than two items. Conclusion: The presence of NSS was low in all groups, and no group was specifically elevated on any particular item. No member of any group had more than one primitive reflex present. The preliminary results do not support the usefulness of NSS for clearly identifying individuals with combat-related mTBI. These differences in results are likely due to the populations studied, which differed in multiple ways, including age, time since TBI, injury mechanisms, and psychiatric issues.
P62. Maine Infants-at-Risk Project
Paul Tisher, Jonathan A. Paul, Beth A. Matano, Ramesh Krishnan, Nicole Heller, Mark Brown, Marie J. Hayes
Background: Over the last decade, Northeastern Maine has suffered a serious prescription-opiate epidemic. The present study examined infant outcomes in low-SES, opiate-dependent, pregnant women from a hospital-based methadone clinic. Objective: The goal was to determine the impact of substance abuse on newborn development and the effects of management via traditional Narcotics Treatment Program (NTP) clinic. Methods: Sleep was assessed in hospital via actigraphy and videography. Infant neurocognition, using the auditory oddball paradigm event-related potential (ERP), was measured at 1 and 7 months of age. Bayley Scales of Infant Development were administered at 9 months of age. Maternal biologic and clinical assessments of polysubstance use and psychopathology were determined during pregnancy. Results: Abnormal ERP and sleep fragmentation were associated with later admission to the narcotic treatment program (NTP) and prenatal physiologic anxiety. ERP and Bayley Scale deficits were associated with maternal alcohol use during pregnancy. Our previous work has reported s a relationship between alcohol consumption during pregnancy, SF, and reduced REM sleep. Conclusion: Women who abuse opiates have rates of alcohol abuse similar to low-SES groups. Opiate abuse during pregnancy and maternal anxiety were associated with newborn sleep abnormalities and neurocognitive performance. ERP and Bayley Scales were similarly adversely affected by prenatal alcohol. Admission to NTP as early as possible is clearly beneficial, but polysubstance abuse cannot be ignored. Programs should address this problem. Both SF and abnormal ERPs suggest delayed development of the CNS and potential problems with learning.
P63. Longitudinal Study of Delirium Phenomenological and Neuropsychological Profile Using Mixed-Effects Regression Modeling
Paula T. Trzepacz, M.D., Maeve Leonard, M.D., Claire Jordan, Jean Saunders, David J. Meagher, M.D.
Background: Delirium is a state of impaired consciousness and information-processing, with inattention as a cardinal symptom. The trajectory of individual delirium symptoms during an episode is not well studied. Objective: To study the longitudinal course of phenomenology during an episode of delirium, with detailed assessment of which symptom severities fluctuate over time. Method: Bi-weekly assessments of patients with DSM-IV delirium in a palliative care unit at the University of Limerick Medical School, Ireland, using the Delirium Rating Scale-Revised–98 (DRS-R98), Cognitive Test for Delirium (CTD) and Delirium Etiology Checklist (DEC). Mixed-effects regression modeling (MRM) was used to calculate change in individual symptom severities. Results: 100 patients (mean age: 70.2 ±10.5; 51% men; 27 with comorbid dementia) underwent a total of 323 assessments (range: 2–9/case), with reasons for discontinuing: death (55), recovery (30), declined (12), discharged (3). Comorbid cases did not differ from delirium-alone on age, assessment number, sex, or etiology. DRS-R98 attention, sleep–wake cycle disturbance, and thought disturbance, and CTD attention, comprehension, and vigilance were most frequent, consistent with being core domains. MRM slopes for DRS-R98 item severities across six visits were all less than 0.019, and only sleep–wake cycle disturbance, affective lability, and long-term memory had confidence intervals (not spanning zero) indicating statistical significance, even though these were not clinically significant. Conclusion: This is the first report that delirium symptom severities, using the DRS-R98, remain consistent during episodes until delirium resolves per DSM-IV criteria. This supports the idea that core features of delirium persist and suggests that highly-distributed neural networks supporting information-processing remain impaired until delirium resolves.
P64. Impulsivity, Apathy, and Executive Dysfunction in a Patient With Multiple Potential Etiologies
Sandeep Vaishnavi, Chad Forbes, Thomas Gualtieri
Background: Impulsivity, executive dysfunction, and apathy can be associated with various disease processes that affect the frontal lobe. Here, authors present a case of a patient who has multiple potential causes of damage to frontal lobe circuits and who presents a diagnostic challenge. Case History: The patient is a 63-year-old man who has a history of impulsive behavior from early life, including inappropriate touching while he was in a postdoctoral program. He is near bankruptcy because of impulsive spending and starting businesses without any plan. He has periods of excess energy and decreased need for sleep. He has suffered seven traumatic brain injuries, with the first one in infancy. He has also suffered from a left-frontal stroke, after which he and his family have noticed more problems with memory and attention. The patient also has a longstanding history of alcohol abuse and dependence. He has had increased apathy and nonchalance. He is not anosognosic about his behavioral changes. The patient has been repeating himself and has had short-term memory problems. On neurocognitive testing, he had mild problems with memory, but more significant problems with executive functioning. An MRI was obtained, which showed significant bilateral frontal and temporal atrophy. Conclusions: This case illustrates various potential causes for behavioral and cognitive changes and the dilemma of causality in neuropsychiatric patients. The differential diagnoses includes bipolar disorder, frontotemporal dementia, alchohol abuse, and effects of traumatic brain injuries. Understanding the complex interaction of these factors may help in fashioning an effective therapeutic plan for this patient.
P65. Attentional Impairment Does Not Predict Response to Phonological Awareness Treatment or Concomitant Improvement in Rapid Automatized Naming
Kimberly Ward, SLPA, Jill Gitten Aloia, Ph.D., Jean Riordan, Ph.D. Kytja K.S. Voeller, M.D.
Background: Both Rapid Automatized Naming (RAN) and Phonological Awareness (PA) are typically impaired in dyslexic subjects. ADHD is a common comorbidity of dyslexia and is associated with impaired performance on RAN. In a previous study on the treatment of dyslexia, the authors demonstrated that, after intensive treatments designed to enhance PA, RAN also improved significantly. The hypothesis underlying the current study was that subjects with impaired attention and slow reaction time (RT) would show less response to PA and little improvement in RN. Furthermore, psychostimulant treatment for ADHD would enhance response to PA. Methods: 41 subjects (ages 6–24 years) underwent PA and RN testing before and after intensive treatment. Data from a continuous performance test (CPT) was available on 40 subjects. Performance of the PA/RN “improvers” and “non-improvers” was compared, using Stimulus Detection, RT, and variability of RT for auditory and visual stimuli as variables. Statistical analyses included t-tests, correlational, and non-parametric measures. Results: PA improved from pre- to post-testing (paired t-test: t = –5.128; p=0.000); 93% of participants performed at or above baseline testing. RAN also improved from pre- to post-testing (t = –3.735; p=0.001); however, 27% of participants performed below baseline testing. CPT performance (attention, RT, and RT variability to visual and auditory stimuli) did not predict response to PA treatment or the improvement in RAN; medication had only a slight effect. Conclusion: Inattention, RT, and RT variability do not appear to influence response to intensive PA training.
P66. No Words for Feelings: The Emotional Word-Fluency Test
Josh Morris, B.A., Jill Gitten Aloia, Ph.D., Jean Riordan, Ph.D., Alex Masi, Kytja K.S. Voeller, M.D.
Background: Learning to regulate one's behavior requires the ability to express one's thoughts and desires in language and involves a lexicon of emotion to describe one's own feelings and categorize the feelings of others. Objective: To examine emotional word fluency (EWF) in children and young adults relative to other verbal fluency measures. Method: Authors evaluated 22 children and young adults for behavior and learning problems. After completing the D-KEFS Verbal Fluency task, subjects were asked to list “feelings and emotions,” and a 60-second sample was recorded. The number of emotion words relative to D-KEFS Category Fluency words (CFW) was examined; word lists were also examined for emotional valence and content. Results: An average of 9.35 ±2.9 emotion words were generated in 60 seconds versus 15.69 ±3.8 CFW). Subjects who performed poorly on the CFW task also had difficulty on EWF, but good performance on CFW did not predict good EWF performance. Several subjects who performed much better on CFW than EWF had significant and persistent social-emotional problems. Some subjects generated lists of words consisting almost exclusively of negative, dysphoric emotions; others included words that had little to do with emotion. One subject presenting with anger and aggression had a large left-frontal porencephalic cyst. His CFW was high-average, but he could generate only seven emotion words. Conclusion: EWF may involve different neural systems from CFW and may be a valuable tool in assessing the capacity for the regulation of emotion and social awareness.
P67. Neuropsychiatric Patients' Association (NPA)
Dr. Hugh Mirolo, Heather S. Watkins, Shauna Smith, Staci Stapleton, Natasha Willoughby, Kariah Noftle
Background: NPA is a non-profit organization founded in January 2008 by current Executive Director, Dr. Hugh Mirolo, as an offshoot of the province's only Neuropsychiatry Clinic. This unique association offers Canada's neuropsychiatric patients an opportunity to fill service deficits in the healthcare system. Objectives: 1) Neuroplasticity promotion via neurocognitive rehabilitation programs employing cognitive recreational activities; 2) Awareness and advocacy-creation regarding neuropsychiatric issues; 3) Therapeutic milieu-provision fostering spontaneous support among patients and families; 4) Scientific contribution through neuropsychiatry research; 5) Professional development through academic opportunities for students and NPA members; and 6) Liaison-establishment with various entities affected by neuropsychiatric issues. Methods: Modus Operandi: For Patients, By Patients. NPA operates under a non-traditional governance structure analogous to the “V” formation assumed by geese in flight. The “flock” is led by an Executive Director, with two levels of Coordinators, and General Members. Coordinators/Members, all of whom are neuropsychiatric patients or their relatives, shift “flight” positions according to level of functioning and ability. Personal growth is therefore fostered, while protecting members from physical/mental exhaustion. Results: Accomplishments: 1) Patients and community members reported benefits from NPA's member-run neurocognitive rehabilitation sessions; 2) Contacts with various community resources have begun to increase awareness regarding neuropsychiatric issues; 3) A self-support network was formed, creating cohesive ties among members; 4) A research committee was created, composed of NPA members and students involved in neuropsychiatric projects; 5) Academic opportunities were provided for research volunteers; 6) Numerous linkages were established throughout the community. Conclusion: Despite its recent establishment, NPA already plays an integral role in the health and well-being of neuropsychiatric patients in Canada.
P68. Successful Use of Right Ultra-Brief Electroconvulsive Therapy for the Treatment of Catatonia, Psychotic Depression, and Motor Fluctuations Associated With Advanced Idiopathic Parkinson's Disease
Nolan Williams, Carol Burns, Baron Short, Vanessa Hinson, Ziad Nahas
Background: Parkinson's disease (PD) is a movement disorder frequently associated with depression, psychosis, and, rarely, catatonia. Despite the effectiveness of electroconvulsive therapy (ECT) in treating concurrent mood and motor symptoms, clinicians are reluctant to use ECT in PD for fear of worsening cognitive deficits. Recent studies have shown that right-unilateral ultra-brief pulse ECT (RU-UBP) has a favorable side-effect profile, yet has never been reported in the treatment for PD. Case History: The authors present the case of a 77-year-old woman with a 10-year history of PD, with severe dyskinesia and motor fluctuations, who developed psychotic depression and catatonia. The patient received an acute course of RU-UBP ECT (Thymatron, Illinois). After 8 sessions, her catatonia resolved; her mood and psychotic symptoms remitted; and her dyskinesia and motor fluctuations reduced. She subsequently discontinued her dopamine agonist and halved her levodopa while continuing maintenance ECT. Worsening of her tremor was temporally associated with a drop in her mood, shaping the patient's ECT treatment strategy. Fourteen months later, the concurrent benefits on mood and motor symptoms continue, while there are no cognitive effects. Conclusions: This case illustrates the role of RU-UBP ECT in PD and catatonia. Authors discuss the functional neuroanatomy of mood and motor regulation, their overlap, and ECT's putative shared mechanism in modulating GABAergic and dopaminergic systems in both networks. Given its relatively benign negative effects on cognition, the interplay between motor and mood regulation, and the putative clinical efficacy, future randomized controlled trials of RU-UBP ECT in PD and comorbid depression are warranted.
P69. Cognitive Deficits After Breast Cancer Chemotherapy: A Case of Severe “Chemo Brain”
Michael Ziffra, M.D.
Background: Many patients treated with adjuvant chemotherapy for cancer report cognitive complaints after their treatment, a phenomenon referred to colloquially as “chemo brain” or “chemo fog.” The authors describe a previously high-functioning patient who experienced a significant subjective cognitive decline after chemotherapy for breast cancer. This case is noteworthy for the severity and chronicity of the “chemo brain.” Case History: The patient is a 56-year-old woman who was diagnosed with and treated for breast cancer 3 years ago. Her treatment included chemotherapy consisting of doxorubicin, cyclophosphamide, and paclitaxel. Shortly after starting chemotherapy, she began to experience significant subjective cognitive complaints. These complaints, which included problems with memory and attention, did not exist before her receiving chemotherapy and have caused significant disability. Neuropsychological testing (the results of which will be presented) did reveal a generalized decrease in cognitive efficiency; however a direct link between the chemotherapy and the patient's cognitive deficits could not be established. Several potentially confounding factors exist, including comorbid medical and psychiatric conditions, and the use of several psychotropic medications. Despite attempts to treat these symptoms, her deficits have not improved and continue to impair her daily functioning. Conclusions: This case illustrates that challenges are faced by clinicians working with patients who experience “chemo brain.” This phenomenon remains controversial because of the lack of data about how these cognitive deficits arise, and how to properly diagnose and treat them. Comorbid medical and psychiatric conditions can often complicate management.