Since the introduction of highly-active antiretroviral therapy (HAART), the population of HIV-infected individuals has become older because AIDS-related mortality has decreased substantially.
1 Currently, 11% of AIDS patients are living to be older than 50,
2 and, by 2015, it is estimated that more than half of HIV+ persons in the United States will be over 50.
3 HAART has had a positive effect on expected lifespan and has also decreased the proportion of individuals with HIV-associated dementia (HAD), the most severe form of HIV-Associated Neurocognitive Disorders (HAND).
4–8 Despite the decline in HAD, the prevalence of milder forms of HAND (e.g., asymptomatic neurocognitive impairment [ANI] and minor neurocognitive disorder [MND]) remains high.
4,7,9,10 Also, as people live longer with HIV/AIDS, the risk of developing neuropsychological (NP) difficulties associated with traditional neurodegenerative disorders (e.g., Alzheimer's disease) and/or the combination of neurodegenerative disorders and HIV increases.
2,8Neuropathologic markers, common in patients with neurodegenerative disorders, are more prevalent among older persons with HIV infection than those without HIV infection.
11–14 Specifically, Green et al.
13 found evidence of β-amyloid deposits in the frontal cortex of approximately 50% of HIV+ cases, predominantly in the neuronal soma and axonal processes, in a cohort that had a mean age of 44; some cases had extracellular plaques, and a few demonstrated deposits in blood vessels. Achim et al.
11 also found an accumulation of β-amyloid in HIV-infected persons ranging from 38 to 60 years old. These findings suggest that longer life expectancy in HIV could increase pathological aggregation of neuronal proteins that are associated with NP impairment. Another CNS complication that is associated with aging is reduction of cerebral gray-matter volume and neuronal density.
15 Studies using magnetic resonance spectroscopy (MRS) have also revealed neuronal damage in the frontal white matter and the basal ganglia of older HIV patients, as compared with seronegative control subjects.
16HIV-induced damage to neurons, associated with neurocognitive impairment,
17–19 is most likely mediated through indirect neurotoxic mechanisms. This neuron toxicity can cause synapto-dendritic damage, neuronal loss, astrocytosis, and microgliosis, which have been shown to be associated with HIV-associated neurocognitive disorders.
20–23Whether other age-related diseases and HIV combine to cause greater-than-anticipated NP impairment is not entirely clear.
2 Some studies have shown that HIV-infected individuals over the age of 50 have a significantly higher prevalence of HAND, as compared with younger individuals.
24–28 For example, age and HIV both contributed to impairment in event-based prospective memory (remembering to remember), even after controlling for possible confounding demographic, medical, and psychiatric factors.
29 Additive cognitive effects of aging and HIV have potential clinical and public health consequences, since cognitive impairment contributes to poor adherence to HAART.
29–31Neurodegenerative diseases such as Alzheimer's disease (AD) are thought to be at least partially inherited; for example, the apolipoprotein ε4 (APOE ε4) allele increases the risk of AD
32–35 and is associated with worse neurocognitive outcomes in those without AD.
36–38 As in AD, HIV subjects with at least one copy of the APOE ε4 allele have increased risk of developing HIV-associated dementia, which suggests that APOE ε4 increases HIV-induced damage to the brain.
26Capturing family history of dementia (FHD) via self-report is an inexpensive proxy for genetic markers known to increase risk of dementia. An advantage of FHD information is that it may detect familial neurodegenerative conditions for which genetic correlates or screenings are not available. Several studies have shown that simply having FHD places one at a higher risk of developing AD.
39–41 For example, one study showed that offspring of parents who both developed AD are at an even higher risk of developing AD themselves.
39 Another study established that FHD and age are important risk factors for developing AD.
41 Interestingly, Fox et al.
42 showed that persons with FHD show a measurable cognitive decline years before the onset of AD. Furthermore, studies have suggested an additive effect of FHD and APOE ε4 on age at dementia onset, risk of dementia development, and rate of cognitive decline.
43–45Since no studies have specifically reported FHD as a potential risk factor for HIV-associated neurocognitive disorders, we investigated whether NP functioning was worse among HIV-infected persons with FHD, versus those without such a history. If FHD is associated with NP impairment, we wanted to assess its strength in the context of other factors (e.g., HIV disease severity) known to be associated with HIV-associated neurocognitive impairment.
PARTICIPANTS AND METHODS
Subjects
We evaluated 1,106 HIV-seropositive (HIV+) men and women who were participating in the multisite CNS HIV Antiretroviral Therapy Effects Research (CHARTER) study of HAND at six U.S. academic medical centers. Family history of dementia (FHD) was captured with a free-response, self-report question. Only first-degree (i.e., biologic parent, sibling, or offspring) and second-degree (i.e., biologic grandparent, grandchild, uncle, aunt, nephew, niece, half-sibling) relatives were considered for this study, using the following interviewer-administered question: “Is there a history of neurologic illness in your family, such as Parkinson's disease, Alzheimer's disease (AD), Huntington's chorea, multiple sclerosis, epilepsy, etc.? If so, who, and was this from the maternal or paternal side of the family?”
Because some of the listed neurologic conditions do not necessarily cause dementia symptoms in all those afflicted, we chose to code persons as FHD-positive only if they responded that a family member was diagnosed with “dementia” or AD. Raters were trained to ask follow-up questions regarding the type of dementia, the specific afflicted family member (assuring that this was a biologic relative), and the degree of the relative, as defined above. When participants were unable to provide all of this information, cases were coded as not having FHD, making it less likely that we would confirm our hypothesis that FHD was associated with worse NP testing. Participants who were adopted and could not provide information about their family history were excluded. All participants completed this portion of the assessment before completing the NP testing described below.
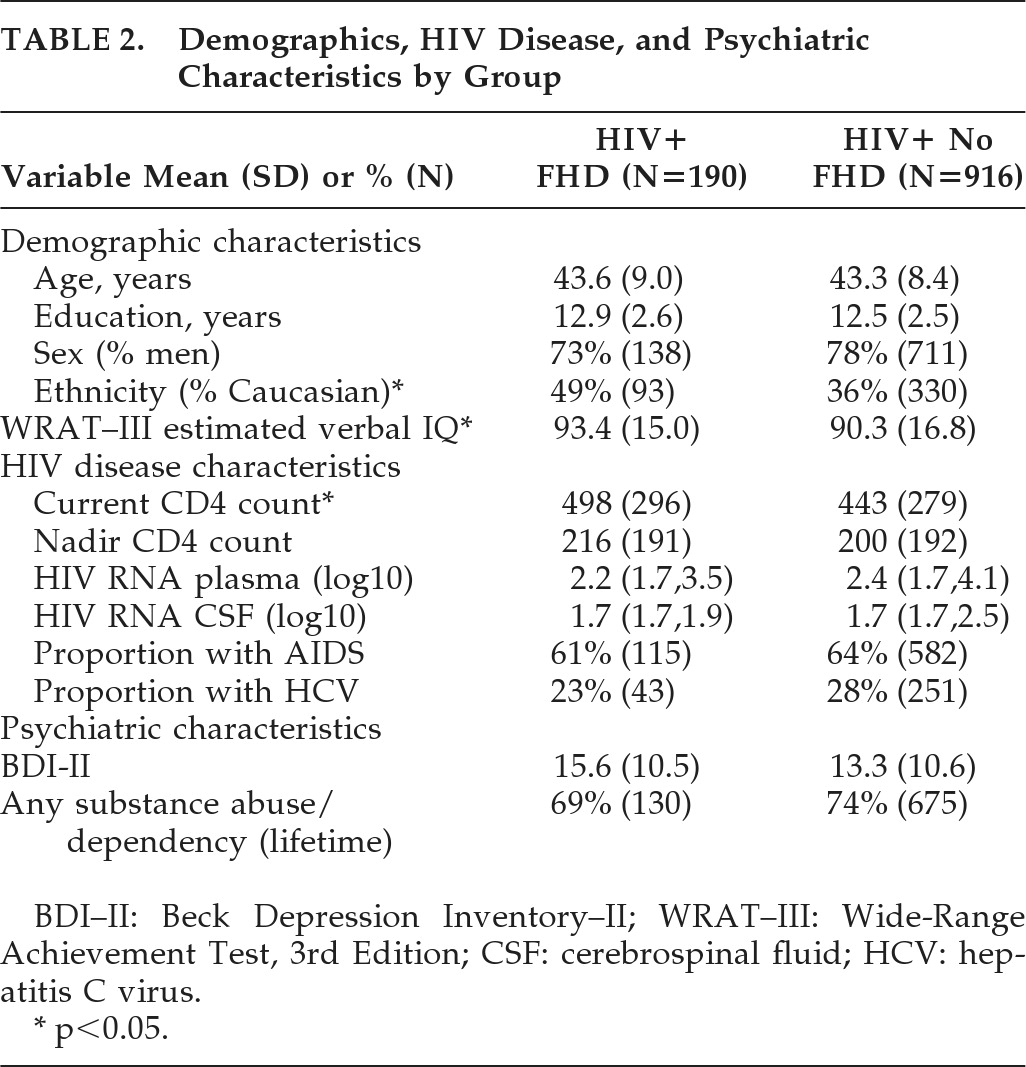
All participants completed a comprehensive NP battery designed to assess seven different NP domains: verbal fluency, executive functioning, speed of information-processing, attention/working memory, learning, memory, and motor skills. A list of each of the tests used to measure each of the NP domains is shown in
Table 1. This battery is the consensus NP battery for the CHARTER study and is widely used across other studies conducted at the HIV Neurobehavioral Research Center.
46Raw NP test scores were converted into T-scores (standard scores with a mean of 50 and standard deviation [SD] of 10), using demographically-adjusted norms to control for the effects of age, education, gender, and, where available, ethnicity.
47–49 These demographically-corrected T-scores were then summarized into a 0- to 5-point deficit scale that places an emphasis on impaired performance, with anything ≥0.5 indicating impairment. The deficit scores were derived by the following conversion: T>39: 0 (no impairment); T 35–39: 1 deficit point; T 30–34: 2 points; T 25–29: 3 points; T 20–24: 4 points; T<20: 5 points. Both domain deficit scores (DDS) and a global deficit score (GDS) were calculated by adding the deficit points of each contributing test and dividing it by the number of tests per domain or over the whole battery.
50–52 A GDS score ≥0.5 was used to define global NP impairment. DDS scores >0.5 defined domain-specific NP impairment.
A comorbidity status defining the level of non-HIV-related contribution to NP impairment (i.e., incidental, contributing, and confounding) was determined by a senior neuropsychologist (RKH), as described elsewhere.
53 We also assigned neurocognitive diagnoses, using an algorithm derived from a published report yielding excellent interrater reliability in previous multisite studies.
54 This algorithm conforms to the Frascati criteria for diagnosing HAND
55 and requires, for HIV-related neurocognitive diagnosis, the presence of mild impairment in at least two of the seven ability domains and the absence of significant confounding variables to be assigned. Depending on severity of impairment and impact on everyday functioning, the following diagnoses were assigned: asymptomatic neurocognitive impairment (ANI), mild neurocognitive disorder (MND), and HIV-associated dementia (HAD).
55 Persons with confounding comorbidity levels were assigned a diagnosis of neuropsychological impairment due to other causes (NPI–O).
Statistical Analysis
The comparison between the FHD and No-FHD groups used the Wilcoxon rank test for continuous variables (CD4 counts, estimated verbal IQ, GDS, DDS, etc.), and Fisher's exact test for binary variables (ethnicity, NPI–O diagnosis, NP impairment, etc.). Significance was defined when probability was less than a critical alpha of 0.05.
RESULTS
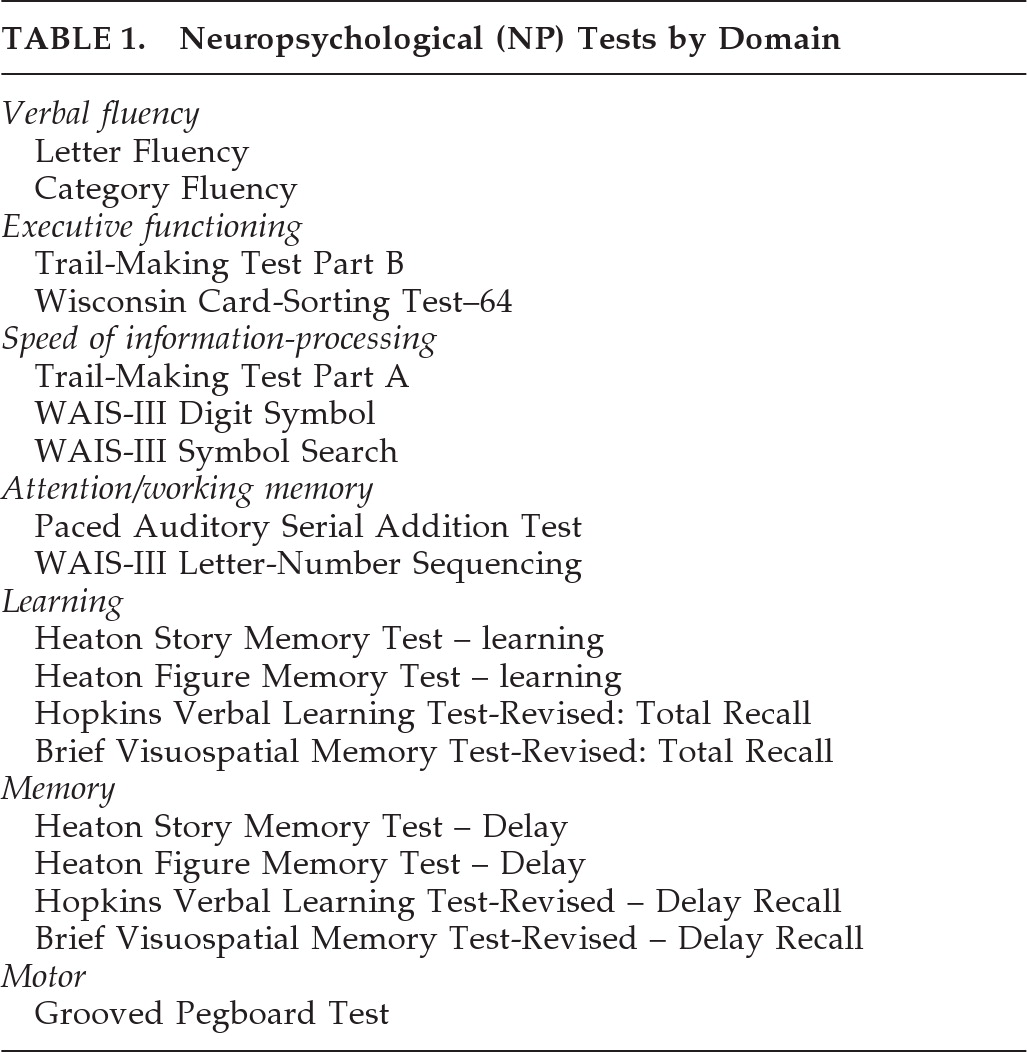
Table 2 shows that FHD-positive and -negative participants were similar in HIV disease-related and demographic factors, except that the FHD group had higher CD4 counts (Z=2.5; p=0.01), higher estimated Verbal IQ (VIQ: Z=2.2; p=0.03), and less ethnic diversity (Fisher's exact test: p<0.01).
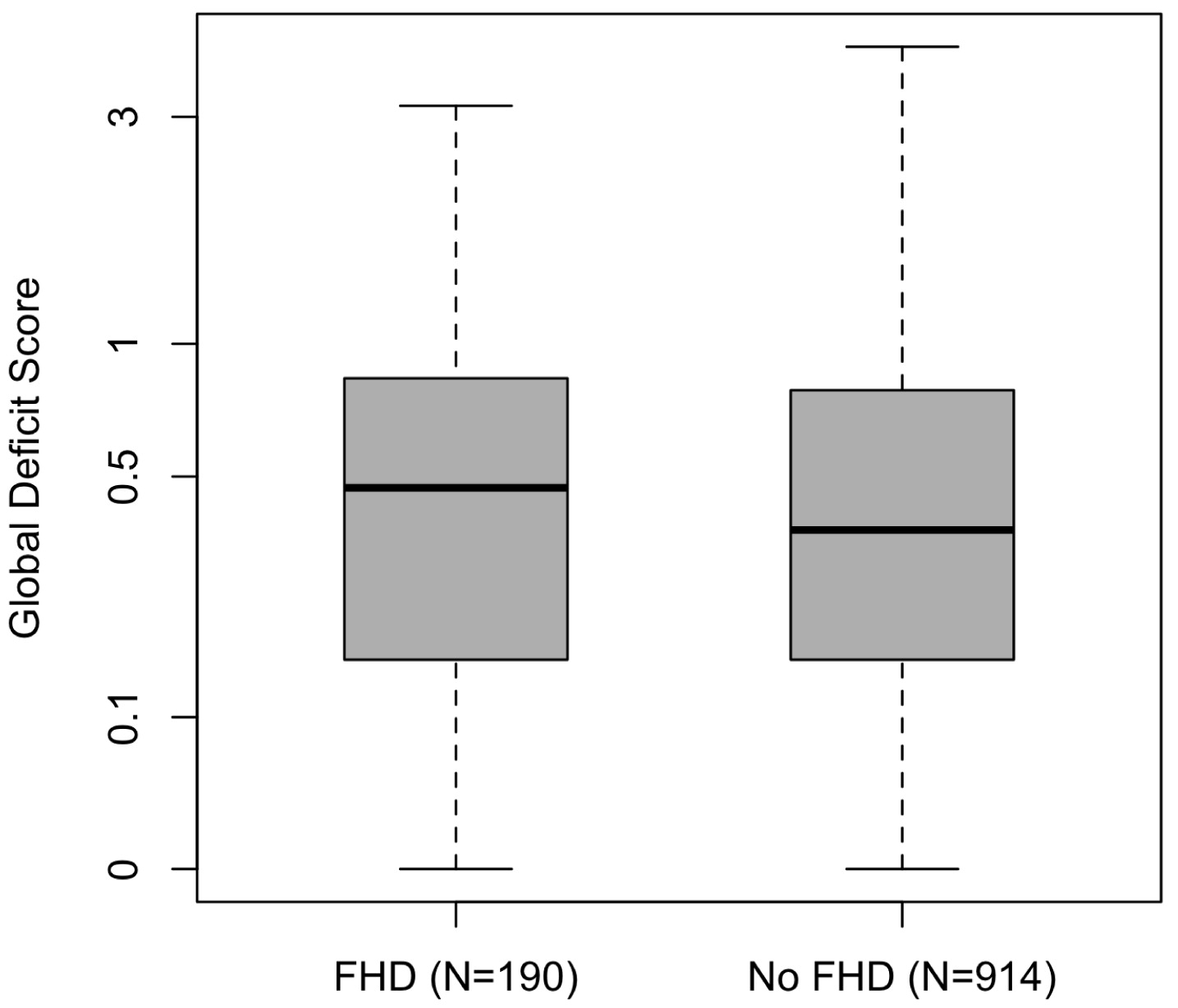
Despite having factors that are associated with better NP performance, such as higher CD4 counts and estimated VIQ, participants with FHD had significantly worse NP ability than those without FHD as measured by the GDS (FHD: mean=0.66 [SD: 0.64]; no-FHD: mean=0.55 [SD=0.56]; Z=2.0; p<0.05; Cohen's δ=0.18;
Figure 1).
Potentially confounding neuropsychological comorbidities were unrelated to FHD. To ensure that FHD and worse NP functioning were related in individuals with the fewest confounders, we analyzed the relationship, excluding those persons with confounding comorbidities. The FHD group still had worse global NP performance, with a slightly stronger effect size (FHD mean: 0.59 [SD=0.61]; No-FHD mean: 0.46 [SD=0.46]; Z=2.1; p=0.03; Cohen's δ=0.24). An overall chi-square analysis, grouping persons into HAND (i.e., ANI, MND, and HAD) versus non-HAND (i.e., NP-normal) was significant (Fisher's exact test: p<0.01), with 53% of the FHD group having a HAND diagnosis and 47% of the No-FHD group having a HAND diagnosis. Comparisons of individual HAND diagnoses by FHD versus No-FHD were not significant.
Persons who reported first-degree relatives with dementia were no more likely to be NP-impaired than those reporting second-degree relatives (persons who reported both first- and second-degree relatives were combined with those who reported first-degree relatives). Eighty-seven percent (87%) of participants in the FHD group reported one relative with dementia; 11%: two relatives; 1%: three relatives; 1%: four relatives. A higher number of self-reported relatives with dementia was not associated with additional risk of NP impairment.
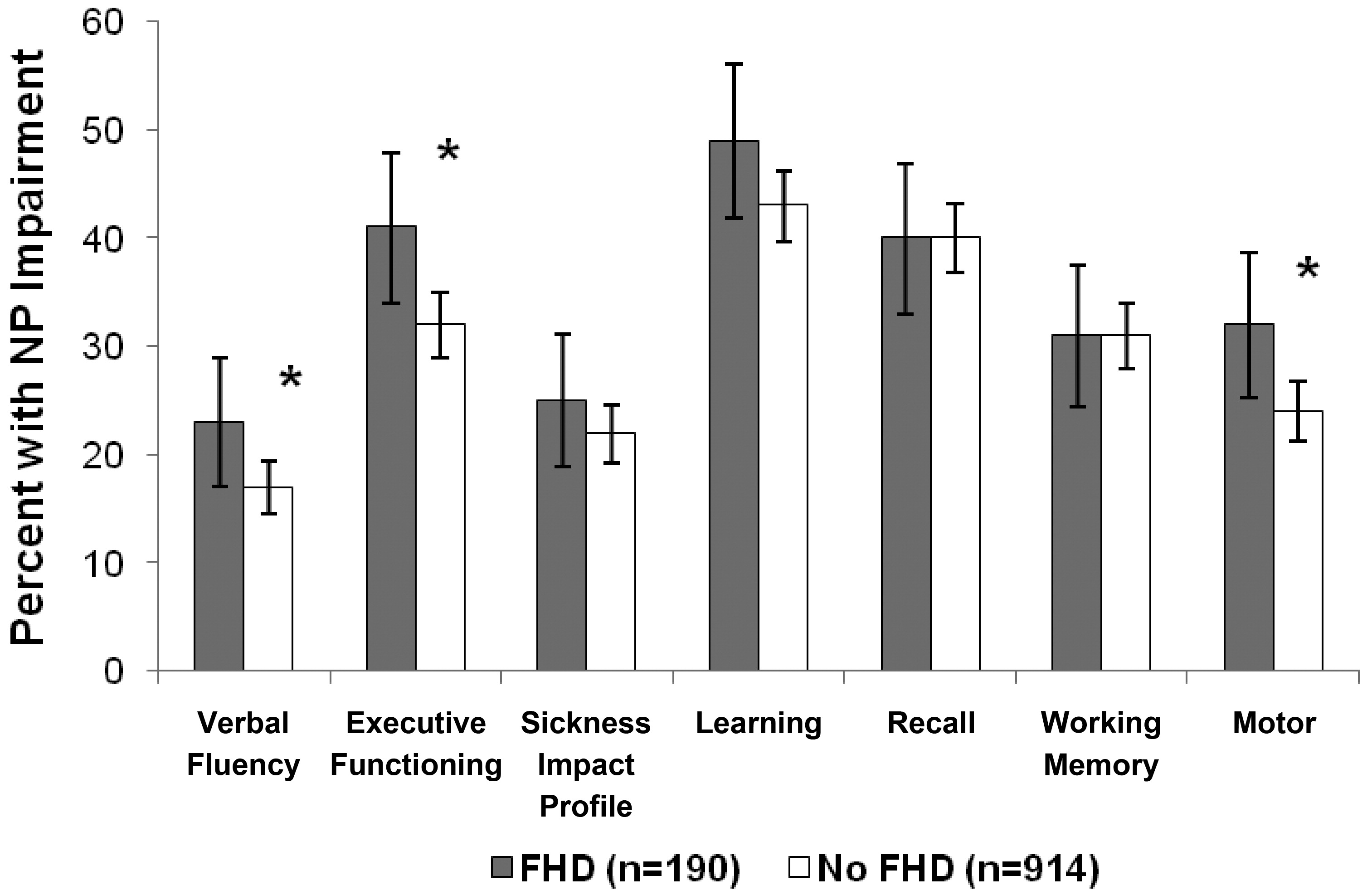
Analysis of impairment in each of the NP domains, defined as DDS scores >0.5, revealed that the FHD group was significantly more impaired than the No-FHD group in the domains of verbal fluency, executive functioning, and motor skills (
Figure 2).
DISCUSSION
HAND appears to arise from multifactorial interactions of human immunity, neurologic factors, HIV invasion and replication in the CNS, and comorbidities. FHD appears to be a surrogate for genetic factors that increase the risk of HAND, and, in this study, we observed worse neuropsychological functioning among HIV+ persons with FHD, versus those without FHD.
NP impairments were found in the domains of verbal fluency, executive functioning, and motor skills, cognitive capacities that are frequently damaged among HIV+ persons. Executive impairments are consistent with damage to frontal subcortical structures. Verbal fluency impairments in HIV are likely due to difficulties with the executive components of the task (e.g., switching to a new strategy when the current strategy is exhausted), rather than language skills.
56 A defining feature of most dementias is memory impairment, and we did not find differences in learning or memory between the FHD and No-FHD groups in this study. This finding might suggest that FHD lowers thresholds for the development of HIV-associated impairments and lessens the likelihood that these data represent a superimposed dementia on top of HIV-associated impairments. Clearly, additional research is needed to tease apart the potential contributions of these factors for neurocognitive outcomes.
Synapto-dendritic simplification in the frontal cortex has been shown to be associated with HIV-associated NP impairment.
20,21 Furthermore, subtle motor impairments can develop as a result of damage to basal-ganglia structures, which have also been documented to undergo HIV-associated synapto-dendritic simplification and to be associated with NP performance.
23 Damage to brain regions already affected by HIV and the associated NP impairments may mean that there is increased susceptibility among those with FHD. A potential mechanism is that HIV accelerates abnormal protein aggregation frequently found in AD, HIV, and other dementias.
11,13 Furthermore, individuals with FHD may have latent neurodegenerative conditions that HIV could accelerate by decreasing neuronal homeostasis.
Although family history had a small effect (Cohen's δ: 0.18 to 0.24) on level of NP impairment, it should be noted that our participants were relatively young (average age in mid-40s); it is possible that these effect sizes might be higher in older persons, consistent with the well-recognized age-dependency in evolution of neurocognitive decline related to neurodegenerative disease. As a post-hoc analysis, we examined our participants to see whether FHD had differential effects in older (i.e., >50) and younger (<40) HIV+ individuals. Analysis did not reveal any significant effect of FHD on NP functioning in the younger versus older groups.
It is curious that we saw a greater report of FHD among our Caucasian participants and those with significantly higher estimated VIQ scores and higher CD4 counts. All of these factors would typically be associated with better NP performance (although demographic corrections for ethnicity differences were applied); however, we observed the opposite: worse NP performance among those with FHD. One possibility is FHD participants with neurocognitive problems have become more aware of the cognitive problems of their family members and that the finding herein reflects this knowledge. Although possible, this hypothesis seems unlikely, given that participants provided FHD information before the formal NP testing in this study.
We have one of the largest sample sizes of any study of NP impairment in HIV+ persons; still, there are a few limitations. Ideally, a validated instrument should be used to diagnose FHD,
45,57 and corroborating evidence of FHD should have been sought from family members. Nevertheless, there were no obvious incentives or disincentives to report FHD to the study. In future studies, we will use a standardized questionnaire of FHD that asks in a systematic way about the family history of various dementias and neurodegenerative conditions. We also plan to study the relationship of FHD with other possible covariates for HAND, including genetic markers of dementia risk (e.g., APOE ε4).
Our study provides evidence that family history of dementia exerts a modest effect on likelihood that a person with HIV will have HAND. As the age of the population with HIV gradually increases with improved survival, FHD may be considered a convenient surrogate for one of several genetic risk factors for HAND. A positive screening for the presence of FHD may serve as a cue for clinicians to heighten the awareness for potential HAND among their HIV-infected patients.
Acknowledgments
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, nor the United States Government.
The CNS HIV Anti-Retroviral Therapy Effects Research (CHARTER) Study is supported by award N01 MH22005 from the NIH. The HIV Neurobehavioral Research Center (HNRC) is supported by Center award MH 62512 from NIMH. The San Diego HIV Neurobehavioral Research Center (HNRC) group is affiliated with the University of California, San Diego, the Naval Hospital, San Diego, and the Veterans Affairs San Diego Healthcare System.
The CNS HIV Anti-Retroviral Therapy Effects Research (CHARTER) group is affiliated with the Johns Hopkins University, Mount Sinai School of Medicine, University of California, San Diego, University of Texas, Galveston, the University of Washington, Seattle, WA; and Washington University, St. Louis, and is headquartered at the University of California, San Diego.