Major disasters, such as the terrorist attacks on the World Trade Center, require rapid assessment of individuals affected and triage to interventions in communities that are beset by chaos and major social disruptions. In such situations, access to clinicians who use the diagnostic gold standard set by the
DSM-IV (
1 ) may be the exception rather than the rule—hence the desirability of brief, standardized, easy-to-use tools that can be used by nonclinicians to identify individuals who, on the basis of presence of clusters of reactions to stress that approximate
DSM-IV criteria, may be especially in need of further assessment and treatment by mental health professionals.
Immediately after September 11, 2001, the New York State Office of Mental Health (NYOMH) conducted multiple needs assessments and cofunded surveys conducted by the New York Academy of Medicine to estimate the scope and duration of traumatic reactions related to and treatment needs stemming from the attacks (
2 ). In a survey conducted one to two months after the attacks, Galea and colleagues (
3 ) used the Diagnostic Interview Schedule to estimate probable attack-related posttraumatic stress disorder (PTSD) and depression as existing among 7.5 percent and 9.7 percent, respectively, of adults in lower Manhattan. In a subsequent survey by New York Academy of Medicine investigators, Galea and colleagues (
4 ) documented substantial declines (from 7.5 to .6 percent) in probable prevalence of PTSD, as defined by
DSM-IV, six months after the attacks, while estimating that 5.3 percent of the respondents continued to show symptoms consistent with subthreshold levels of PTSD.
Melnick and colleagues (
5 ) found that much higher proportions of adults surveyed in the greater New York City metropolitan area reported reactions of worry, sleep difficulties, and hopelessness (38 percent, 14 percent, and 8 percent, respectively) between one and two months after the attacks on the World Trade Center. For example, Schuster and colleagues (
6 ) used a modified PTSD checklist to assess stress reactions in a national sample. These investigators reported finding substantial stress reactions in 44 percent of adults, with 61 percent of adults living within 100 miles of the World Trade Center site reporting substantial traumatic stress reactions.
Twelve months after the terrorist attacks, continued emergence of trauma-related disorders was found. Preliminary findings from a survey conducted in September 2002 by the New York Academy of Medicine uncovered new-onset PTSD related to the attacks on the World Trade Center, where 5 percent of respondents without PTSD in March 2002 (most of whom were symptomatic but met only subthreshold criteria) met full criteria for PTSD in September 2002 (personal communication, Galea S, 2003).
In addition, psychological distress within a population after a major disaster is not limited to diagnosable disorders (
7 ). Marshall and colleagues (
8 ) found that subthreshold PTSD was associated with increased likelihood of comorbid major depressive disorder, suicidal ideation, and functional impairment, all of which increased linearly and significantly as a function of number of PTSD-related symptoms reported.
Project Liberty was the large-scale crisis intervention initiative funded by the Federal Emergency Management Agency (FEMA). Although there was a clear need to offer immediate support to enhance community coping with the terrorist attacks, evaluating longer-term need for services also was a priority. Such assessment of the psychiatric impairment of service recipients longitudinally over several years had not been conducted systematically after previous terrorist attacks. The overall aim of Project Liberty was to facilitate rapid return to predisaster functioning among the populace. About a quarter of New Yorkers were aware of Project Liberty, and those with probable current PTSD were more likely than those without these symptoms to say they would call Project Liberty (
9 ). Thus it is useful to know the extent to which Project Liberty service recipients had cognitive, emotional, behavioral, and physical event reactions that would map to approximations of
DSM-IV diagnostic groupings.
To monitor the geographic penetration of Project Liberty outreach and service delivery across the declared disaster area and to assess the demographic and clinical representation of Project Liberty service recipients compared with all residents of the disaster area, NYOMH adapted a form originally developed by the Center for Mental Health Services to track contacts between Project Liberty counselors and persons receiving crisis counseling. When completing the form, counselors indicated whether service recipients manifested any of 31 distress reactions. These distress reactions (hereafter, "event reactions") included the most commonly reported behavioral, emotional, physical, and cognitive responses postdisaster, including reactions associated with depression and posttraumatic stress. They also were used by counselors to document service provision and to aid decisions about referral of more distressed individuals to more intensive treatment.
This report augments syndrome-oriented population surveys by examining statistically the 31 psychological distress and impairment reactions reported by Project Liberty service providers to see what clusters of event reactions emerged and how those clusters align with DSM-IV diagnostic criteria. Information is also provided regarding the frequency of first-time use of these services by individuals who showed possible PTSD or major depressive disorder over the 27-month period in which the community-based Project Liberty program was active.
Methods
Variables and participants
Project Liberty services were provided by more than 175 community-based organizations in a wide variety of settings, as described by Felton (
10 ). Contracted service providers were paid to provide individual crisis counseling, educational services to groups, and group crisis counseling. Under FEMA funding conditions, all services provided under Project Liberty were anonymous; no participant names were reported. As an administrative requirement for reimbursement, providers were required to complete service encounter log forms for each contact, indicating date and location of service (such as a school or place of employment) and borough or county. For persons receiving individual counseling, service providers indicated whether the counseling contact was a first visit or a follow-up visit and provided demographic information (including gender, preferred language, and race or ethnicity, as observed by the counselor).
Logs included a record of the presence of up to 31 event reactions. Event reactions were categorized as behavioral (extreme change in activity level; excessive use of drugs, alcohol, or prescription drugs; isolation or withdrawal; hypervigilance; reluctance to leave home; and violent behavior), emotional (sadness or tearfulness, irritability or anger, feeling anxious or fearful, despair or hopelessness, feeling guilty or shameful, and feeling emotionally numb or disconnected), physical (headaches, stomach problems, difficulty falling or staying asleep, difficulty eating, worsening of chronic health conditions, fatigue or exhaustion, and chronic agitation), and cognitive (inability to accept or cope with the death of a loved one, distressing dreams, intrusive thoughts or images, difficulty concentrating, difficulty remembering things, difficulty making decisions, preoccupation with death, and suicidal thoughts or feelings). Each category also had items labeled other, unknown, and none. Counselors checked event reactions that were present. The Mount Sinai School of Medicine Institutional Review Board found that this project involved analyzing anonymous, secondary data and was therefore exempt from the board's review.
Statistical analyses
Hierarchical cluster analysis was performed on the 31 event reactions recorded for 465,428 logs of initial counseling sessions that occurred between September 2001 and December 2003. Because the event reaction data were coded as either present or absent, absolute binary phi 4-point correlations were used (the equivalent of a Pearson correlation between two dichotomous variables) to create clusters. Hierarchical cluster analyses first link the two variables that are most strongly correlated with one another and then join subsequent variables to a new variable or to an existing cluster on the basis of the strength of their correlations. This linking is done in a hierarchical fashion by entering larger correlations first and the smallest correlation last. Because each successive cluster is based on weaker associations, later clusters are less likely to comprise meaningful groupings. Moreover, event reactions that occur rarely (such as suicidal thoughts or feelings) have attenuated correlations and are thus less likely to be included in the clusters. SPSS 12.0 for Windows was used to conduct these analyses (
11 ). We conducted a hierarchical cluster analysis specifying between-groups linkage using an absolute phi 4-point correlation measure.
Results
Description of service users
Individual crisis counseling services were accessed by a broad spectrum of the population. Of the total sample, 91.0 percent (N=423,315) were adults, 97.5 percent (N=453,580) lived in New York City, 31.2 percent (N=145,198) were Caucasian, 30.1 percent (N=140,209) were African American, 25.3 percent (N=117,834) were Hispanic, and 52.9 percent (N=246,070) were women (
12 ). Rates of endorsement of event reactions ranged from 42.6 percent (N=198,382) for sadness and tearfulness to .6 percent (N=2,777) for suicidal thoughts or feelings.
Table 1 displays the numbers and proportions of service recipients who exhibited those event reactions. [An expanded version of this table is available at ps.psy chiatryonline.org and includes a 31×31 correlation matrix.]
Identification of event reaction clusters
Seven distinct clusters were identified from the 31 items. The weakest included a wide array of responses coded under "other" reactions in the behavioral, emotional, physical, and cognitive domains. This cluster was dropped from further discussion.
The two most statistically robust and coherent clusters included event reactions that resembled criteria for
DSM-IV diagnoses of major depressive disorder and PTSD (
1 ). The cluster that most closely resembled major depressive disorder (hereinafter referred to as "depressive episode cluster") contained ten items, seven of which matched major depressive disorder criteria listed in
DSM-IV: despair and hopelessness, feeling guilty or shameful, difficulty eating, fatigue or exhaustion, difficulty concentrating, difficulty remembering things, and difficulty making decisions. The three remaining items were isolation and withdrawal, feeling emotionally numb or disconnected, and stomach problems.
The cluster that most closely resembled PTSD (hereinafter referred to as "traumatic stress cluster") contained eight items, seven of which corresponded to DSM-IV criteria for the disorder: hypervigilance, reluctance to leave home, feeling anxious or fearful, difficulty falling or staying asleep, distressing dreams, intrusive thoughts or images, and preoccupation with death. The final item of the cluster was extreme change in activity level.
Two additional clusters were designated as aggression and grief clusters. The aggression cluster included violent behavior, irritability and anger, and chronic agitation, whereas the grief cluster included inability to cope with the death of a loved one, sadness and tearfulness, and headaches. The three remaining items—excessive use of drugs, alcohol, or prescription drugs; worsening of a chronic health condition; and suicidal thoughts or feelings—did not cluster with any of the previous four groups.
Next, hierarchical cluster analyses were conducted separately for different subgroups (for example, males only, females only, and African Americans only) to determine whether similar clusters would emerge. The depressive episode cluster consistently included nine of ten reactions found in the overall group (all but feeling guilty or shameful, which typically clustered with grief in the subgroup analyses). The traumatic stress cluster consistently included seven of eight reactions found in the overall group (all but preoccupation with death, which also typically clustered with grief). The clusters used in subsequent analyses included only the depressive episode cluster (nine items) and traumatic stress cluster (seven items).
Identifying increased risk for major depressive disorder or PTSD
Next, we calculated depressive symptom and traumatic stress scores for each service recipient on the basis of his or her score on these clusters. The rarely observed item on suicidal thoughts and feelings was added to the depressive episode cluster in order to include individuals who reported this rare but serious reaction. Thus depressive symptom scores could range from 0 to 10, whereas traumatic stress scores could range from 0 to 7. Resulting cluster scores were highly skewed, with a mean±SD of 1.18±1.46 (range=0-10; median=1.0) for depression and a mean of 1.64±1.50 (range=0-7; median=1.0) for traumatic stress.
Service recipients were also divided into two subgroups based on whether they had three or more event reactions within either cluster to identify individuals who likely fit Marshall and colleagues' (
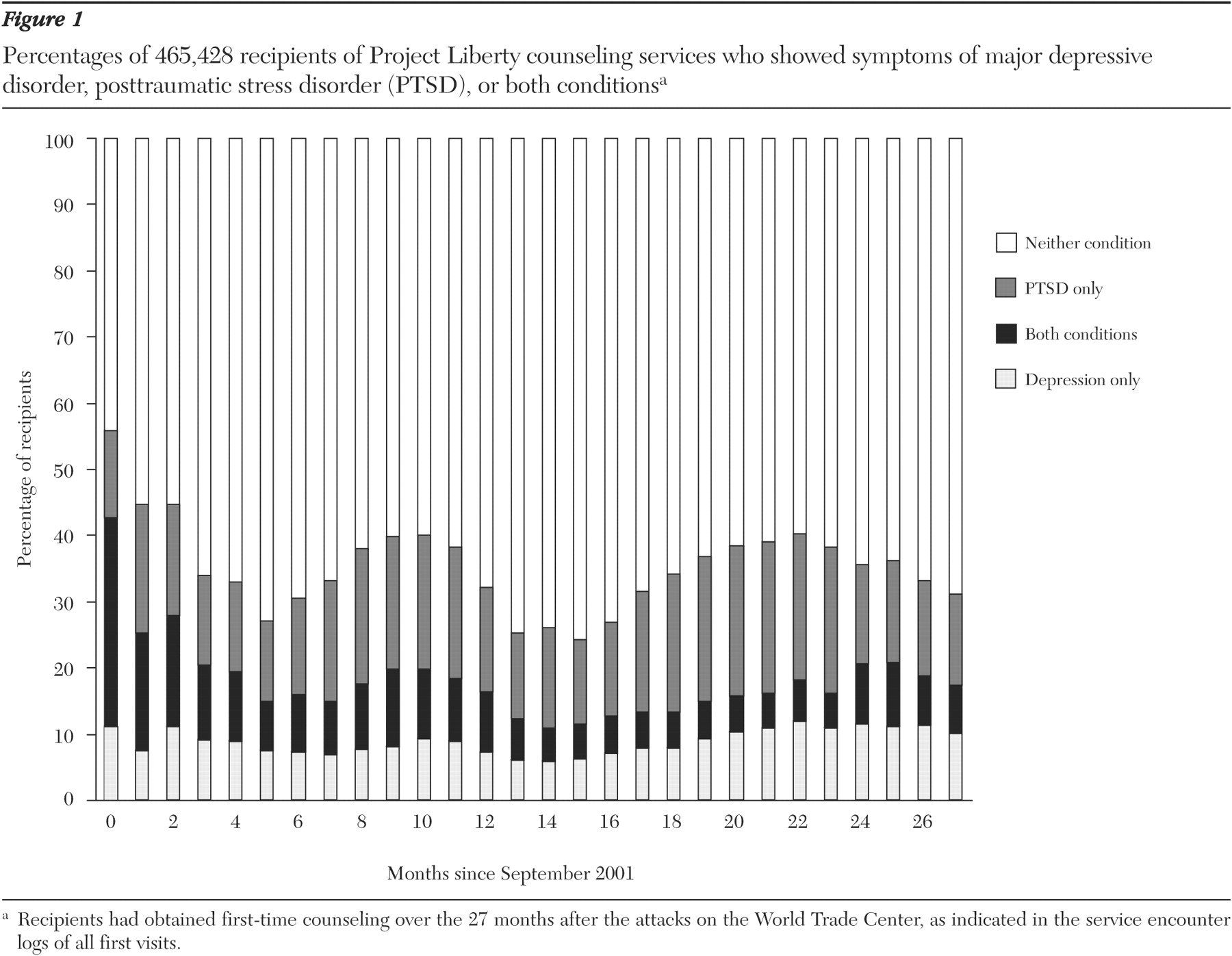
8 ) description for manifesting subthreshold conditions. The Marshall study reported significant linear increases in impairment as the number of endorsed symptoms increased from one to four. The presence of three symptoms was chosen to match the criterion that Marshall and colleagues set for defining subthreshold PTSD; 16 percent of recipients met these criteria for subthreshold or greater major depressive disorder, 26 percent for PTSD, and 8 percent for both. Although displaying three or more event reactions is not the equivalent of meeting full criteria for either of these diagnoses, the scores were used to show the pattern of morbidity for these syndromes over the first 27 months since the attacks. As illustrated in
Figure 1, individuals in all three of these groups sought first-time Project Liberty counseling on a relatively consistent basis for more than two years after the attacks on the World Trade Center.
Longitudinally, 55.8 percent (275 of 493 persons) of individuals receiving first-time crisis counseling in the first month after the attacks met our high-risk criteria for either one or both clusters. Percentages dropped across the next five months to a low of 27.1 percent (2,505 of 9,237 persons), then rose to a second peak of 40.1 percent (10,465 of 26,120 persons) at ten months. Percentages then dropped again in a linear fashion to 24.4 percent (5,681 of 23,307 persons) at 15 months, and peaked again at 40.2 percent (10,290 of 25,599 persons) at 22 months. The ten- and 22-month peaks correspond to anticipation of the first-year and second-year anniversaries of the attacks on the World Trade Center.
Discussion
The immediate psychological consequences of the September 11 attacks were widespread and detrimental. Residents within the greater New York metropolitan area reported symptoms indicating pervasive traumatic stress, depression, grief, and anger (
3,
13 ). Project Liberty counselors provided services to hundreds of thousands of recipients. In the course of providing these services, counselors completed service encounter logs that included checklists for cognitive, behavioral, emotional, and physical distress. These checklists formed a simple assessment tool, far short of a complete diagnostic assessment using
DSM-IV criteria but amenable to documenting event reactions and services carried out under extraordinarily difficult conditions.
Cluster analyses indicated that the event reactions clustered in groups consistent with criteria for major depressive disorder and PTSD. The presence of three or more event reactions permitted identification of individuals at particular risk for experiencing PTSD (
8 ), depression, and associated functional impairment. These higher-risk individuals represented about half of the first-time recipients of Project Liberty counseling services, a number that is substantially higher than was seen in several population-based surveys conducted six to 12 months after the attacks on the World Trade Center. These surveys (
4,
9 ) suggested that most of the New York populace returned to predisaster functioning within six months after the attacks.
The presence of multiple event reactions likely overestimates diagnostic syndromes of PTSD and major depressive disorder compared with DSM-IV criteria. Furthermore, hierarchical cluster analysis is an exploratory tool; hence the results presented here should be treated as tentative. Nevertheless, it is noteworthy that 26 percent, 16 percent, and 8 percent of Project Liberty crisis counseling service recipients had event reactions suggestive of at least subthreshold PTSD, depression, or both conditions, respectively. Taken together, these individuals represented more than 40 percent of Project Liberty service recipients throughout the 27-month period. Individuals with these clusters of event reactions continued to seek access to Project Liberty counseling services in a fairly steady stream for more than two years after the terrorist attacks, with spikes occurring near the first and second anniversaries of the attacks.
Also of considerable interest, these data are consistent with related findings (
12 ) that men and people of racial and ethnic minorities used Project Liberty services at a higher rate than is typical for traditional mental health services. Thus Project Liberty served as an accessible venue for short-term services for individuals with possible PTSD and depression as well as a portal of entry to standard mental health treatment (
14 ).
These results have implications for future crisis services and for ongoing public mental health services. A simple event reaction rating tool can be completed by lay crisis counselors who are responding to disasters. Such a tool can both assist counselors in providing services and referrals and provide administrators with useful data regarding the scope of the problems that such programs must address. Information recorded by nonclinicians can be clustered into meaningful diagnostic categories that, in turn, help identify pockets of need under circumstances where full clinical evaluations would be cost prohibitive.
Conclusions
Although hierarchical cluster analysis is an exploratory tool with associated limitations, our findings indicate that a large proportion of recipients of disaster-related crisis intervention showed reactions consistent with at least subthreshold DSM-IV diagnostic criteria. Our results have implications for future crisis interventions after terrorist attacks and for public mental health services. A simple checklist of possible event reactions, completed by nonclinicians, may be a useful way to identify individuals experiencing reactions consistent with PTSD and major depressive disorder. Event reaction clusters identifying subthreshold or possible PTSD and major depressive disorder were consistent across men and women and people of differing ethnicities, supporting the validity of the clusters. Having counselors note these 31 event reactions as part of completing routine service encounter logs can be a relatively inexpensive way to help with decisions about what care is needed. Identifying individuals with three or more of these event reactions permitted easy identification of Project Liberty service recipients who had a greater likelihood of having impairment consistent with PTSD or major depressive disorder.
The consistent proportion of individuals with possible PTSD and major depressive disorder seeking first-time Project Liberty counseling over the 27 months after the attacks suggests the need to ensure that such counseling services remain available for prolonged periods after disasters.
Acknowledgments
This evaluation was funded by grant FEMA-1391-DR-NY (titled "Project Liberty: Crisis Counseling Assistance and Training Program") to New York State from the Federal Emergency Management Agency. The Center for Mental Health Services of the Substance Abuse and Mental Health Services Administration administered the grant. The authors express their appreciation to Katherine M. Shear, M.D., Nancy H. Covell, Ph.D., and Sue Marcus, Ph.D.