It has been well established that psychiatric patients are at an elevated risk of mortality compared with individuals in the general population (
1,
2,
3 ). It is also clear that individuals with substance use disorders have a higher risk of mortality relative to individuals in the general population (
4,
5,
6 ). However, despite the high prevalence of substance use disorders among psychiatric patients (
7 ), there has been relatively little systematic study of the contribution of co-occurring substance use disorders to mortality among psychiatric patients. A better understanding of this relationship could suggest possible secondary prevention strategies to reduce death among psychiatric patients with co-occurring disorders.
Many prior studies that have compared mortality among substance users or psychiatric patients have important limitations. Several studies were based on only one hospital, which limited their generalizability (
8,
9,
10 ). Other studies coded only one primary psychiatric or substance use diagnosis, thus mixing patients who have co-occurring psychiatric and substance use disorders together with substance abusers who had no other mental disorders (
1,
3 ).
Two recent studies have used large statewide data sets to compare mortality of psychiatric patients with and without co-occurring substance use disorders. Maynard and colleagues (
11 ) estimated that discharged psychiatric inpatients with a co-occurring substance use diagnosis had a 50% higher risk of mortality compared with patients with a psychiatric disorder only. Dickey and colleagues (
12 ) found that patients with co-occurring disorders had a 60% higher risk of mortality from external causes than did patients with a psychiatric disorder alone. However, this study included deaths from only external causes, so it did not assess medical sequelae of substance use.
The U.S. Department of Veterans Affairs (VA) is perhaps the world's largest provider of mental health care, annually treating 1.1 million patients diagnosed as having psychiatric or substance use disorders (Greenbaum, 2007, unpublished analysis of VA administrative data for fiscal year [FY] 2005). Over one-third of VA patients screen positive for psychiatric or substance use disorders (
13,
14 ). Yet few studies have examined substance-related mortality among VA psychiatric patients. Studies of mortality among VA psychiatric patients have generally been narrow in scope, focusing on a specific cause of mortality (such as suicide) (
15,
16 ), a particular psychiatric condition (schizophrenia or posttraumatic stress disorder [PTSD], for example), or a special subpopulation (such as homeless patients) (
17 ). No prior studies have specifically assessed substance-related mortality among VA psychiatric patients.
Half of all VA patients with psychiatric or substance use disorders served during the period of the Vietnam war (Greenbaum MA, 2007, unpublished analysis of VA administrative data for FY 2005). This "Vietnam era" cohort includes military personnel deployed to Southeast Asia and those who served elsewhere. This is a particularly relevant cohort for assessing substance-related mortality. This was the first generation of veterans to come of age at a time when street drugs were readily available in addition to alcohol. This cohort has also now reached middle age, when chronic medical effects of substance use might begin to affect their survival.
This study examined mortality and causes of death among Vietnam-era servicemen who received VA treatment for psychiatric disorders. This study addressed two specific questions. How much does having a diagnosed co-occurring substance use disorder contribute to overall mortality among VA psychiatric patients? And do causes of death differ between psychiatric patients with and without co-occurring disorders?
Methods
Sample
Data were selected for male patients who met four inclusion criteria. First, they completed an outpatient mental health or substance abuse treatment visit in any VA medical center or clinic between April 1, 1998, and September 30, 1998 (the first mental health or substance abuse clinic visit during that period is termed the "index visit"). We based inclusion on the outpatient file because preliminary analyses showed that a large majority of VA inpatients also had one or more VA outpatient visits. Second, they received an ICD-9 code consistent with a DSM-IV axis I psychiatric diagnosis for a problem other than substance use (see below) during the index visit or in the 12 months before that visit. Third, they served during the period of the Vietnam war (Vietnam-era veterans). This does not necessarily mean they were deployed to Southeast Asia. VA administrative data typically do not indicate whether someone was in combat. Fourth, patients were between the ages of 40 and 59 at the time of the index visit. These criteria yielded a total of 169,051 participants.
Data sources and measures
VA medical administrative data. VA treatment utilization, psychiatric and medical diagnoses (
ICD-9 codes), and demographic information were drawn from the VA outpatient encounter file, patient treatment file, and the extended care file. Analyses comparing diagnoses in VA administrative records with diagnoses in patients' charts indicated .88 sensitivity and .99 specificity for diagnosis of alcohol dependence, .67 sensitivity and .99 specificity for diagnosis of drug dependence among inpatients, and median sensitivity of .94 and median specificity of .98 for medical diagnoses in primary care (
18,
19 ).
Demographic variables obtained from these files included age, race, marital status, income, and receipt of a pension for a service-related medical or psychiatric disability. Because racial information is typically incomplete in VA administrative records, race was coded into three categories: white non-Hispanic, nonwhite or Hispanic, and missing data.
Psychiatric diagnoses qualifying patients for inclusion in this study were categorized into six dummy-coded variables: depressive disorder (depression or dysthymia), PTSD, other anxiety disorder (other than PTSD), bipolar disorder, dementia or mild cognitive impairment, and psychotic disorder (schizophrenia or other psychosis). Patients were required to have one or more of these diagnoses to be included in the study. Substance use diagnoses were coded into a four-category variable: no substance use disorder, alcohol use disorder (abuse or dependence), drug use disorder (abuse or dependence), and both an alcohol and a drug use disorder.
Medical diagnoses and severity of illness were coded with the Charlson Index (
20 ), an indicator of medical severity designed to predict mortality risk, which has been shown to have adequate reliability and predictive validity (
21 ). Charlson medical severity scores range from 0 to 16: two-thirds of patients (N=113,520) had a score of 0, indicating no co-occurring medical conditions; only 12.5% (N=21,119) had a score of 2 or higher. Inpatient utilization data for the 12 months before the index visit were coded with VA bed section codes. We included four variables indicating presence or absence of any hospitalization in an acute or intermediate medical bed section, a medical extended-care bed section, an acute or intermediate psychiatric bed section, and an acute or intermediate addiction treatment bed section. Stays in psychiatric residential or extended care and in residential addiction treatment were coded but not included in the analyses because they did not predict mortality.
Mortality and cause of death. Mortality status was assessed for the seven years from the index visit in 1998. Mortality was determined from the VA's Beneficiary Identification and Records Locator Subsystem (BIRLS), which lists all deceased veterans whose families received VA death benefits. BIRLS is free to VA researchers and is nearly as accurate as mortality information purchased from the National Death Index (NDI) (
22,
23 ). This makes it a cost-effective alternative for large-scale mortality studies of VA patients.
Because BIRLS does not include causes of death, we purchased cause-of-death information (
ICD-10 codes) from NDI for a random sample of the decedents identified in BIRLS. We sampled 11.4% of the decedents without substance use diagnoses (N=1,324) and 23.8% of decedents who had co-occurring substance use disorders (N=2,059). This sample size yielded 90% power to detect a small (Cohen's h=.20) difference in proportions of causes of death between our smallest cell of patients with co-occurring psychiatric and substance use disorders (340 decedents who had psychiatric illness plus drug abuse diagnoses) and the reference group of decedents with only psychiatric diagnoses.
ICD-10 codes for death were categorized into 11 mutually exclusive categories. Comparative data on mortality rates and causes of death among males in the general U.S. population were obtained from the National Center for Health Statistics (
24,
25 ) and were weighted to match the age and white-nonwhite distributions of our sample.
Statistical analyses
We considered two alternative methods of multivariate analysis. Logistic regression considers whether an individual died by a certain time point. Survival analysis uses more of the data because it also uses information on when each person died. However, survival analysis may be less intuitive to readers unfamiliar with mortality research. We decided to use logistic regression after preliminary analyses showed that the hazards did not cross and that both analytic methods generated similar risk estimates.
Logistic regression analyses evaluated the association between substance use diagnoses and mortality while controlling for covariates that had significant bivariate associations with mortality. Variables that had significant bivariate effects on mortality but no significant effect after other variables were controlled for were conceptualized as markers for other factors but not included in the final model (
26 ). In addition to the substance use disorder categorical variable, covariates entered in the final model were age, race, marital status, psychiatric diagnoses (psychotic disorder and PTSD), medical severity (Charlson Index), and hospitalizations (acute or intermediate medical, medical extended care, acute or intermediate psychiatric, and acute or intermediate addiction treatment). The correlates of all predictors in the regression model were less than .30 (median r=.04), indicating acceptably low multicolinearity. To control for experimentwise error, we adjusted the alpha criterion by Bonferroni analysis to p<.004 (p<.05/14).
To aid clinical interpretation of these findings, the odds ratios (ORs) generated in the regression model were also used to estimate risk-adjusted probabilities of dying within seven years for people with different substance use disorders. These probabilities were calculated with the following formula: estimated probability= (OR i ×odds 0 )/[1+(OR i ×odds 0 )], where OR i is the odds ratio for each substance use disorder category in the regression model and odds 0 is the odds of dying for patients in the reference category (patients without co-occurring substance use disorders).
Differences in causes of death
An omnibus chi square analysis was conducted to evaluate whether cause-specific mortality differed between patients with and without a substance use diagnosis. If this overall test proved significant at p<.01, follow-up chi square comparison tests were conducted for each specific cause of death, which involved comparing each substance use category with the group that had psychiatric illness without a co-occurring substance use disorder ( α =.01).
Results
Sample characteristics
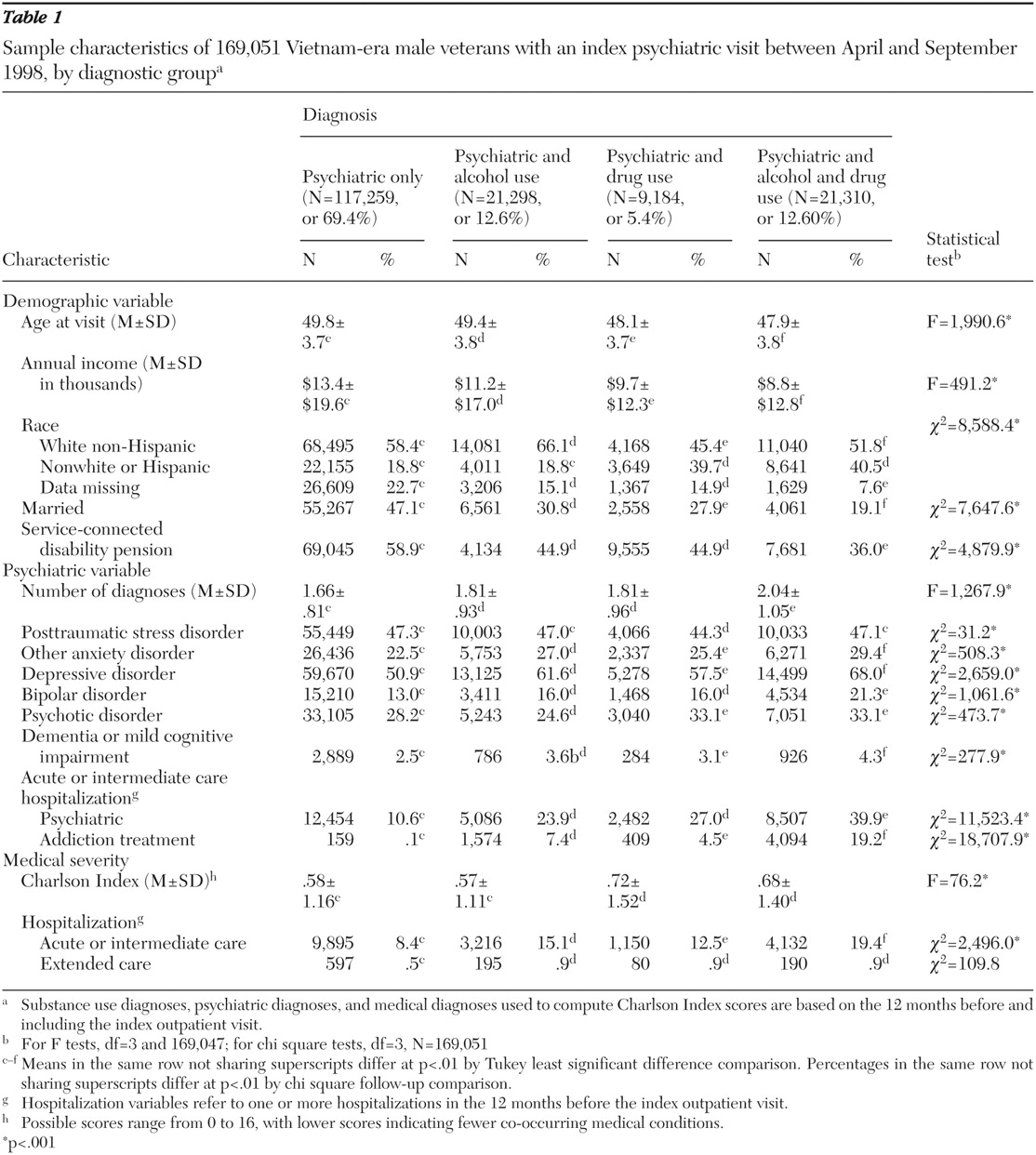
Table 1 presents demographic characteristics, medical severity, and psychiatric and substance use disorders of the sample. Overall, 57.8% (N=97,784) of the sample were white non-Hispanic, 16.5% (N=27,833) were African American, 5.4% (N=9,153) were Hispanic, .4% (N=668) were Asian or Pacific Islander, .5% (N=802) Native American, and 19.4% (N=32,811) were of unknown race (race information was missing from their administrative data).
Observed mortality
In our entire sample of psychiatric patients, 20,198 people (11.9%) died within seven years. This is double the seven-year mortality rate (5.8%) for age- and race-matched males in the general U.S. population.
Observed mortality rates are shown in the solid black bars in
Figure 1 . One in ten (9.9%,) psychiatric patients without a co-occurring substance use diagnosis died within seven years. The mortality rate was nearly 70% higher, 16.7% (N=8,631) among psychiatric patients diagnosed as having any type of co-occurring substance use disorder. By specific substance use diagnoses, seven-year mortality rates were 17.7% among psychiatric patients with alcohol use disorders, 16.4% among psychiatric patients with both alcohol and drug use disorders, and 15.1% among patients with co-occurring drug use disorders.
Covariate-adjusted mortality
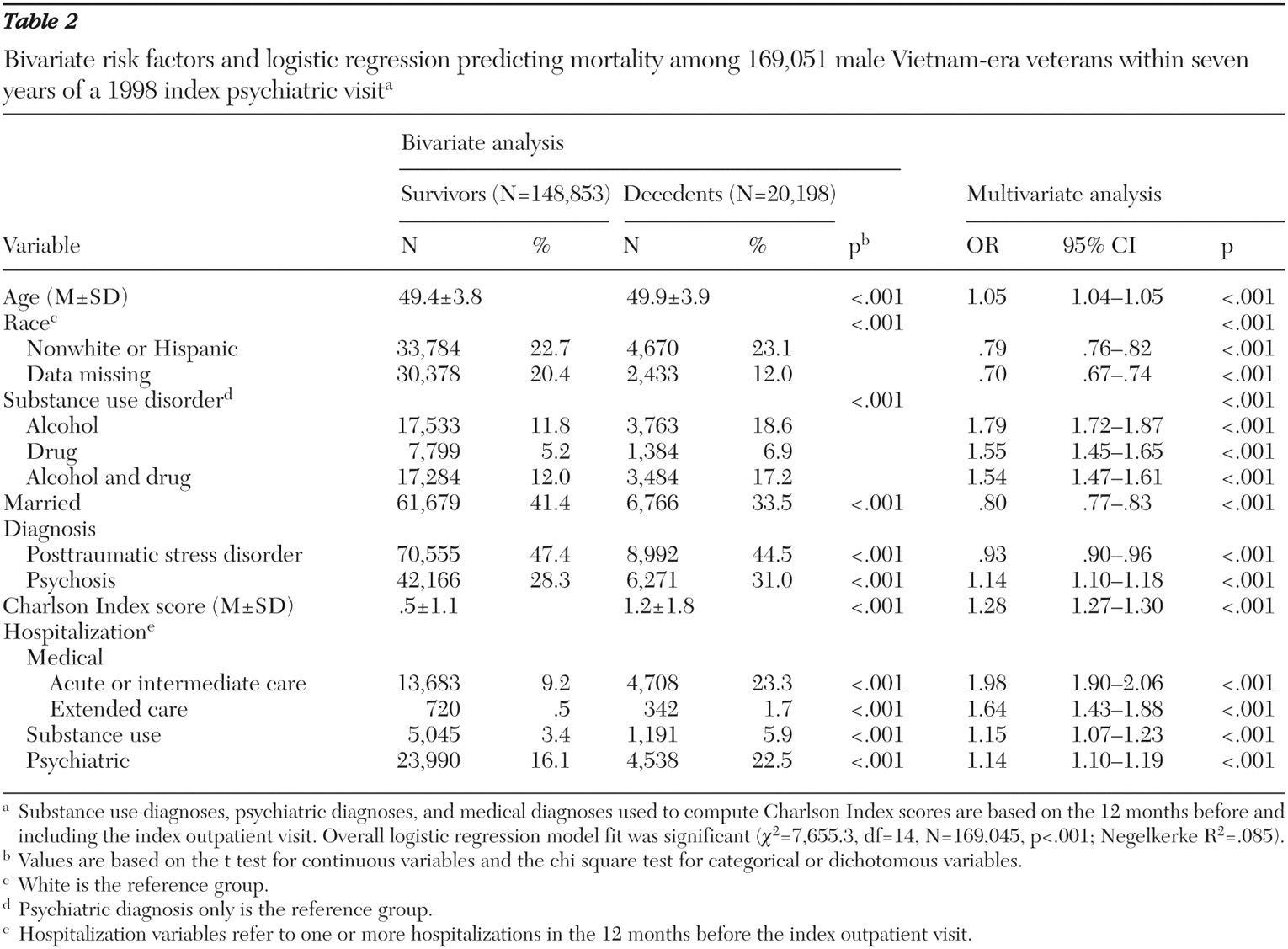
Table 2 presents both bivariate effects and multivariate effects of risk factors included in the logistic regression model. The overall logistic regression model was significant (
χ 2 =7,655.3, df=14, N=169,045, p<.001; Negelkerke R
2 =.085). Substance use diagnoses strongly predicted elevated mortality after the analysis controlled for covariates (
χ 2 =839.9, df=3, N=169,045, p<.001; incremental Negelkerke R
2 =.009). In comparison with mortality of psychiatric patients with no substance use diagnoses, mortality was significantly higher for those diagnosed as having co-occurring alcohol use disorders (OR=1.79), drug use disorders (OR=1.55), or both alcohol and drug use disorders (OR=1.54).
The pale bars in
Figure 1 show estimated risk-adjusted probabilities of death within seven years on the basis of the regression model. After we controlled for other covariates, patients with co-occurring substance use disorders had a 55% higher risk of dying than did psychiatric patients without substance use disorders (
Figure 1 ).
Risk-adjusted mortality appeared to be highest among patients with co-occurring alcohol use disorders. To test whether mortality varied significantly across persons with a substance use disorder, we conducted a post hoc analysis replicating our logistical regression but included only the patients with substance use disorders. The effect of substance use category (alcohol, drugs, or both) was significant ( χ 2 =17.9, df=2, N=51,787, p<.001) but small, explaining only .1% of the variance in outcome. Mortality among psychiatric patients with alcohol disorders was only slightly higher than for those with drug use disorders (OR=1.12, p<.002) or those with both alcohol and drug use disorders (OR=1.12, p<.001).
Causes of death
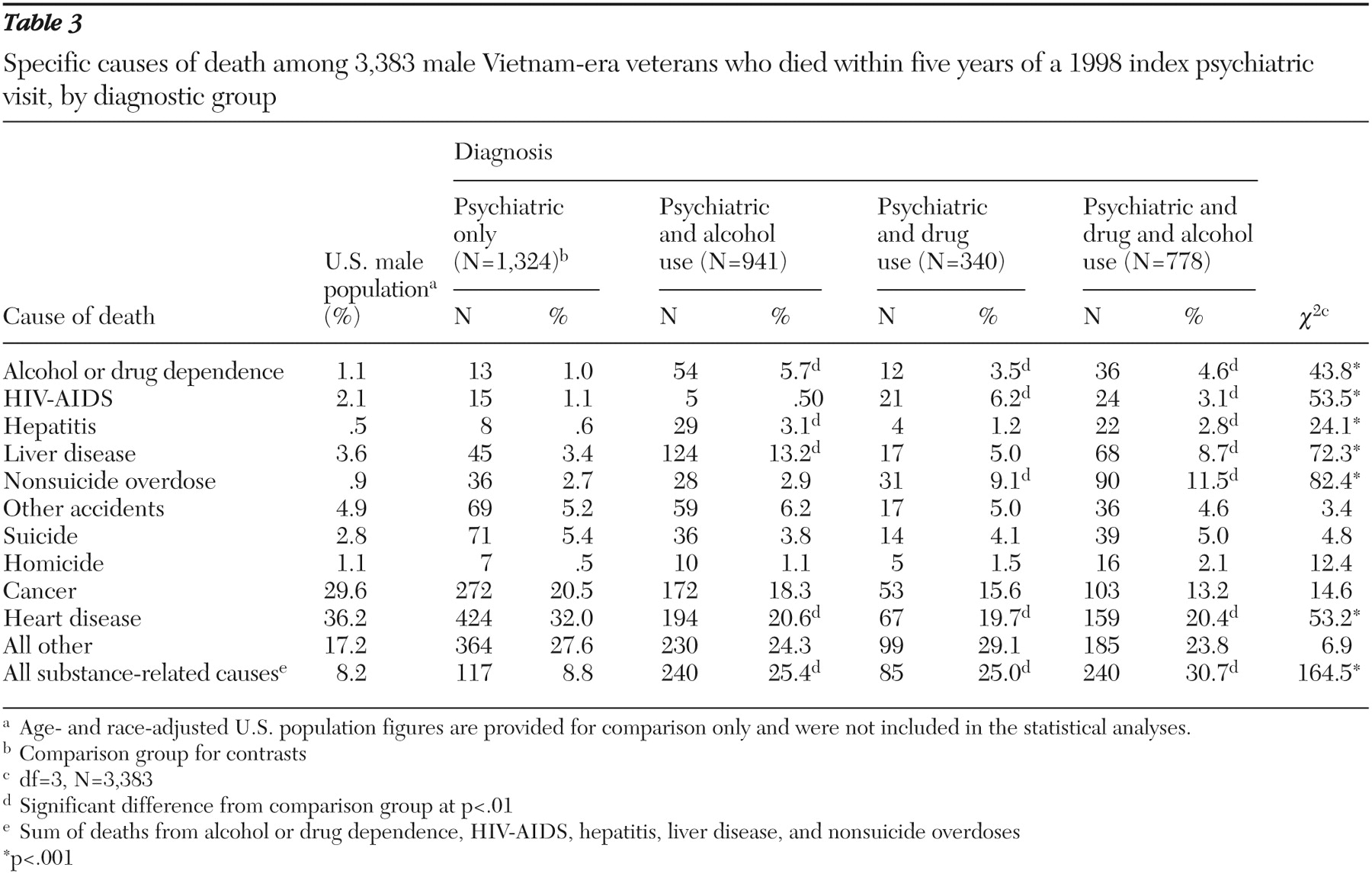
Among patients who died, causes of death differed significantly for those with and without substance use diagnoses (
χ 2 =356.9, df=30, N=3,384, p<.001). As shown in
Table 3, having any type of substance use diagnosis was significantly associated with a higher proportion of deaths attributed to "alcohol or drug dependence." Having an alcohol use disorder (with or without a drug use diagnosis) was associated with a higher proportion of deaths from liver disease and viral hepatitis. Having a co-occurring drug use diagnosis (with or without an alcohol use disorder) was associated with significantly higher proportions of deaths from overdose and HIV-AIDS.
Overall, at least one-quarter of the deaths in each of the groups with co-occurring substance use diagnoses were directly attributed to substance dependence, liver disease, hepatitis, HIV-AIDS, or nonsuicide overdoses. These combined causes of death accounted for only 8.8% of all deaths among psychiatric patients without a substance use diagnosis—similar to the distribution of these causes of death (8.2%) in the general U.S. population (
25 ).
Discussion
This study confirmed the contribution of substance use disorders to premature mortality among psychiatric patients. Consistent with previous research, this study found a two-fold increase in all-cause mortality among male psychiatric patients in comparison with their age- and race-matched counterparts in the general U.S. population. Among psychiatric patients, the probability of dying was 55% higher for patients diagnosed as having substance use disorders than among those without a substance use diagnosis. Psychiatric patients with co-occurring substance use disorders also had a significantly higher proportion of deaths from substance-related causes. Although similar findings have been reported in other samples (
11,
12 ), our findings are striking because we conservatively controlled for preexisting medical conditions, including potential sequelae of past substance use. The presence of a substance use disorder diagnosis emerged as the third strongest predictor of mortality status, surpassed only by the Charlson Index of medical comorbidities (
χ 2 =3,568.3, df=1, N=169,045, p<.001) and prior medical hospitalizations (
χ 2 =1,568.8, df=1, N=169,045, p<.001).
Our findings confirm the need for aggressive treatment of comorbid substance use problems among psychiatric patients. The proportion of deaths from substance-related causes among patients with co-occurring psychiatric and substance use disorders was three times higher than in the general population. This finding suggests that a co-occurring substance use disorder among psychiatric patients should be viewed as a potentially life-threatening condition requiring consistent risk assessment and intervention and should be treated with the same seriousness as other mortality risks, such as suicidality.
Better integration of addiction services with psychiatric care might reduce mortality from both acute and long-term effects of substance use. Sharing information about mortality risks with patients may be helpful as part of a motivational intervention (
27 ) to encourage psychiatric patients with substance use problems to seek, achieve, and maintain recovery. Because psychiatric patients often receive inadequate medical care (
2,
28 ), secondary prevention efforts to ensure adequate medical care could reduce mortality from HIV-AIDS, hepatitis, and liver disease among psychiatric patients with co-occurring substance use disorders. System-level efforts to enhance coordination of care between mental health, substance abuse, and medical providers would further ensure that the medical needs of these patients are fully addressed.
This study has several strengths, including the use of a national census of all psychiatric outpatients treated within a large health care system that maintains extensive electronic medical records. These records enabled control for preexisting medical comorbidity and prior hospitalizations when assessing mortality risk. Limiting the sample to men ages 40 to 59 removed the confounding of substance use with age and gender that is found in some other samples. Focusing on middle-aged patients also allowed detection of the long-term medical consequences of substance use.
Reliance on administrative data has some inherent limitations, including diagnostic uncertainty, incomplete data, and nonstandardized data collection. Information on smoking status, a key predictor of mortality, was not available. Finally, our sample was limited to male Vietnam-era veterans receiving VA services. It would be interesting to assess whether similar findings are obtained among female veterans who served during the same period. Future research should examine whether findings are similar in other samples of psychiatric patients, including nonveterans and those in other age cohorts.
Conclusions
In summary, this study confirmed that substance use strongly contributes to premature death among middle-aged male psychiatric patients, particularly among psychiatric patients diagnosed as having co-occurring substance use disorders. More research is needed to determine whether interventions to reduce substance use or to improve access to and compliance with medical care can reduce mortality among patients with co-occurring psychiatric and substance use disorders.
Acknowledgments and disclosures
This research was supported by Department of Veterans Affairs (VA) Seattle Epidemiological Research Pilot Project Grant CSP-603, awarded to the first author; the VA Sierra-Pacific Mental Illness Research, Education, and Clinical Center; the VA National Center for Posttraumatic Stress Disorder; the VA HSR&D Center for Health Care Evaluation; the VA Office of Academic Affiliations; and the VA Palo Alto Health Care System. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
The authors report no competing interests.