Depressive disorders involve considerable impairments of mental well-being, physical well-being, and social attachments (
1 ). There is evidence that guideline-adherent treatment leads to marked improvements in depressive symptoms (
2 ). Although both prevalence (one-year prevalence 6%) and symptoms of depression are roughly the same in all countries and cultures, differences can be discerned depending on a person's cultural background (
3,
4 ). Over 14 million people in Germany have a non-German cultural background (
5 ). Although these persons constitute a heterogeneous group, with diverse cultural, ethnic, religious and social origins, many share a barrier to health care in terms of their limited proficiency with the German language (
6 ).
Although communication is seen as particularly important in the treatment of depression (
7,
8 ), little is known about the impact of language barriers on the quality of inpatient depression treatment. This study analyzed process and outcome quality of inpatient treatment of depression in association with patients' level of proficiency in speaking German.
Methods
Between 1998 and 2000, all patients with depression were consecutively documented in 24 hospitals in Baden-Württemberg (South Germany). In addition to having a diagnosis of depressive illness according to
ICD-10 criteria (dysthymia, depressive episode, or adjustment disorders), a further inclusion criterion was sufficient linguistic competence to fill out assessment questionnaires. Diagnostic and therapeutic measurements during inpatient treatment, admission and discharge diagnosis according to
ICD-10 criteria, and the duration of stay were extracted from the computerized patient files (the documentation system for German psychiatric hospitals) (
9 ). The study protocol was approved by the local ethics review committee, and written informed consent was obtained from all participants.
For outcome quality, the Hamilton Rating Scale for Depression (HAM-D) was used to measure depression severity at both admission and discharge. Patients' language proficiency was assessed by the attending clinician. Assessment choices were native German speaker, nonnative speaker with good German language proficiency, and nonnative speaker with limited German language proficiency.
From the sample of 3,189 patients with depressive illness, three subgroups were formed according to their German speaking proficiency and subsequently matched with a sequential procedure. First, all patients from the smallest group (limited German proficiency) were analyzed in terms of the distribution of sex, age, and education characteristics in order to establish a frame of reference for further steps. Next, patients from the other two groups (native Germans and patients with good German proficiency) were included in a stepwise process; the analyses always included the patient with the smallest possible difference between the reference and empirical distribution of the variables. The group sizes were kept equal at 67 in order to provide optimal characteristics for statistical testing (balanced group sizes) and to avoid overpowering the comparisons and thus emphasizing statistical effects that were not clinically relevant.
Both process and outcome parameters were analyzed according to the following questions: Which measures did the hospitals use? How successful was the inpatient treatment? What was the duration of treatment? To analyze the primary outcome (improvement of depressive symptoms), the individual difference between HAM-D score at admission and discharge and the individual response rates were calculated. We defined complete remission as the absence of clinically relevant depressive symptoms (HAM-D score at discharge ≤7, with possible scores that range from 0 to 56), a partial remission as an improvement of at least 50%, and minimal remission or no response as less than 50% improvement compared with the admission score. On the basis of level of data (interval or categorical scales), we used t tests, univariate analyses of variance with Scheffé post hoc tests (interval or Likert scales), and chi square tests (categorical scales) to compare groups. A two-sided significance level of p≤.05 was used throughout, and analyses were conducted with SPSS, version 15.0.
Results
Of the 201 patients, about two-thirds (N=132) were women. The mean±SD age was 51±11, and three-quarters of the patients lived with their partner or children (N=153). German patients indicated being in full-time or part-time employment with greater frequency than the other two groups (35 native Germans, 53%; 26 speakers with good proficiency, 39%; 20 speakers with limited proficiency, 31%). Nonnative patients with limited proficiency were more likely to be homemakers (13 speakers with limited proficiency, 20%; eight native Germans, 12%; nine speakers with good proficiency, 13%). Unemployed patients were found primarily in the two groups of nonnative German speakers (11 speakers with good proficiency, 16%; ten speakers with limited proficiency, 15%; three native Germans, 5%).
A depressive episode ( ICD-10 criteria) was the most frequent diagnosis given at admission (136 patients, 68%). German patients more frequently had a recurrent depressive disorder (28 patients, 42%), whereas patients from both nonnative speaker groups were more likely to show a first-time depressive episode (25 nonnative speakers with good proficiency, or 37%, and 23 nonnative speakers with limited proficiency, or 34%). With an overall HAM-D score of 22.2±7.0 (German patients, 22.3±7.1; nonnative patients with good proficiency, 21.1±7.1; and nonnative patients with limited proficiency, 23.2±6.7), all patients had a severe depressive disorder upon admission. Comparison of the subgroups with the original, unmatched sample of patients with depression showed that the sample we analyzed was somewhat younger, had a smaller age range, and lived with others somewhat more frequently.
A majority of patients in all three subgroups had already received in- or outpatient treatment for their depression before this study (58 native German patients, or 88%; 58 nonnative speakers with good proficiency, or 87%; and 60 nonnative speakers with limited proficiency, or 90%). There were also no differences between the groups regarding the number of depressive episodes (average of 2.6 episodes), and most patients had already received antidepressants before their hospitalization (57 native German patients, 85%; 56 nonnative patients with good proficiency, 84%; and 59 nonnative patients with limited proficiency, 88%). A significant difference was found regarding previous psychotherapeutic treatment. Whereas 18 (27%) native German patients had already received psychotherapy, only eight (12%) of the nonnative speakers with good proficiency and three (5%) of the patients with limited proficiency had ( χ 2 =13.84, df=4, p=.001).
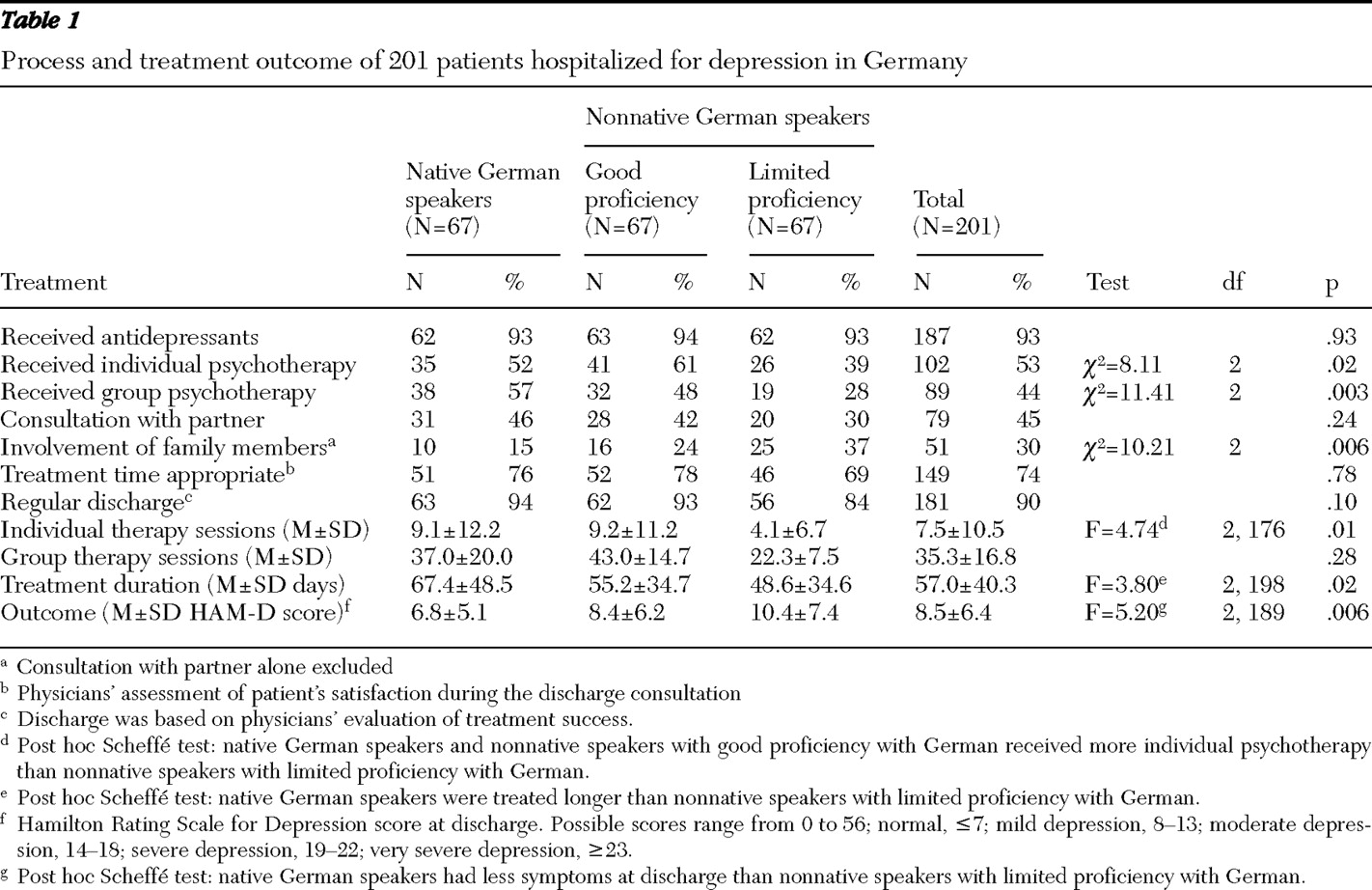
Differences in the type of psychotherapy emerged between the subgroups (
Table 1 ). Over half of the native German patients and 61% of the nonnative speakers with good proficiency received individual psychotherapy, but only 39% of the patients in the group of nonnative speakers with limited proficiency received this type of psychotherapy. Furthermore, the number of individual psychotherapy sessions for nonnative patients with limited proficiency averaged four sessions, significantly fewer than the number of sessions that native German patients and nonnative patients with good proficiency received (average of nine sessions each). Similarly, significantly fewer nonnative speakers with limited proficiency than patients in the other two groups took part in group therapy sessions. Although no differences were found regarding the involvement of patients' partners during inpatient treatment, there was a significantly higher involvement of family members in the nonnative speaker group with limited proficiency compared with the other two subgroups. Almost all patients received antidepressants, independently of subgroup, and approximately 59% (N=118) did not report any problems from using the antidepressants.
Significant differences between the subgroups were found in terms of treatment duration. Nonnative speakers with limited proficiency were discharged an average of 18 days earlier than native German patients and six days earlier than nonnative patients with good proficiency. Although no significant differences could be found with regard to patients' satisfaction with treatment length when assessed by physicians during the discharge consultation, almost one-fifth of nonnative speaker patients with limited proficiency were discharged against physicians' advice (11 patients, 16%).
By discharge, highly significant differences had emerged between the groups. Whereas native German patients no longer showed any depressive symptoms, nonnative patients with good proficiency showed residual symptoms. The least improvement was recorded among nonnative speakers with limited proficiency, who had slight depressive symptoms. Regarding the individual response rates, 53 (79%) native German patients had a complete remission, compared with 41 (61%) nonnative speaker patients with good proficiency. Nonnative patients with limited proficiency fared the worst, with only 35 patients (52%) showing a complete remission ( χ 2 =11.69, df=4, p=.02).
Discussion
On admission to inpatient treatment, the subgroups differed only with regard to previous psychotherapeutic treatment. The more limited the German speaking proficiency, the less frequently the patients indicated having had prior psychotherapeutic treatment. During inpatient treatment, native German patients more frequently received a combination of individual and group therapy. Patients from the two nonnative speaker subgroups, in contrast, received more individual therapy, whereas only a small number of these patients received group therapy. A reason for this could be that better communication was possible in an individual contact situation. Consultations with family members were also carried out more frequently in these two subgroups. Although it cannot be discerned from our data, it is very likely that this finding is attributable to family members' involvement as interpreters, which is a fairly problematic issue, considering that they are not qualified for this task (
7 ).
The central finding is the clear link between the length of hospitalization and the treatment outcome in association with the linguistic proficiency of the patients. Although an improvement in the depressive symptoms was achieved in all subgroups, as linguistic communication difficulties increased significantly fewer patients were discharged with complete remission of symptoms. In comparison with native German patients, twice as many nonnative speaker patients with good proficiency and almost four times as many nonnative speaker patients with limited proficiency were discharged with clinically relevant depressive symptoms. In this context, it is worth mentioning that a HAM-D score difference of even 3 points has clinical significance (
10 ).
Native German patients were treated for the longest period (average 67 days), and patients with limited proficiency were treated for the shortest time (average 49 days). This difference indicates the limitations of inpatient treatment in providing opportunities for intensive discussion for the nonnative speakers. In most clinics, limited resources and a lack of cross-cultural orientation offer no opportunity for intensive psychotherapy treatment of patients who speak different languages.
In summary, a clear link was apparent between linguistic proficiency and the course and outcome of treatment. With a comparable situation at the beginning of treatment, nonnative German speakers received less intensive treatment and were discharged earlier even if clinically relevant depressive symptoms were still present. This finding was all the more strongly pronounced the worse the communication abilities were between physician and patient.
Limitations can be found largely in the operationalization of German language proficiency. Using physicians' subjective assessments of language proficiency to determine group membership was problematic because of possible bias resulting from variability among physicians and cultural differences in communication styles. Furthermore, it was unclear whether nonnative speakers were immigrants or had indirect migration experience (such as being from a family's second generation of immigrants in Germany) or whether the German language was learned in Germany or abroad (such as ethnic German immigrants). Therefore, patients' cultural and migration experiences and their possible impact on treatment process and efficacy are unknown, and some of the group differences observed could be due to cultural differences rather than language differences (including differences in treatment preferences and physician-patient relationship).
Although the subjective assessment of communication abilities was ultimately the decisive factor in group assignment, it is nonetheless possible to draw important insights for the future care of patients with limited German language proficiency. To overcome the language problem the common practice of using family members as interpreters is problematic. If the use of qualified personnel with sufficient knowledge of foreign languages is not possible, the use of qualified interpreters is the optimal solution (
7,
11,
12 ). However, multilingual staff cannot be available for all languages, and the use of qualified interpreters is often not financially viable. Therefore, a good way to deal with this problem would be to enhance the cross-cultural competencies of hospital staff, including language skills for the main migrant groups as well as the assignment of qualified interpreters when necessary (
13,
14 ).
Conclusions
The results confirm the necessity of considering linguistic factors in the treatment of patients with depression. Further specific research is necessary regarding the impact of language proficiency as well as the impact of cultural and migration experiences of depressive patients with nonnative cultural backgrounds on the treatment process and its efficacy.
Acknowledgments and disclosures
Data are from the project "Quality Assurance of Inpatient Depression Treatment in the Psychiatric Hospitals of Baden-Württemberg," which was sponsored and supported by the Chamber of Physicians of the County of Baden-Württemberg. Dr. Berger initiated the project. The authors thank Ferdinand Keller, M.D., Rudolf Metzger, M.D., Werner Wiegand, M.D., Gerhard Schnell, M.D., Rolf-Dieter Stieglitz, Ph.D., and Manfred Wolfersdorf, M.D., for their active collaboration in carrying out the project and Matthias Felsenstein, M.D., for support with data collection.
The authors report no competing interests.