Use of antidepressants increased dramatically during the 1990s (
1,
2,
3,
4 ), with rates of antidepressant treatment for depression increasing from 37% in 1987 to 75% in 1997 (
2 ). This increase has largely been attributed to the introduction of selective serotonin reuptake inhibitors (SSRIs) in the late 1980s and 1990s—which, compared with tricyclic antidepressants, have fewer side effects, easier dosing, and less lethality in overdose—and to the concomitant advent of direct-to-consumer advertising for prescription drugs. It is believed that direct-to-consumer advertising both increased recognition of the symptoms of depression and diminished stigma associated with the disease, resulting in higher treatment rates (
2 ). During this time the modal location of treatment for depression moved from the mental health specialty sector to the primary care sector (
3,
5 ).
Although several studies have documented increased antidepressant use during the 1990s, there have been relatively few studies investigating rates of use in the 2000s, although this period has also been one of dynamic change. Recent studies examining trends in antidepressant treatment have focused on children and adolescents, following the warnings regarding suicidality and SSRI use in the United Kingdom in June 2003 and by the Food and Drug Administration (FDA) in October 2003 (
6,
7,
8,
9 ). These studies all found a significant decline in antidepressant use among children and adolescents after the FDA warnings, with one study documenting that 80% of pediatricians altered how they managed depression after the FDA warnings (
10 ). However, there is no evidence of greater frequency of provider contacts in this population, even though the FDA warning recommended increased supervision of youths taking antidepressants (
11 ). One study that examined the spillover effect of the FDA warnings on adult depression treatment by using claims data from managed care plans from 1998 through 2005 found a significant reduction in antidepressant use among adults (
12 ).
However, several other important events during the early 2000s may also have affected antidepressant use. For example, several widely prescribed SSRIs either went off patent during or shortly after this period. Also, new antidepressants were introduced. Although there are no studies to suggest that these newer medications are more efficacious, some of these medications have new mechanisms of action, easier dosing regimens, and different side effect profiles. It is possible that direct-to-consumer advertising of antidepressants influenced the rate of antidepressant use during this period, because drug companies promoted newer antidepressants more heavily and older off-patent SSRIs less actively. Also, during the past decade antidepressants have been increasingly promoted and prescribed for anxiety disorders. If changes in treatment rates for depression are to be understood, it is important to track antidepressant prescriptions for the entire population, as well as for those with depression.
This study used data from a nationally representative survey of U.S. households to estimate rates of antidepressant use, including rates of adequate antidepressant treatment, between 2000 and 2004. These rates were examined for the U.S. population as a whole and for individuals with self-reported depression and self-reported anxiety disorders without comorbid depression. Antidepressant treatment rates were examined by age group and by antidepressant medication class in order to identify whether any observed trends were being driven by a particular age group of patients or class of medication.
Methods
Data
This study used data from the 2000–2004 Medical Expenditure Panel Surveys (MEPS), a nationally representative survey sponsored by the Agency for Healthcare Research and Quality (AHRQ) that is conducted annually. The MEPS employs an overlapping panel design in which data are collected for individuals over a two-year period, and the data can be used for cross-sectional or longitudinal analysis (
13 ). The MEPS household component collects detailed information on health care use and expenditures, health status, health insurance coverage, and demographic characteristics. There were a total of 25,096 observations in 2000, 31,196 observations in 2001, 39,165 observations in 2002, 34,215 observations in 2003, and 34,403 observations in 2004. This resulted in a combined sample of 164,075 observations. The data in each year of the MEPS household component were collected during that year (for example, the MEPS 2004 Household Component data were collected in 2004). The MEPS content and sampling procedures are described in detail at
www.meps.ahrq.gov .
Individuals with depression or anxiety disorders
Individuals with depression were identified with the medical conditions file of the MEPS. The medical conditions file contains an observation for each self-reported medical condition the individual experiences during the year. Parents or guardians report medical conditions for youths younger than 18 years. Households in the MEPS sample are interviewed five times over a 2.5-year period. During each interview respondents are asked about medical conditions that were experienced since the previous interview. Thus all conditions are self-reported by respondents. Self-reported conditions are mapped onto ICD-9 codes by the AHRQ using the full five-digit ICD-9 codes. For example, if a person responds that he or she had depression, this is assigned a code of 311 (depression not otherwise specified), while a response of major depression was assigned a code of 296.2 or 296.3. Thus we classified conditions with ICD-9 codes of 296.2, 296.3, or 311 as depression. In this report the term depression is used to identify these individuals. By using this method, 10,959 individuals with depression (6.6% of the sample) were identified over the 2000 through 2004 samples.
Individuals with anxiety disorders were also identified from self-reported conditions. We classified as anxiety disorders conditions with ICD-9 codes of 300.0–300.9 and 308.0–309.9, which are broadly defined as neurotic disorders (for example, panic disorder, generalized anxiety disorder, and obsessive-compulsive disorder), acute reaction to stress, and adjustment reaction (for example, posttraumatic stress disorder). Individuals with comorbid depression were not included in the calculations for anxiety disorders. Individuals with comorbid depression and anxiety were excluded from the study. By using this method, 6,899 individuals with anxiety disorders (4.2% of the sample) were identified.
Antidepressant treatment
Antidepressant treatment was identified using the prescribed medicines event files of the 2000–2004 MEPS household components, which contain 1,421,240 prescribed medicine records combined. Each record represents one household-reported prescribed medicine purchased or obtained during 2000 through 2004. Antidepressant medications were identified by drug name. Drugs classified as antidepressants were amitriptyline, amoxapine, bupropion, citalopram, clomipramine, desipramine, doxepin, duloxetine, escitalopram, fluoxetine, fluvoxamine, imipramine, isocarboxazid, maprotiline, mirtazapine, nefazodone, nortriptyline, paroxetine, phenelzine, protriptyline, sertraline, tranylcypromine, trazodone, trimipramine, and venlafaxine. These antidepressants were also grouped into antidepressant medication class. The three classes identified included SSRIs (citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline), second-generation antidepressants (bupropion, duloxetine, mirtazapine, nefazodone, trazodone, and venlafaxine), and tricyclic or tetracyclic antidepressants (amitriptyline, amoxapine, clomipramine, desipramine, doxepin, imipramine, isocarboxazid, maprotiline, nortriptyline, phenelzine, protriptyline, tranylcypromine, and trimipramine). The tricyclic and tetracyclic antidepressants are referred to in this report as TCAs. It is possible for individuals to take more than a single class of antidepressant medication.
We calculated the daily dosage for each antidepressant prescription using the pill dosage and the number of pills in the prescription. In our analysis, it was assumed that each antidepressant prescription was for 30 days, unless fewer than 30 pills were prescribed. In this case, the number of days covered in the prescription equaled the number of pills supplied. Of the 75,201 prescriptions for antidepressants, 16,412 (21.8%) contained fewer than 30 pills. The daily dosages were then compared with the minimum adequate daily dosage, as defined by Weilburg and colleagues (
14 ).
Adequate depression care
Adequate antidepressant treatment over a one-year period was defined as receiving at least four antidepressant prescriptions at the minimum adequate daily dosage. This definition was based on evidence-based treatment guidelines (
15,
16 ) and is similar to that used by Kessler and colleagues (
17 ) in their analysis of depression care that used data from the National Comorbidity Survey Replication and in previous published studies (
18,
19 ). It is not possible to distinguish between treatment for acute depression and maintenance treatment of depression, so adequacy for acute treatment was used in this analysis.
Patient age
To determine whether trends in antidepressant use were being driven by a particular age group, four age categories were created, and antidepressant utilization rates were calculated for each age group separately. The four age groups correspond to children and adolescents (under age 18), young adults (18 to 34), middle-aged adults (35 to 64), and older adults (65 and older). Indicator variables for each age group were created and used in the analyses.
Statistical analysis
The analysis first calculated the proportion of all individuals who filled at least one antidepressant prescription during the calendar year and then calculated the proportion of individuals with self-reported depression and the proportion of individuals with self-reported anxiety who filled at least one antidepressant prescription during the calendar year. All estimates were calculated with the survey procedures of Stata statistical software using the weights provided by AHRQ to account for the complex sampling strategy when calculating standard errors and 95% confidence intervals (CIs) and to produce nationally representative estimates (
20 ). Next, the analysis was limited to only the respondents with self-reported depression. The proportion filling at least one antidepressant prescription, by age-group and by antidepressant medication class, was calculated for each calendar year. For all analyses of time trends, including those by age or by antidepressant medication class, statistically significant trends were identified with logistic regressions, with 2000 serving as the reference group and indicator variables for 2001, 2002, 2003, and 2004 included as the only covariates. Statistically significant overall time trends were identified by assessing the joint significance of the year variables in the logistic regression, and statistically significant differences between specific years (for example, comparing rates in 2002 to 2004) were identified by testing equality of the coefficients, both using the Wald test.
Results
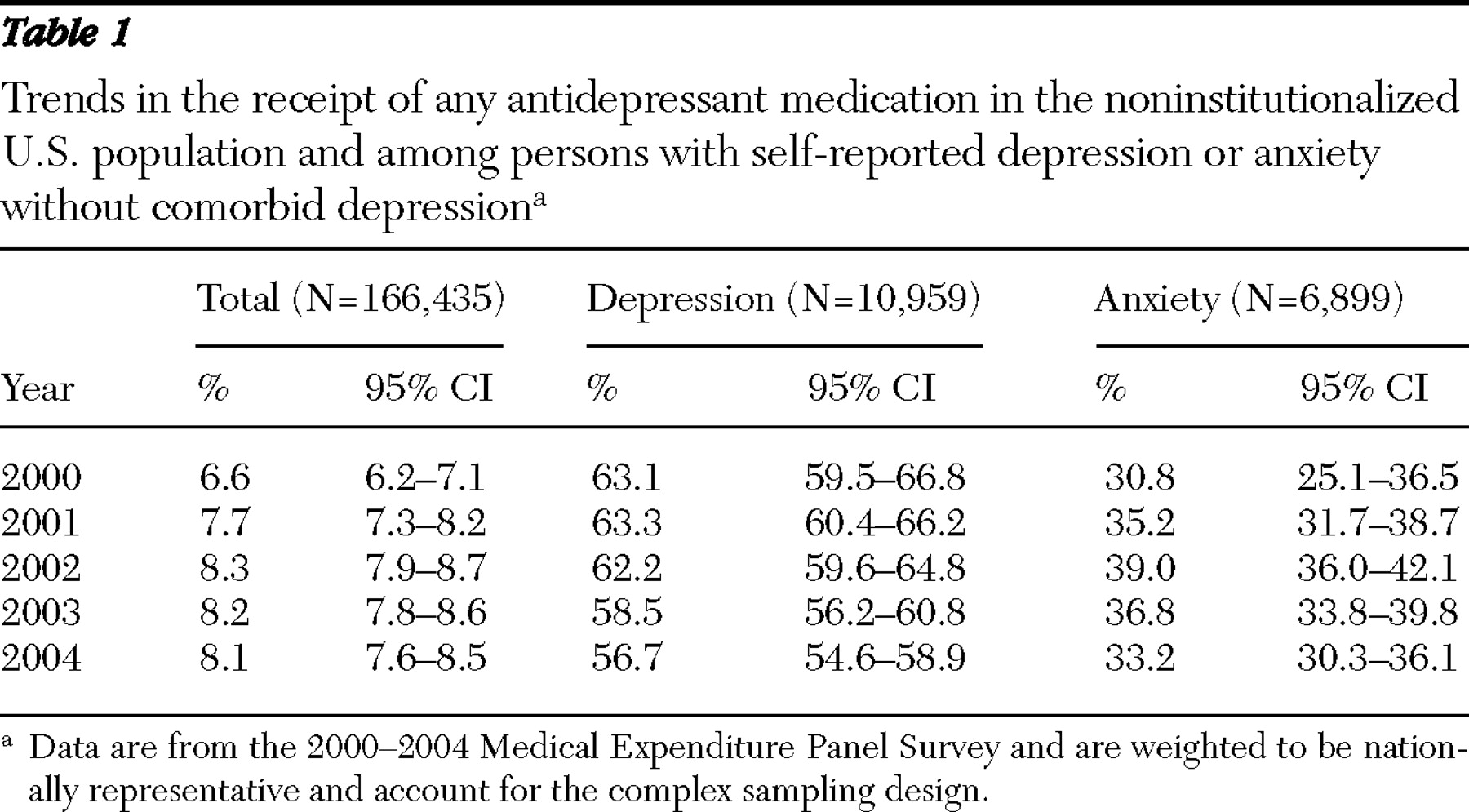
As shown in
Table 1, the percentage of all Americans who filled at least one antidepressant prescription during a calendar year increased from an estimated 6.6% in 2000 to 8.1% in 2004 (F=7.95, df=4 and 640, p<.001). However, the largest increase happened between 2000 and 2002, and rates remained essentially the same between 2002 and 2004. During the period examined by this study, the rate of self-reported depression increased steadily, from 5.9% in 2000 (CI=5.5%–6.3%) to 7.7% in 2004 (CI=7.3%–8.2%). Thus the percentage of the population with self-reported depression that used antidepressants rose between 2000 and 2004, from 3.7% (63.1% of those with depression used antidepressants × 5.9% had self-reported depression) to 4.4% (56.7% of those with depression used antidepressants × 7.7% had self-reported depression). For anxiety disorders, a mean of 4.6% reported having this condition without comorbid depression between 2000 and 2004 (CI=4.5%–4.8%), with the proportion also steadily increasing from 3.4% in 2000 (CI=3.1%–3.8%) to 5.3% in 2004 (CI=4.9%–5.7%).
When we examined data for persons with depression (
Table 1 ), a significant trend of decreasing rates of any antidepressant use was observed, decreasing from 63.1% in 2000 to 56.7% in 2004 (F=5.28, df=4 and 640, p<.001). This downward trend largely occurred between 2002 and 2004. A similar trend was observed among individuals with anxiety disorders. In 2000, 30.8% of individuals with anxiety disorders received at least one antidepressant, increasing to 39.0% in 2002 (t=2.45, df=640, p=.015) before dropping to 33.2% in 2004 (F=7.79, df=1 and 643, p=.005).
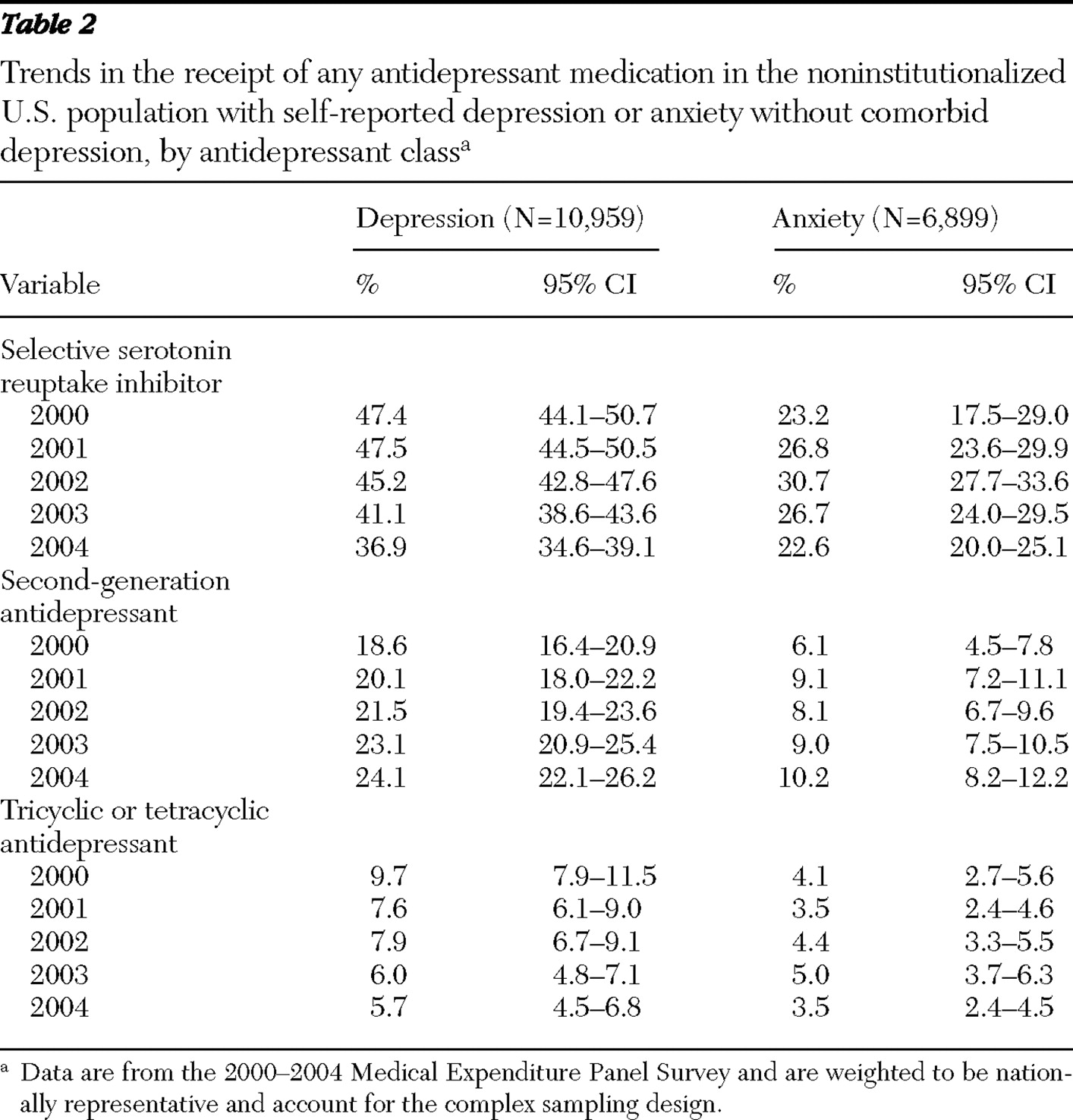
To identify the potential causes of this observed downward trend in antidepressant use among individuals with depression, rates of antidepressant use were examined by antidepressant medication class (
Table 2 ), by patient age (
Table 3 ), and by antidepressant medication class and patient age (
Table 3 ). When rates were examined by medication class, we saw that the downward trend in antidepressant use occurred mostly with SSRIs, where rates of any use dropped from 47.4% to 36.9% (F=12.29, df=4 and 640, p<.001), a 22% decline. Rates of TCA use also dropped during this period, from a high of 9.7% in 2000 to 5.7% in 2004 (F=4.56, df=4 and 640, p=.001). However, a significant increase in the use of second-generation antidepressants was seen over this period, increasing from 18.6% in 2000 to 24.1% in 2004 (F=3.69, df=4 and 640, p=.006). The trends in antidepressant use by medication class for individuals with anxiety disorders mirrored the trends among individuals with depression, with an upward then downward trend in SSRI use and an upward trend in use of second-generation antidepressants, although the rates of antidepressant use were significantly lower among individuals with anxiety disorders without comorbid depression.
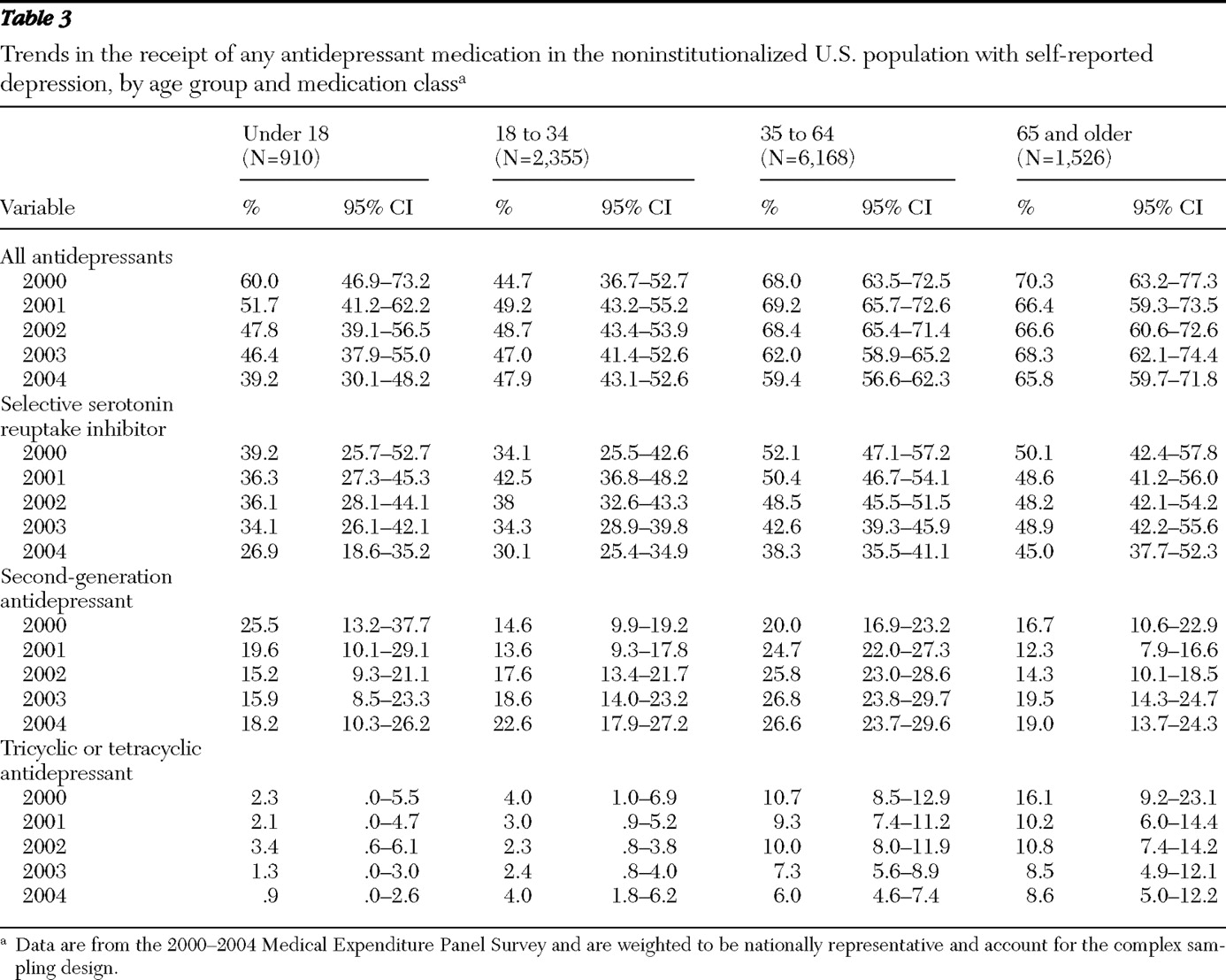
When rates of antidepressant use by age were examined, the decrease in use among individuals with self-reported depression occurred largely among children and middle-aged adults, where rates of antidepressant use dropped from 60.0% in 2000 to 39.2% in 2004 for children and adolescents and from 68.0% in 2000 to 59.4% in 2004 for middle-aged adults. However, because of the relatively small sample of children whose parents reported that they had depression and the resultant decrease in precision of estimates, the decrease in antidepressant use among children was not statistically significant at the p<.05 level. Rates of antidepressant use remained relatively constant for young adults and for older adults. When these trends were further broken down by medication class (
Table 3 ), the largest and most significant decline occurred for SSRIs among middle-aged adults, where rates of any SSRI use dropped from 52.1% in 2000 to 38.3% in 2004.
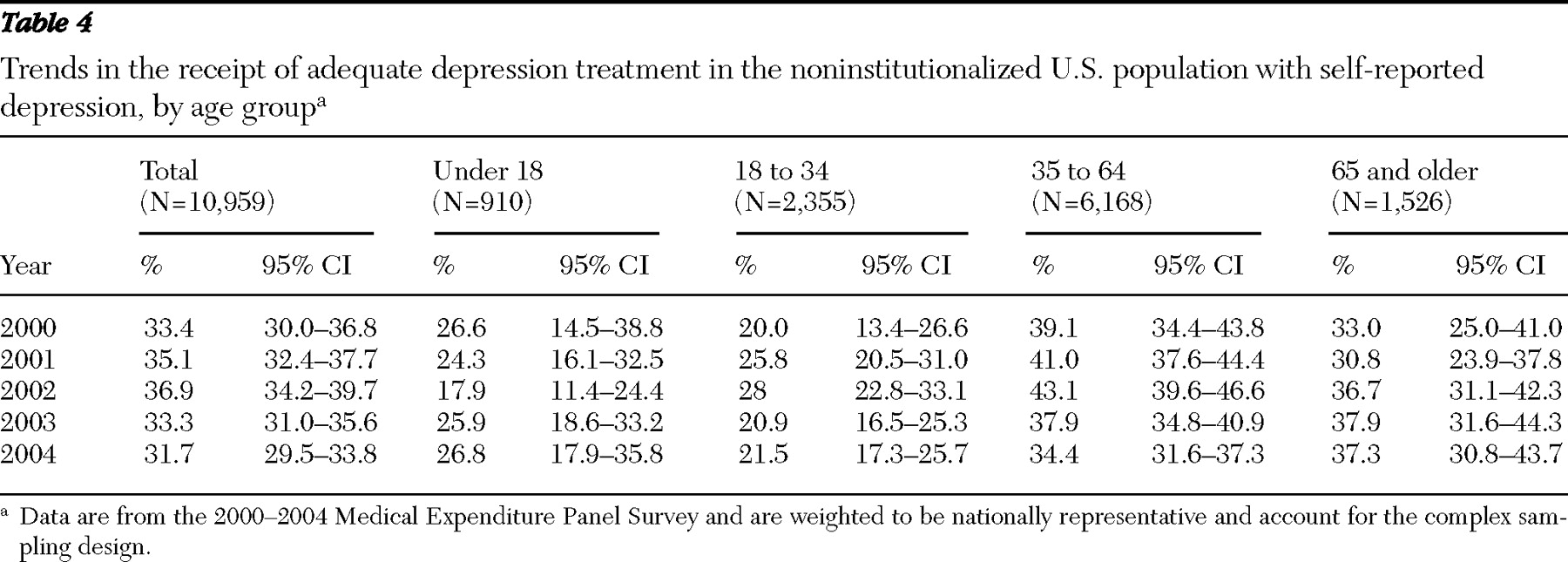
Finally, rates of adequate antidepressant treatment were calculated to determine whether the overall decline in antidepressant use was also seen for rates of adequate treatment (
Table 4 ). Adequate antidepressant treatment reached 36.9% in 2002, but that rate declined to 31.7% by 2004, a statistically significant drop (F=8.72, df=1 and 643, p=.003). Next, rates of adequate treatment were split by age to determine whether the observed trend was being driven by a particular age group (
Table 4 ). As was the case with the trend in any antidepressant use, a statistically significant decline in the rate of adequate treatment was seen only among middle-aged adults (from 43.1% in 2002 to 34.4% in 2004).
Discussion
We observed two major trends. First, after years of increased use of antidepressant therapy to treat depression, a trend reversal beginning in 2002 was observed. Second, the percentage of individuals with self-reported depression increased. As a net result, the percentage of the U.S. population with self-reported depression that was using antidepressants actually increased from 3.7% of the total population in 2000 to 4.4% of the total population in 2004.
The prevalence of antidepressant use by children whose parents reported that they had depression went from 60% in 2000 to 39% in 2004, a 35% drop. Rates of antidepressant treatment among middle-aged adults with self-reported depression also significantly declined between 2000 and 2004. However, it appears that some of the decline in SSRI use among middle-aged adults was offset by an increase in the use of second-generation antidepressants.
Although we cannot state definitively why the use of SSRIs declined during this period while the use of second-generation antidepressants increased, we can speculate. Perhaps most important, the SSRIs went off patent, or were going off patent shortly after this period, and thus the drug companies had no incentive to promote them. A likely result of this practice by drug companies is that use of cheaper generic versions of once popular drugs such as Prozac are being replaced with more expensive brand-name antidepressants that are heavily marketed. On the other hand, the decreased use of SSRIs might represent patients switching from a class of medications that was not effective to a class of medications with new mechanisms, which would be indicative of better treatment for depression.
Why did the use of antidepressants decline in the population with self-reported depression, but not in the overall population? Part of the decline may be explained by the increase in prevalence of self-reported depression over the observed time period. Although the proportion of people with self-reported depression who filled at least one antidepressant prescription decreased, the proportion of the total population that reported being depressed and that filled at least one antidepressant prescription increased. Another possibility is that the use of antidepressants for anxiety disorders increased over this period because antidepressants were actively promoted as being able to treat anxiety by drug companies to clinicians and patients. However, significant reductions in SSRI use were also seen among individuals who reported having an anxiety disorder, even though the warnings in the United Kingdom and by the FDA were not for individuals with these conditions.
There are some limitations to this study that should be considered when interpreting the results. One limitation is that we observed a downward trend in antidepressant treatment among individuals with self-reported depression, but we did not examine rates of effective psychotherapy. It is possible that rates of treatment were stable if individuals were switching from drugs to therapy, although this explanation is unlikely. Another limitation is the reliance on self-report to identify individuals with depression. It is possible that people with depression did not report being depressed or that people who did self-report having depression did not meet the clinical criteria for depression. Additionally, the date that antidepressant medication prescriptions were filled and the days of medication supplied were not known. Because only treatments that were provided during the calendar year were assessed, our data might be subject to left or right censoring—that is, some individuals may have initiated a treatment regimen before the beginning of the calendar year or continued treatment after the end of the calendar year, and thus, all of their prescriptions might not be included in our data, which would affect our estimates of rates of adequate antidepressant treatment. The issue of left censoring is common to past studies that have examined care in the past 12 months (
18,
21,
22 ). This study also only examined a five-year period, thus it is not known whether the observed trends have continued, and it is not possible to directly determine the causes of the observed trends.
Conclusions
Although there has been some concern about the overuse of antidepressants among individuals with less severe forms of depression (
23 ), this trend toward lower antidepressant use among people who consider themselves depressed is troubling, especially since a significant decline in the rate of adequate antidepressant treatment was also observed. Interestingly, this observed decline in antidepressant treatment began before the black-box warnings were included on antidepressant prescriptions in 2004, although the announcement regarding the link between SSRIs and suicidal ideation in adolescents was made in the United Kingdom in June 2003 and endorsed by the FDA in October 2003. Thus it appears that the decrease in antidepressant use after the FDA warnings that has been documented in several other studies (
6,
7,
8,
9,
12 ) was a continuation or perhaps an exacerbation of the trends documented in the study presented here. Further research is needed to help identify potential causes for the observed decline in antidepressant medication use among individuals who identify themselves as being depressed.
Acknowledgments and disclosures
This research was partially supported by grant U1CRH03713-04-00 from the U.S. Health Resources and Services Administration, Office of Rural Health Policy. The authors thank Fran Dong, M.S., and Stan Xu, Ph.D., for their assistance on this study.
The authors report no competing interests.