Understanding how clinicians decide about the use of psychotherapy techniques is key to designing effective appeals for their dissemination and sustained use. There is limited information on what influences clinicians to persist in practicing particular therapies, whatever their evidence base, or to adopt new therapies (
1 ). Thus far, evidence from surveys assessing psychotherapists' perceived influences on practice suggests the importance of several factors: supervision, discussions with colleagues, one's own personal therapy and work with clients (
2,
3,
4,
5,
6,
7,
8,
9 ); information gathered from books, academic learning, or professional training (
4,
6,
8 ); compatibility with therapists' repertoire of practices (
3,
10,
11 ); Internet or database searches (
5,
7 ); and time and resources for mastering treatments (
9 ).
Many surveys have focused on a restricted target population: most surveyed only psychology graduate students or psychologists (
2,
5,
9,
10 ). Others were limited either to specific guild associations, scientist-practitioners, or particular geographic regions (
2,
5,
10,
12 ). The mental health workforce, however, comprises numerous other core disciplines, such as psychiatry, social work, marital and family therapy, and psychiatric nursing (
13 ), with additional subcategories such as addiction counselors and licensed professional counselors. Psychologists and those trained in a scientist-practitioner model represent a minority of this workforce.
It is likely that influences on psychotherapy practices may differ according to work setting (such as private practice or other settings) and time since graduate training (recent graduates versus others). A better understanding of what affects the adoption and sustained use of new treatments could be used to directly influence what and how clinicians practice.
Although this study focused on the use of "new therapies," the findings should be relevant for evidence-based treatments as well. The development, rigorous scientific evaluation, and dissemination of evidence-based treatments have become a priority in the field of psychotherapy (
14 ). However, the enthusiasm for establishing evidence-based treatments has not been matched by an emphasis on developing evidence-based strategies for their dissemination and implementation (
15 ). Enhancing the use of evidence-based treatments depends on reaching and winning over a broad mental health clinician audience.
The primary purpose of this study was to identify influences on current clinical practices as well as on adoption and sustained use of new practices among mental health providers. A secondary aim was to determine whether there are demographic, training, and work-related differences in these influences.
Methods
Participants
Participants were readers of the Psychotherapy Networker ( PN ), a well-known psychotherapy magazine that received the prestigious National Magazine Award for excellence in the magazine industry. In 2006 PN was named by the Chicago Tribune as one of the 50 Best Magazines in America. The articles in PN typically focus on everyday challenges of clinical practice but also discuss social issues and therapeutic innovations.
A total of 2,739 users registered and at least partially completed the Web-based survey. Psychotherapists who lived outside of the United States and Canada (N=92, 3%) were removed from analysis because of potential differences in formal training, licensure, and practice circumstances. Furthermore, because the primary focus was on practicing clinicians, an additional 40 who were students were excluded, which left a total sample of 2,607.
Calculating a single response rate for Web-based surveys is not feasible, and thus we followed Eysenbach's advice (
16 ) to report response metrics, such as number of views and rates of participation and completion. To meet institutional review board requirements to ensure participant confidentiality, we did not use tracking cookies or perform Internet protocols checking. However, this kind of information would have allowed for the identification of the number of unique visitors to the Web site that is necessary to determine the view rate. One estimation for the participation rate is the number of registrations on the site divided by the number of individuals who were sent e-mails. On the unlikely assumption that every
PN subscriber who was sent an e-mail invitation visited the Web site and could be counted as a unique site visitor, a minimum of 13% consented to participate in this study. However, this is likely a gross underestimation of the true participation rate because the number of those who actually read the e-mailed invitation was likely to be substantially lower. The completion rate, a ratio of participants who completed the survey (N=2,085) to those who consented (N=2,901), was 72%.
Measure
The construction of our psychotherapy practices survey was a systematic, sequential, and iterative process that began with open-ended qualitative interviews about current practices and influences on practice that was conducted with seven psychotherapists (including psychiatrists, psychologists, and nurses). Interviews were interactive and adaptive; they were audiotaped and transcribed by a professional transcriptionist. The transcripts were reviewed by the first author and used to generate initial items for the survey.
Other potential items were culled from a range of Web sites (including the American Psychological Association's site at
www.apa.org ) and magazines (such as
PN ), and a provisional survey was devised (Cook JM, Coyne JC, McLellan AT, unpublished manuscript, 2004). Several national clinical researchers (including the second and third authors of the survey) reviewed the document, and six full-time clinicians filled it out and provided feedback on clarity, redundancies, and response burden.
We chose to assess the use of new rather than evidence-based treatments because it became clear during the pilot study that the definitions of "empirically supported" and "evidence based" were not uniformly understood and that most therapists were unfamiliar with which psychotherapies were evidence based.
The final version of the survey asks respondents to rate how much their current psychotherapy practice is influenced by each of 22 factors. These include traditional dissemination methods, such as workshops and journal articles, and innovations, such as the Internet and electronic Listservs. Respondents were also asked the degree to which eight factors would affect their willingness to learn and try a new therapy and the extent to which 11 factors were likely to lead to continued use. Responses were rated on a 5-point Likert scale: 1, not at all; 2, a slight extent; 3, a moderate extent; 4, a great extent; and 5, a very great extent. In the study, responses of 4 and 5 were coded "influential."
Procedure
This study was approved by the Columbia University-New York State Psychiatric Institute Institutional Review Board. Participation was elicited by two e-mail invitations from the editor of PN, sent two months apart between September 2006 and April 2007. Participants were directed to a secure Web site in which they were able to read a study description, offer consent, and complete the survey. To reduce rates of noncompletion and partial completion, e-mails were sent to those who registered and did not complete the survey as well as those who started the survey but did not complete it; the messages asked for feedback and ways to assist in completion. Although the survey was designed for Web-based administration, it was sent out by U.S. postal mail to 32 participants on their request.
Data analyses
The number and percentage of respondents who rated each item as influential were calculated, and the three highest and lowest influences were identified. For exploratory purposes, potential effects of three therapist characteristics on rating of influences were examined via independent-samples t tests: gender, work setting (private practice versus institutional settings), and time since graduate training. To facilitate understanding the magnitude of effects, we calculated effect sizes with Cohen's d (
17 ). For data analysis we used SPSS, version 16.
Results
Participants
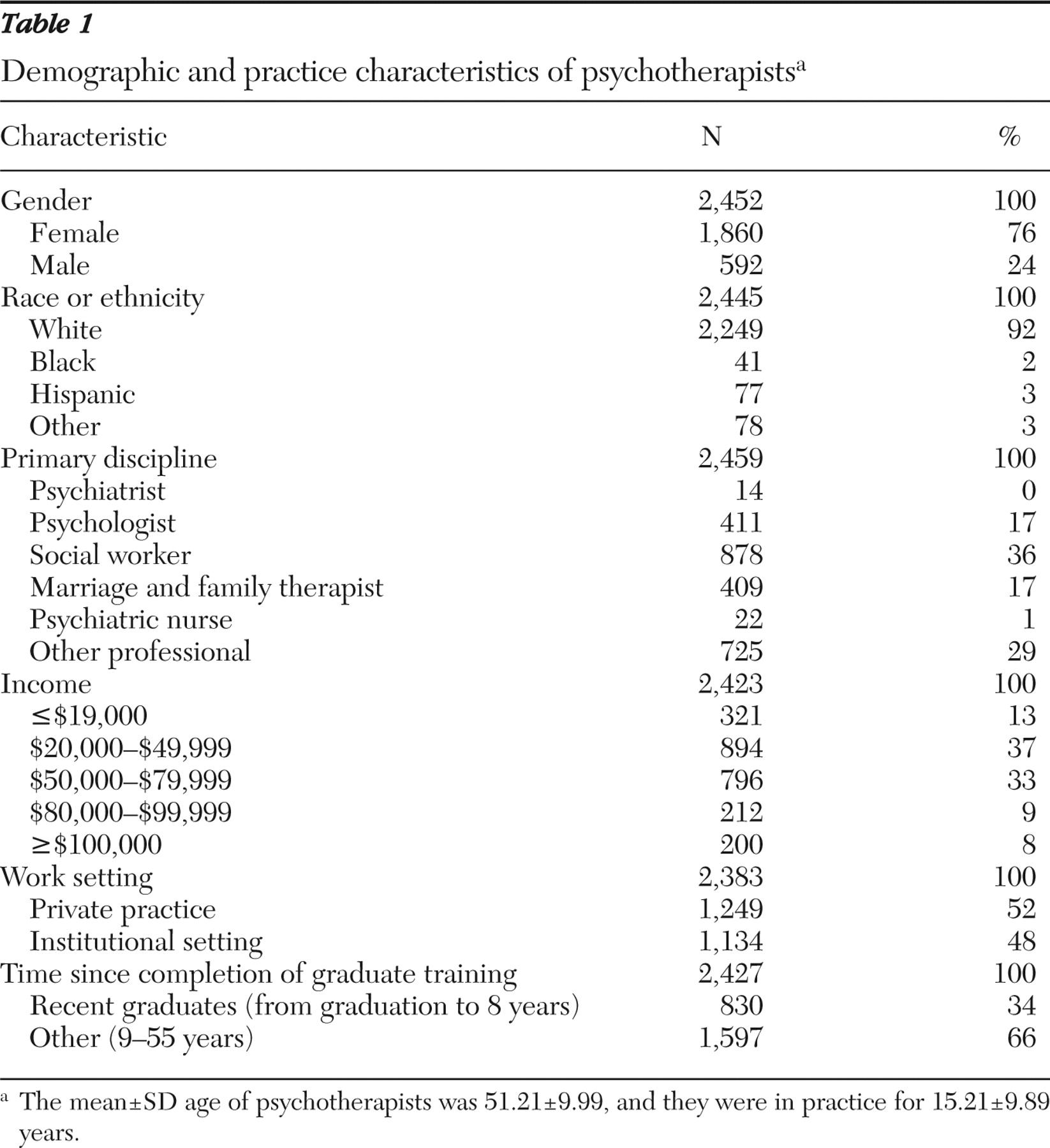
Participants' demographic characteristics are provided in
Table 1 . The typical participant was a white female holding a master's degree and in practice for 15 years, whose income from the practice ranged from $20,000 to under $80,000. Time since completion of graduate training ranged from 0 to 55 years (mean±SD of 14.61± 10.16 years). The sample was split into tertiles according to the number of postgraduation years. The bottom tertile (4.29±2.64, range zero to eight years) was compared with the combined upper tertiles (20.01±8.29, range nine to 55 years).
Influences
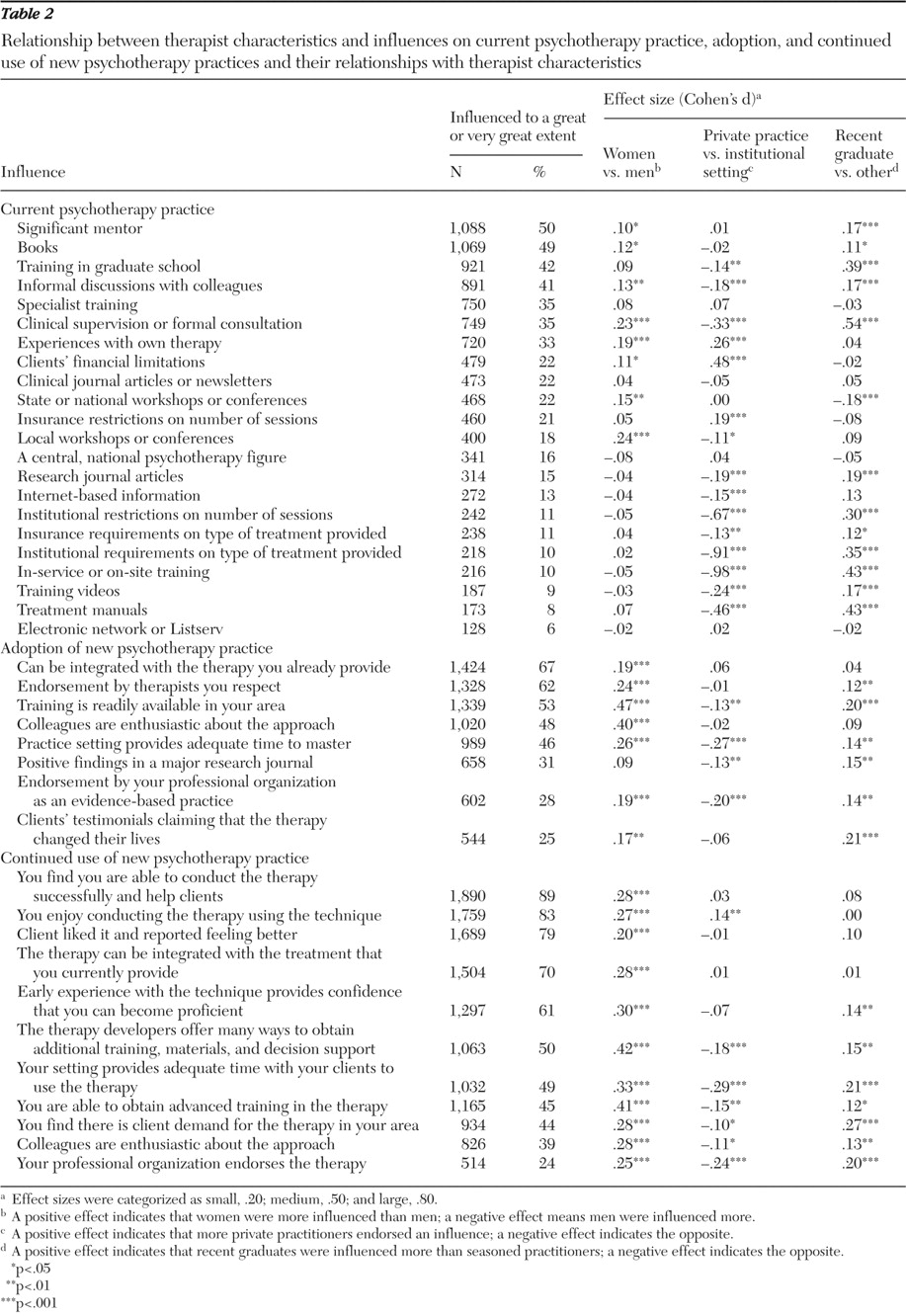
As shown in
Table 2, significant mentors, books, and training in graduate school were the top three influences on current practice. Training videos, treatment manuals, and electronic Listservs were the three least endorsed influences.
The top influences on willingness to learn a new therapy were that it can be integrated with therapy the clinician already provides, is endorsed by respected therapists, and is supported by local training opportunities (
Table 2 ). The three least influential factors were positive findings reported in a research journal, endorsement by a professional organization as being evidence based, and clients' testimonial about the therapy's effectiveness.
We found that the top three influences on a psychotherapist's willingness to continue to use a new treatment were ability to conduct the therapy successfully and help clients, the therapist's enjoyment in conducting the therapy, and clients' liking the therapy (
Table 2 ). Endorsement by one's professional organization, colleagues' enthusiasm about the approach, and client's demand were the three factors that were least influential.
Relationship between therapist characteristics and influences
Overall, most effects of the factors could be considered small (Cohen's d=.20). Only a few items achieved medium and large effects (Cohen's d=.50 and .80, respectively) and only for factors that influenced current practices. The largest effects for work setting were found primarily for institutional influences—that is, on-site training and institutional restrictions on the number of sessions and the type of treatment, with private practitioners feeling less influenced than those working in institutional settings. Supervision or formal consultation was the only influence with medium effect size for recency of training, and more recent graduates rated it higher.
Women rated influences higher than men. Private practitioners rated influences lower than clinicians working in institutional settings, with two exceptions—experiences with own therapy and clients' financial limitations—which were rated higher by those in private practices. Recent graduates were more influenced than earlier graduates.
Discussion
This study provides information on a broad range of North American psychotherapists in regard to what influences their current clinical practice, as well as their openness to adopt and use new treatments on a sustained basis. Findings have implications for the dissemination of evidence-based treatments, particularly the design of strategies to encourage the uptake of novel treatments.
Empirical evidence by itself did not have a strong direct influence on clinicians' decisions to use a treatment. Rather, significant mentors or role models, training received in graduate school, and informal discussions with colleagues were among the greatest determinants of current practice. Learning from books was rated as highly influential, whereas evidence-based media, such as treatment manuals, guidelines, and research-based and other types of journal articles, were rated low. It thus appears that evidence-based therapeutic strategies are more likely to be adopted if trainees are exposed to them early in their careers. For example, those interested in promoting evidence-based treatments may want to teach therapy courses, run workshops for graduate students, or serve as supervisors to students of psychotherapy while they are on field placements or completing practicums, internships, or postdoctoral fellowships. In contrast, the way to influence seasoned professionals might be to train a few respected clinicians in the treatment targeted for dissemination in places of employment.
Results further indicate that likelihood of integration of novel therapies with what therapists already provide and endorsement by respected therapists were top influences in encouraging clinicians to learn new approaches. The former is consistent with the seminal work on diffusion of innovations pioneered by Everett Rogers (
18 ). In particular, this influence parallels one of the Rogers' five characteristics of innovation necessary for successful dissemination—compatibility or the degree to which an innovation is consistent with potential adopters' existing values, experiences, and needs.
Factors such as personal effectiveness in conducting a therapy and helping clients (also substantiated by clients' feedback), enjoyment in conducting the therapy, and confidence in becoming proficient seemed to strongly affect the continued use of a newly acquired approach. These findings touch upon an important notion proposed by Bandura (
19 ), a sense of self-efficacy, or the belief that one is capable of successfully performing a particular task, such as a newly learned psychotherapy treatment.
Effects of therapist characteristics on influences
Gender differences, although small in magnitude, were found for nearly all influences on adoption and continued use of a new treatment. The only two factors influencing current practices that differentiated women from men were local workshops and conferences and clinical supervision or formal consultation. Perhaps because of greater family demands, female practitioners rely more on local resources. Although the effect was small, this finding may have important implications because most mental health providers are women (
13 ).
Effects of work setting were also small, with the exception of on-site training and institutional restrictions on the number of sessions and type of treatment. Private practitioners were understandably less influenced by these and other institutional factors but were affected more by their own therapy and clients' financial limitations.
Compared with seasoned professionals, recent graduates gave higher ratings to many of the influences, but most effects were small. Supervision or formal consultation was the only influence achieving even a medium effect size, with the importance of this factor understandably decreasing as time since graduation increased and practitioners become more assured in their skills.
Limitations
The main limitation of this study was the unknown rate of viewing the survey on the Web site and the participation rate of those who viewed it. Because demographic data for the
PN readership were not available, the characteristics of this sample could not be compared with those of subscribers. Although there is no comprehensive database on the mental health workforce to which our sample can be compared, our sample appears fairly comparable with estimates of the workforce in terms of professional discipline (
13 ). The proportions of certain disciplines in our study (that is, social workers, psychologists, marriage and family therapists, and professional and pastoral counselors) were nearly identical to those in Robiner's estimated mental health workforce data (
13 ). However, the number of psychiatrists was 16 times lower in our study, and the number of nurses five times lower. Although the exact representativeness of our survey is not known, our data set, much like the large and diverse study by Orlinsky and colleagues (
8 ), likely better captured the psychotherapy field than studies targeting specific professional populations.
Conclusions
Even though they were open to novel approaches, practitioners tended to stay within the treatment approach learned in their initial training and were more likely to adopt a new technique recommended by a personal source (a colleague, especially a mentor) versus an impersonal source (such as a journal article or a recommendation from an organization). Those interested in facilitating evidence-based treatments need to recognize and accommodate this conservatism. Training for a new therapy may be more effective if it is geared toward boosting confidence at the outset that clinicians will succeed in its mastery. Developers of training workshops might also need to emphasize ways to integrate their approaches into clinicians' existing practices to help workshop participants with integration of new knowledge. Developing confidence, or self-efficacy—an important factor in sustaining the use of treatments—may need to be promoted with the seasoned professional who is learning new techniques in the same way as it is promoted among students learning psychotherapy for the first time.
Evidence- or theory-based strategies to promote evidence-based treatments should be further investigated (
15 ). Bandura's social learning theory (
20 ) highlights the importance of observing and modeling behaviors and attitudes of others. Clearly the results of this study indicate that clinicians learned from key mentors and colleagues and perhaps imitated their behavior. Behavioral modeling may serve as a tool to aid in dissemination and implementation of innovative treatments.
Acknowledgments and disclosures
This study was supported by grant K01-MH070859 from the National Institute of Mental Health.
The authors report no competing interests.