Life in rural areas is often characterized as easygoing and lacking the stress of metropolitan living. Despite this characterization, research has consistently shown more similarities than differences in prevalence rates of anxiety and depressive disorders between rural and nonrural areas (
1 ). Indeed, anxiety and depressive disorders have deadly consequences in rural areas, given that suicide rates are markedly higher there than in urban areas (
2 ). Treatment of depression and anxiety in rural areas remains an important challenge to the heath care system of the United States.
The shortage of specialty mental health services in rural areas of the country has been well established, and primary care providers are often the only viable treatment option for rural residents (
3 ). Rural community health centers are less likely than those in urban settings to have on-site specialty mental health services and also may have more difficulty in obtaining referrals to local mental health providers (
4 ). Despite this increased role in providing mental health care, primary care physicians have acknowledged difficulties in diagnosing common mental disorders such as depression (
5 ).
Moreover, primary care providers in rural areas may have greater difficulty effectively managing disorders such as depression. Adams and colleagues (
6 ) found that a depression management program improved mental health status among depressed patients in urban primary care settings but not in rural settings. It was unclear whether the difference in treatment outcomes could be attributed to greater difficulty implementing the program in rural primary care, unique features of the rural sample, or some other variable. Surprisingly, studies examining differences in the quality of mental health care practices between rural and urban primary care settings are largely absent from the literature. One large study found that the likelihood of receiving minimally adequate mental health treatment was comparable in rural and nonrural general medical settings (
3 ). However, studies conducted in urban settings suggest that most patients with significant depression and anxiety do not receive high-quality treatment (
7 ), indicating that quality of care may be problematic in both areas.
This report provides a broad overview of the diagnosis and treatment of depressive and anxiety disorders by rural primary care providers. The study used data from the National Ambulatory Medical Care Survey (NAMCS). Practices of rural primary care providers were compared with those of urban providers. Because primary care providers are often the only option for the treatment of depressive and anxiety disorders in rural areas (
3 ), we examined differences in diagnosis rates and expected that compared with urban primary care providers, rural primary care providers would diagnose depression and anxiety in a higher proportion of visits. We also predicted that because rural primary care providers report difficulty with diagnostic precision (
6 ), a substantial proportion of the anxiety and depression diagnoses would reflect this uncertainty through greater use of the diagnoses anxiety disorder not otherwise specified (NOS) and depressive disorder NOS.
We also examined quality-of-care indicators based on criteria from the American Psychiatric Association (APA) practice guidelines. We predicted that rural primary care providers would be less likely than urban primary care providers to refer patients for counseling or psychotherapy but would not differ in rates of prescription of appropriate psychotropic medications.
Methods
Data from the 2006 NAMCS were used to test the hypotheses. The NAMCS is an annual survey of a nationally representative sample of physicians in nonfederal office-based clinical practice conducted by the National Center for Health Statistics. Physicians practicing in hospital and research settings were excluded from the survey. Participating physicians completed one survey for randomly selected patient visits over the course of one randomly assigned week. Physicians recorded information regarding patients' demographic characteristics, reason for visit, episode of care, diagnoses, medications ordered, counseling or therapy provided or ordered, and total minutes for the encounter. Physician data included specialty, practice setting (group or individual), and geographic location (metropolitan or nonmetropolitan). The response rate was 58.9%. Data for a total of 29,392 visits were gathered, but the analyses reported here included only the 11,658 visits to primary care providers.
For each visit, the NAMCS uses dichotomous variables to indicate the rural or urban status of both the physician's office and the patient's residence. Rural visits were defined as those by a patient residing outside of a metropolitan statistical area (MSA) to a physician practicing in an office located outside of an MSA. That is, both the patient's residence and the physician's office had to be located in a county with a population center of less than 50,000 inhabitants for the visit to be classified as rural. Visits that did not satisfy both of these criteria were classified as nonrural.
Physicians reported up to three diagnoses per sampled visit using ICD-9-CM codes. Patients were considered to have received a diagnosis of a depressive disorder if physicians reported major depressive disorder (296.20–296.3), dysthymic disorder (300.4), or depression NOS (311). Patients were considered to have received a diagnosis of an anxiety disorder if physicians reported panic disorder with or without agoraphobia (300.1 or 300.21), generalized anxiety disorder (300.2), agoraphobia without panic (300.22), social phobia (300.23), specific phobia (300.29), obsessive-compulsive disorder (300.3), posttraumatic stress disorder (309.81), or anxiety disorder NOS (300.0). Visits in which a diagnosis of both a depressive disorder and an anxiety disorder were given were included in both sets of analyses.
Because the NAMCS does not supply detailed information regarding medication regimens (such as dosage and duration of treatment) or referrals for psychotherapy (type of therapy or duration of therapy), a relatively liberal set of criteria was used to define quality-of-care indicators. The indicators for depressive disorders included referral for psychotherapy and the prescription of a psychotropic medication as recommended in practice guidelines (
8 ), including tricyclics and tetracyclics, selective serotonin reuptake inhibitors (SSRIs), monoamine oxidase inhibitors (MAOIs), bupropion, desipramine, nortriptyline, and venlafaxine. Quality-of-care indicators for anxiety disorders were similarly derived from APA's practice guidelines for obsessive-compulsive disorder, panic disorder, and posttraumatic stress disorder (
9,
10,
11 ) and included referral for psychotherapy and the prescription of SSRIs, tricyclics, and MAOIs.
Analyses were conducted with SPSS for complex samples, which allowed for consideration of the multistage sampling design used by the NAMCS to extrapolate to national estimates. The results therefore represent national estimates of visits to primary care physicians rather than sample characteristics. Chi square testing was used to examine differences in diagnosis and treatment practices between rural and nonrural visits. Tests of significance were conducted with adjusted F statistics derived from the Rao-Scott adjusted chi square statistic to consider the multistage probability design of the NAMCS.
Results
Most patients in the surveyed visits were female (57.6%) and non-Hispanic (85.5%). White patients accounted for 83.4% of patients in the visits, with smaller proportions of black (10.5%), Asian (5.6%), Native American (.6%), and multiracial (.3%) patients represented in the survey. Additional demographic information is available from the first author on request. Rural visits represented 18.3% of all visits to primary care (95% confidence interval [CI]=9.2%–24.2%). The results did not support the hypothesis that rural primary care providers diagnose depressive and anxiety disorders with greater frequency. Estimates of rates of depression diagnosis were similar in rural (3.3%, CI=2.2%–4.7%) and nonrural (2.8%, CI=2.3%–2.4%) visits and did not differ significantly. Rates of diagnosis of anxiety disorders also did not differ significantly between rural (1.7%, CI=.9%–3.3%) and nonrural (1.5%, CI=1.1%–1.9%) visits. Comorbid anxiety and depression was diagnosed in less than .01% of visits in both rural and nonrural settings.
Depressive disorder NOS accounted for 74.0% of depression diagnoses in primary care settings (CI=66.7%–81.3%). Diagnosis of depressive disorder NOS accounted for 81.2% of all diagnoses of a depressive disorder in rural visits (CI=62.0%–91.9%) and 72.5% of all depressive disorder diagnoses in nonrural visits (CI=63.5%–80.1%). The difference in these proportions was not significant between visits in rural and nonrural settings.
Anxiety disorder NOS accounted for 70.3% of anxiety diagnoses (CI=58.9%–79.6%). Among visits featuring a diagnosis of an anxiety disorder, anxiety disorder NOS was given as a diagnosis more frequently in rural settings (87.2%, CI=73.4%–94.4%) than in nonrural settings (66.8%, CI=53.9%–77.6%) ( χ 2 =6.76, adjusted F=5.99, df=1 and 58, p<.02).
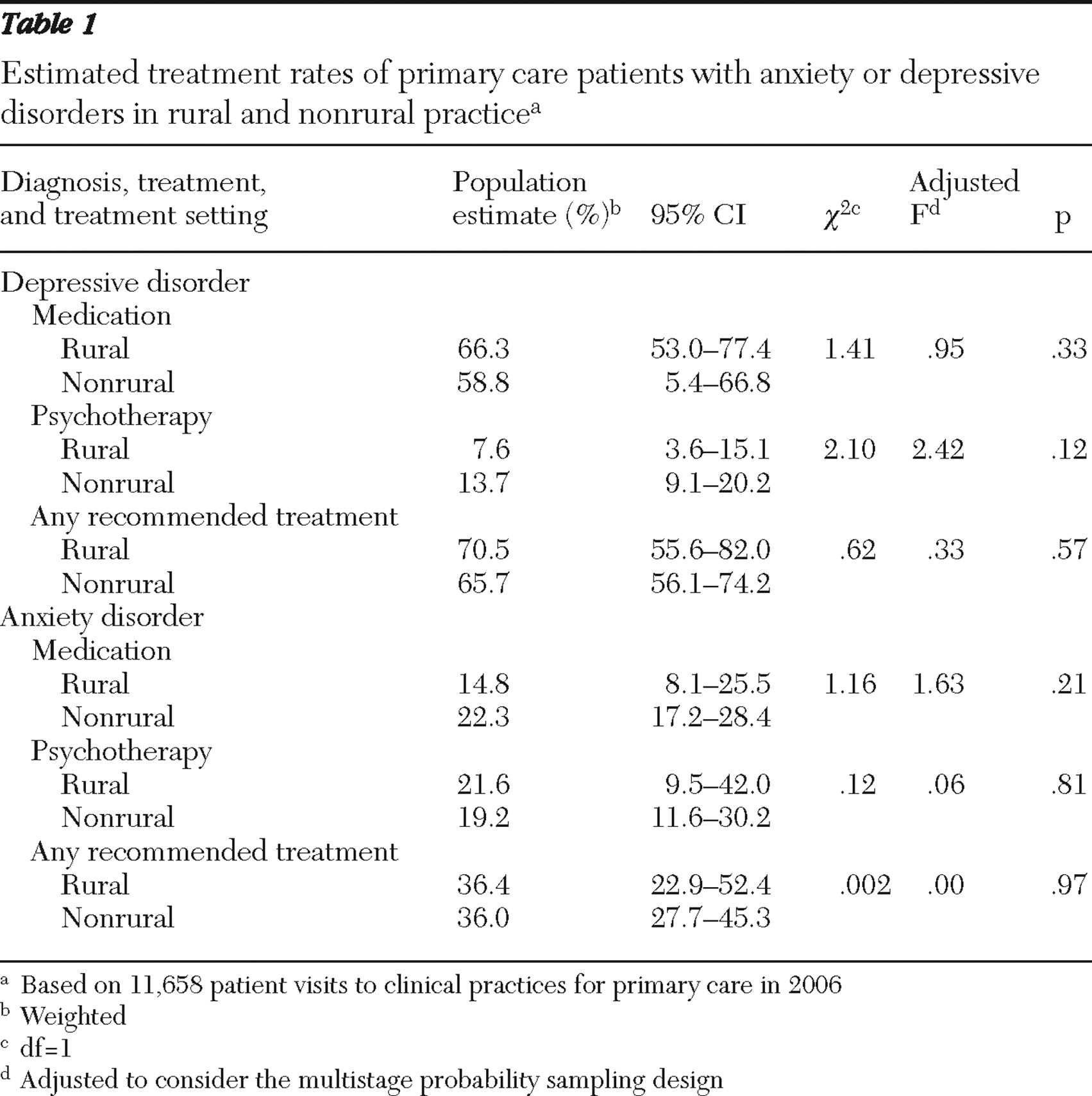
Treatment rates for patients with diagnosed depressive and anxiety disorders are presented in
Table 1 . The likelihood of receiving a prescription for a recommended medication or a referral for psychotherapy did not differ between rural and nonrural visits, nor did the likelihood of receiving any of the recommended treatment options for depressive or anxiety disorders.
Discussion
The results suggest that rural and nonrural primary care providers do not differ greatly in their diagnosis and treatment of depressive and anxiety disorders. Although the findings do not suggest that rural primary care providers are lagging behind their nonrural counterparts, they also do not paint a particularly rosy picture of mental health care in primary care practice. Our estimates indicate that primary care providers diagnosed depression in just 3% of visits and diagnosed anxiety in less than 2% of visits. The available data do not allow us to examine the percentage of patients who had undiagnosed depression or anxiety, but other studies have estimated point prevalence of clinically significant depression among patients in primary care settings at 10%–29% (
12 ). Similarly, the point prevalence of anxiety disorders in primary care settings has been estimated at 13%–20% (
12,
13 ). This strongly suggests that a majority of individuals presenting with depression and anxiety in primary care went undiagnosed.
As expected, primary care providers rarely used specific diagnoses for anxiety and depressive disorders, instead relying on diagnoses of depressive disorder NOS and anxiety disorder NOS. This nonspecific approach is especially problematic for the treatment of anxiety disorders, because recommended treatments vary by specific disorder. For example, the APA guidelines for treatment of panic disorder include use of benzodiazepines, but these medications are not indicated for the treatment of obsessive-compulsive disorder or posttraumatic stress disorder (
9,
10,
11 ). Nonspecific diagnosis is a particular concern for rural providers, because they were more likely than nonrural providers to give a diagnosis of anxiety disorder NOS.
Despite our use of broad quality criteria, a substantial proportion of patients with depression and anxiety did not receive high-quality care during their visit. No recommended treatment was provided in approximately one-third of visits by patients with a depression diagnosis and in approximately two-thirds of visits by patients with an anxiety disorder diagnosis. Rural providers did not significantly differ from nonrural providers in referral rates for psychotherapy. However, the referral rates were low in both rural and nonrural visits. Less than 15% of individuals diagnosed as having depression and less than 20% of individuals with an anxiety diagnosis were referred for psychotherapy treatment, suggesting a lack of integration generally between primary care and specialty mental health services.
Taken as a whole, these findings reiterate the need for increased awareness and action on the part of primary care providers in their role as mental health service providers in both rural and nonrural areas. Wider use of screening measures for the detection of depression and anxiety in primary care settings would be a reasonable and cost-effective approach to ameliorating this problem, at least in the short term. Long-term solutions may include more formal training during medical school or residency in the diagnosis and treatment of common mental disorders.
This study yielded several other findings worth noting. Anxiety disorders were diagnosed at a much lower rate than depressive disorders, which is particularly alarming considering that anxiety disorders have the highest national prevalence rate of any class of psychiatric disorders (
1 ). Further, anxiety disorders were less frequently treated within recommended guidelines than mood disorders, a finding consistent with research by Young and colleagues (
7 ). It is possible that awareness of depressive disorders is greater than awareness of anxiety disorders among primary care providers. Alternatively, individuals suffering from anxiety disorders may be less likely to believe that they are in need of treatment, less likely to discuss symptoms with providers, and more likely to refuse treatment. Variability in clinical presentations of anxiety disorders compared with depressive disorders may also complicate diagnosis and treatment decision making.
Finally, very few patients were diagnosed as having both an anxiety disorder and depressive disorder, which is alarming considering the high comorbidity of these two classes of disorders and suggests that primary care providers may see depression and anxiety as unrelated disorders. The low incidence of comorbid diagnoses in this data set prevented an examination of quality indicators for treatment of these patients. Future studies may wish to examine this issue in greater detail.
This study had several limitations. First, the data available from the NAMCS are not specific enough to allow for detailed examination of treatment (such as medication dosage and outcomes of psychotherapy referrals). Second, we had to collapse all anxiety disorders into a single category because of the lack of specificity of diagnoses in the data set. Therefore, we cannot speak to specific recommendations for specific disorders. Third, the use of anxiety disorder NOS and depressive disorder NOS diagnoses may be a flawed indicator of diagnostic imprecision. Rather, the widespread use of these diagnoses may instead simply reflect a shorthand diagnosis commonly used by physicians, so the conclusions regarding a lack of recognition of these disorders by providers should be interpreted with a degree of caution. There may be a lack of willingness by providers to note these disorders in the record. It is also unclear whether the definition of rurality we used adequately discriminated truly rural areas from nonrural areas. Although we used the most stringent definition of rurality available in the data set, it is possible that this definition categorized as rural many areas that are well integrated with nearby metropolitan areas. Such dichotomous classifications of rurality that do not consider adjacency to metropolitan areas have been noted as problematic and may fail to capture the heterogeneity of rural areas (
14 ).
Conclusions
Despite these limitations, the study indicated that more should be done to improve the diagnosis and treatment of depression and anxiety in primary care settings. This may be especially critical for rural primary care providers, because individuals suffering from these disorders probably face many more barriers to specialty mental health care than those living in nonrural areas (
15 ). Future research endeavors may wish to test initiatives to improve diagnosis and treatment of these common disorders and consider the unique challenges faced by both rural and urban primary care settings (
6 ).
Acknowledgments and disclosures
The authors thank Dianne Chambless, Ph.D., for her helpful comments during the preparation of the manuscript.
The authors report no competing interests.