Childhood abuse experiences and their potential role in the etiology, presentation, and treatment of adult psychiatric disorders are the focus of much current interest and speculation. Although the literature reflects a growing awareness of the prevalence of childhood physical and sexual abuse in various adult psychiatric populations (1-5), the clinical implications of this finding for specific disorders remain unclear. The link between childhood abuse and adult psychiatric symptoms is perhaps best established for the dissociative disorders (
6,
7), and some researchers have proposed that treatment is most successful when the abuse experiences are addressed directly in psychotherapy (
8).
However, childhood abuse may have different significance in other diagnostic categories and in other clinical settings. In particular, there are important gaps in current knowledge about the effect of childhood abuse on the presentation and treatment outcome of acute and severe psychiatric disorders. Some investigators, using cross-sectional assessments, have reported that childhood abuse is associated with greater overall levels of psychopathology among adults, especially symptoms of dissociation (
1,
9). Some longitudinal studies of outpatients have suggested that those with a history of abuse have an earlier onset of psychiatric problems and a more chronic course (
10,
11).
These findings, combined with the relatively high prevalence rates of childhood abuse in psychiatrically hospitalized adults, have led to the suggestion that a history of childhood abuse is an important clinical variable for psychiatric inpatients (
12,
13). However, this hypothesis is largely unexplored. Indeed, one study of adults hospitalized for first episodes of psychoses found that childhood abuse was not strongly linked to overall symptom level or degree of recovery achieved in the hospital (
14).
Affective disorders may represent a diagnostic category in which the potential impact of a history of abuse on clinical presentation and outcome is relevant. Affective disorders are among the most common psychiatric illnesses (
15) and account for a significant proportion of inpatient admissions. Adults with major affective disorders have been reported to have a 35 percent prevalence rate of childhood physical or sexual abuse (
3), somewhat above the baseline rates reported for community samples (3,16-18), raising the possibility that a history of abuse could affect the clinical presentation or treatment outcome of affective disorders. However, little systematic investigation in this area has been reported.
We hypothesized that a history of childhood abuse would be associated with more prolonged or less successful treatment of acute affective episodes. (A single diagnostic category was selected to minimize the potential confounding effects of diagnostic heterogeneity on outcome.) We examined the hospital course and outcome of major affective episodes among patients with and without a childhood history of abuse. Common measures of clinical outcome were used, including duration of hospitalization, level of functioning at discharge, amount of medication prescribed, type of discharge, and whether the patient was rehospitalized within six months. These variables generally reflect the overall complexity and difficulty of the hospital course and may have implications for service utilization or treatment planning (
19,
20).
Methods
The study was conducted by reviewing charts of patients discharged from a university hospital psychiatric unit serving an urban, publicly insured population. At the time of this study, the program did not serve patients covered by managed care programs.
All cases with a primary diagnosis of major affective episode (unipolar depression, bipolar depression, or mania) over the 15-month period from January 1991 through March 1992 were included in the study. For patients with more than one admission, only the first admission during the sampling period was examined. Patients with severe mental retardation or severe organic mental disorders were excluded. Other comorbid diagnoses, including substance use disorders, were allowed.
The final sample consisted of 110 patients, whose charts were reviewed and coded for the following data: discharge diagnoses (including comorbid axis I and II disorders), childhood sexual and physical abuse, age, gender, presence of psychotic symptoms, duration of hospital stay, number of previous psychiatric admissions, antipsychotic medication dose (in chlorpromazine equivalents per day), number of psychotropic medications prescribed at discharge, Global Assessment Scale (GAS) (
21) score at admission and discharge, and regular or irregular discharge status. Readmissions to the same hospital within six months after the index admission were also identified.
The
DSM-III-R diagnoses had been made by the treating physicians and were confirmed through chart review by one of the investigators (the first author) using
DSM-III-R criteria (
22). All other data were obtained or confirmed through chart review by a psychiatric research nurse (SH) who was blind to the hypotheses being tested.
Using a structured interview as part of the standard admission protocol, social workers assigned to the clinical team had asked all patients about childhood abuse and recorded those answers in the chart. The research nurse coded the chart data for the presence or absence of childhood physical and sexual abuse before age 16, using standard definitions of these terms (
13,
23). Childhood sexual abuse was defined as being pressured against one's will to participate in physical contact of an erotic or sexual nature, not including consensual sexual exploration between peers. Childhood physical abuse included being hit hard, kicked, punched, stabbed, or thrown such that physical injury did or could have occurred. "Emotional abuse" and "neglect" were not counted as childhood abuse in this study.
Admission and discharge GAS scores had been assigned by the treating clinicians and were confirmed by the research nurse via chart review on the basis of admission forms, discharge summaries, and progress notes. Irregular discharges included those in which the patient was discharged from the hospital against medical advice or eloped before being discharged.
The groups with and without a history of childhood abuse were compared using chi square analyses with Yates' correction for categorical variables and two-tailed t tests for continuous variables.
Results
The sample of 110 patients had the following diagnostic distribution: unipolar depression, 67 patients, or 60.9 percent; bipolar depression, seven patients, or 6.4 percent; and mania, 36 patients, or 32.7 percent. Of the 74 patients with either unipolar or bipolar depression, 29 patients, or 39 percent, had psychotic symptoms. Twenty-nine of the 36 patients with mania, or 81 percent, were psychotic. Comorbid psychiatric diagnoses included minor cognitive deficits associated with mild mental retardation or dementia, seven patients; posttraumatic stress disorder, five patients; anxiety disorders, four patients; dysthymia, two patients; and bulimia, one patient. No patients had dissociative disorders.
Fifty-five percent of the sample, or 60 patients, were female. The mean age of the sample was 44.8±16.6 years. The patients in the sample had a mean of 3.7±4.9 previous psychiatric hospitalizations.
The overall prevalence of childhood sexual abuse, physical abuse, or both was 37.3 percent (41 patients). Only a small number of subjects reported childhood physical abuse, and all of them also reported childhood sexual abuse. No group had a history of childhood physical abuse only. Analyses compared the group with childhood sexual abuse (in some cases combined with physical abuse) with the group with no history of abuse.
Patients with a history of abuse were significantly younger than patients in the nonabused group (mean= 37.8±11 years compared with 48.9± 18 years; t=4, df=108, p≤.001) and were significantly more likely to have a diagnosis of a comorbid personality disorder (34.1 percent compared with 14.7 percent; c2=4.6, df=1, p≤.05). The abused and nonabused groups were equivalent in gender distribution; number of previous psychiatric hospitalizations; frequency of nonpsychotic depression, psychotic depression, and mania; and frequency of comorbid diagnoses other than personality disorders.
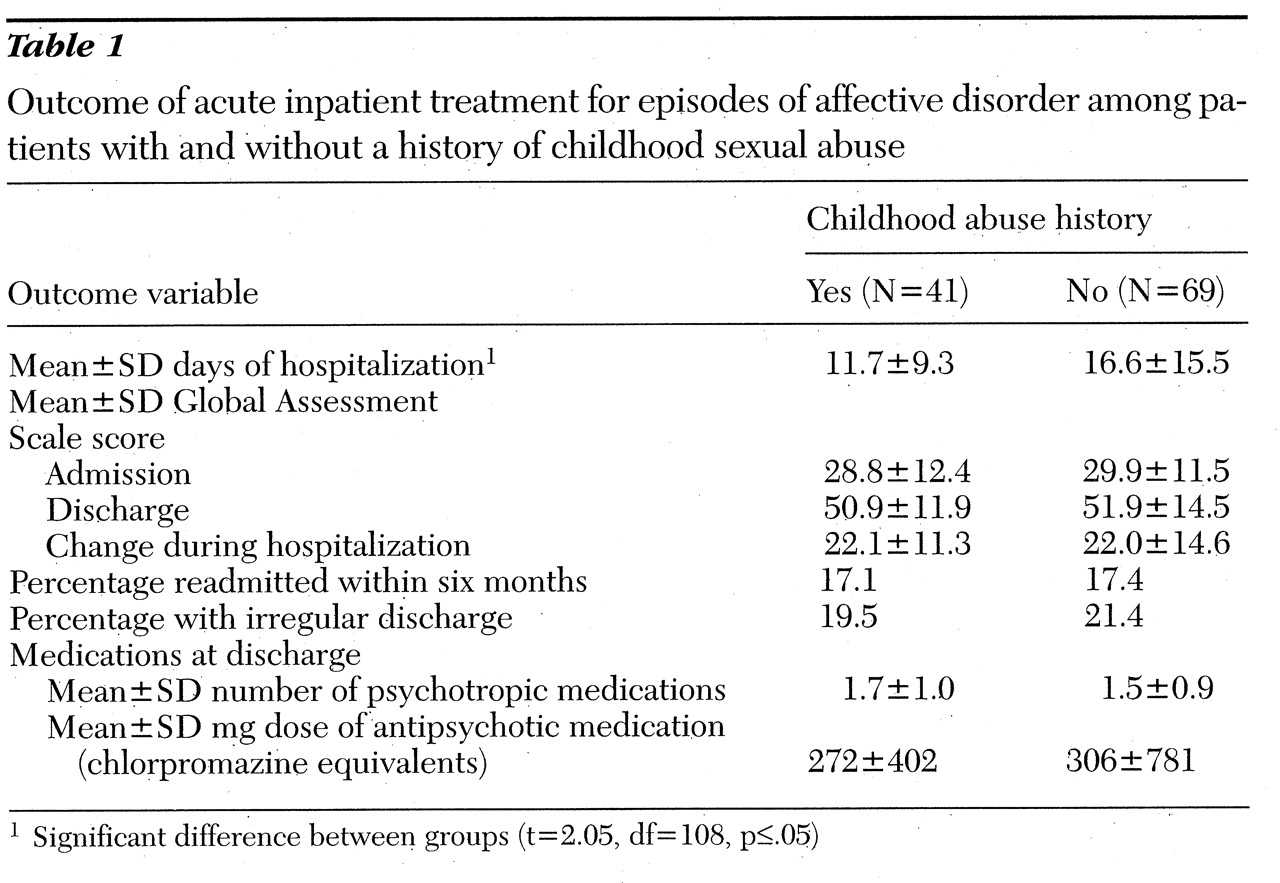
Table 1 shows data on the treatment outcome variables for the abused and nonabused groups. The group with a history of abuse differed from the nonabused group on only one outcome measure: the mean duration of hospitalization, which was significantly shorter for the abused group (11.7±9.3 days compared with 16.6±15.5 days; t=2.05, df=108, p≤.05). Other measures, including GAS scores and readmission rates, did not differ significantly between the two groups. The two groups did not differ in the proportion of patients discharged irregularly before completing their hospital treatment.
Because both younger age and shorter duration of hospitalization were found in the abused group, the possible relationship between age and length of stay in this population was further analyzed using Pearson product-moment correlation. No significant relationship between these variables was found.
Discussion
The hypothesis that a history of childhood abuse would significantly complicate hospital treatment of acute affective episodes was not supported by this study. A history of childhood abuse was not adversely related to length of hospitalization, degree of symptomatic recovery, likelihood of completing hospital treatment, or readmission within six months. Although appropriateness for discharge does not necessarily reflect complete recovery, the acute symptoms of patients with and without a history of abuse were stabilized at a similar rate.
The finding of equivalent GAS scores for the abused and nonabused groups on admission and discharge suggests that the two groups had similar levels of psychopathology and achieved a similar degree of recovery while hospitalized, at least on a global measure of functioning. Although readmission rates of the two groups to the same hospital did not differ, patients could have been readmitted elsewhere during the six-month follow-up period.
The finding of a shorter duration of hospitalization in the abused group is somewhat surprising and does not appear to be accounted for by differences in objective clinical variables such as GAS scores or frequency of psychotic symptoms. The younger mean age in the abused group also does not appear to explain the difference in length of hospitalization. Some studies have found that older age is associated with longer psychiatric hospitalizations (
20), but age and length of hospitalization were not significantly correlated in this sample. Perhaps the significantly higher prevalence of personality disorders in the abused group, consistent with studies linking early abuse to borderline personality and other axis II disorders (24-26), is relevant to the duration of hospitalization. Affective decompensations in patients with axis II disorders could be triggered more easily by psychosocial crises, which in turn might respond more readily to environmental or psychosocial interventions (
27).
Shorter hospitalizations in the abused group could also represent premature discharges related to hospital staff's negative reactions to patients with personality disorders or histories of abuse (
28). Some researchers have suggested that patients with major depression plus personality disorder receive less aggressive treatment, including less aggressive somatic treatment, than do patients with major depression alone (
27). However, in the study reported here, the similarity between the groups' GAS scores and recidivism rates and the two groups' patterns of psychotropic medication use do not support this hypothesis.
The findings of younger mean age in the abused group and an equivalent number of previous psychiatric hospitalizations suggest that patients in this group may be more vulnerable to affective decompensation at a younger age. Taken together with the finding of more frequent personality disorders, the younger mean age of the abused group suggests that childhood abuse may be associated with earlier onset of affective episodes and poorer interepisodic social functioning (27,29-31). Although this study did not find a strong association between a history of abuse and inpatient recovery from acute affective episodes, the impact of abuse may be more pronounced in the outpatient setting.
Our results are consistent with longitudinal outpatient studies suggesting that persons with a history of childhood abuse have more chronic courses of psychiatric illness. Goff and associates (
11) studied a diagnostically heterogeneous sample of 62 chronically psychotic outpatients and found that the abused group had a younger age of onset, more dissociative symptoms, and more frequent relapses compared with the nonabused group. In both a community-based sample of adult women (
29) and a longitudinal follow-up of women treated for depression (
10), "childhood adversity," including sexual abuse, parental indifference, or physical abuse, and "interpersonal difficulties" were associated with the development of a chronic course of depression.
The interpretation of these results is limited by several factors related to the chart review method. The psychiatric diagnoses were assigned by the treating psychiatrists and confirmed by chart review. This method is less rigorous than standardized diagnostic interviewing and carries the risk of missing secondary axis I or axis II diagnoses. The chart review method is especially likely to underestimate axis II comorbidity, as acute care clinicians often focus assessment and treatment on crisis stabilization and axis I disorders (
32). The overall prevalence of comorbid personality disorders in this sample—22 percent—is within reported ranges for psychiatric inpatients with affective disorders in studies using the chart review method (
27) but lower than in studies using structured diagnostic interviews (
30,
33,
34).
The method for determining whether a patient had a history of childhood abuse also warrants discussion. Social workers assigned to the study unit routinely screened all admissions for childhood abuse; thus potential bias inherent in asking about abuse based on clinical suspicion was eliminated. In this sample, the overall prevalence of childhood sexual abuse, in some cases combined with physical abuse, of 37 percent, is within reported ranges for inpatient populations in studies using similar methods (
1,
13,
35,
36). However, histories of abuse obtained as part of clinical practice may be less detailed than those obtained through research protocols with extensive interviews (
1,
12). Analyzing the outcome measures according to specific types of abuse experiences or level of severity might identify significant effects of particular aspects of childhood abuse on hospital outcome.
Also, the method of using adult recollection of childhood events without external validation carries the risk that some subjects will give erroneous information; this is a major limitation of retrospective approaches. Finally, the primary clinical rating scale used in this study, the GAS, is a global measure that reflects a variety of dimensions. It may be that significant differences in symptomatic recovery between the two groups could be detected if more sensitive and specific measures were used.
The generalizability of these results may be limited. We restricted our sample to patients with affective disorders; the findings may not apply to inpatients whose presenting complaints are directly related to traumatic events or to dissociative disorders. However, these results are consistent with those of Greenfield and associates (
14), who studied 38 adults admitted for first episodes of psychoses. They found that the group with a history of childhood abuse, 53 percent of their sample, had significantly more dissociative symptoms but was not more severely ill in general. Childhood abuse was only marginally related to longer hospital stays in their study and did not appear to affect the rate or degree of recovery from the acute episodes.
The nature of the treatment program used in the study setting may also affect the study's generalizability. In this study, all patients were treated on the same inpatient psychiatric service, which used a structured treatment approach that included pharmacotherapy, cognitive and behavioral psychotherapy, and crisis intervention targeting environmental stressors. None of the patients received treatment focusing on past abuse or childhood experiences in general.
Despite the lack of treatment directed at abuse experiences, the abused patients did not differ from the nonabused patients in improvement in symptoms during hospitalization and in readmission rate, and the abused patients had a shorter length of hospitalization. However, this study did not address the potential impact of childhood abuse on longer-term adjustment outside the hospital or later recurrences. It is possible that addressing the abuse directly in the acute treatment could actually increase the duration of the index hospitalization but decrease the frequency of readmissions and enhance interepisode functioning. This hypothesis is untested, however, and few systematic studies clearly support the efficacy of particular acute treatment approaches for persons with a history of abuse.
These results highlight the need for more rigorous longitudinal studies of the impact of childhood abuse on the presentation and treatment of specific diagnostic groups. For example, even if short-term outcomes of affective illness are not strongly correlated with a history of abuse, what about longer-term outcome? Could addressing abuse directly in the acute care setting effect more rapid recompensation, so that the abused group could recover even more quickly than demonstrated in this study? If addressing the history of abuse directly in treatment is efficacious, what are the most appropriate techniques and modalities, and what is the optimum timing?
Conclusions
The results of this study suggest that a history of childhood abuse is not strongly related to the acute outcome of adult inpatients with affective disorders. In addition, this study found no evidence that a hospital treatment model that does not address abuse directly is associated with negative outcomes in this population. The findings do suggest, however, that a history of childhood abuse may be associated with earlier and perhaps more frequent hospital admissions for affective disorders and more frequent comorbid personality disorders.