Today psychiatric hospitals must meet the challenge of reducing the costs of care while maintaining a high level of quality (
1). One approach to reducing costs is to reduce an individual patient's length of stay.
The physician, in collaboration with the treatment team (typically comprising a nurse, social worker, psychologist, and rehabilitation services representative) and the utilization review staff, usually decides how long each patient needs to remain in the hospital. One method of reducing length of stay is to repeatedly remind the physician about the need to shorten stays and make treatment as efficient as possible. To support such reminders, most inpatient facilities collect data on length of stay for the patients of each physician and regularly distribute those data to the psychiatric staff for comparative purposes. However, length of stay may not always be comparable between physicians because of clinical differences in caseloads.
To improve the utility of data on length of stay, one might determine what variables increase or decrease length of stay and then adjust the data for their effects. Multivariate analysis of data on length of stay has been repeatedly used to determine relationships between length of stay and variables related to patients' demographic characteristics and psychopathology. In a comprehensive literature review, Mezzich and Coffman (
1) found that 22 different variables influenced length of stay in various studies. Diagnosis is a common predictor of length of stay (
2,
3,
4). However, the particular diagnoses found to be predictors and the direction of their influence tend to vary across psychiatric facilities. A patient's age has also been found to be a predictor in some but not all facilities (
5,
6).
According to Choca and associates (
7), past efforts to predict length of stay using a broad range of demographic, diagnostic, and treatment variables have failed to consistently account for variance in length of stay in all hospitals. In general, the field has become pessimistic that any particular variables reliably predict length of stay across psychiatric facilities.
Nonetheless, multivariate data analysis could be an important tool in providing feedback to individual physicians about length of stay in an individual facility. If the predictor variables remain stable within a facility, such statistical techniques could be used to provide data on length of stay to individual physicians, with adjustments for differences in the clinical make-up of their patients.
We reasoned that three types of variables could influence length of stay: patient-, treatment-, and system-related variables, such as changes in reimbursement practices. In this study, we focused on patient-related variables because our facility databases contained relatively complete information for such variables. Our databases are currently being modified so that we will be able to collect data on a number of treatment-related and system-related variables, and such variables will be the subject of future analyses. The purpose of this study was to apply stepwise multiple regression analysis to our database to identify patient-related variables that remained stable over time and significantly predicted length of stay. The results of the analysis would be used to identify statistically significant differences between predicted and observed length of stay for a group of individual physicians.
Methods
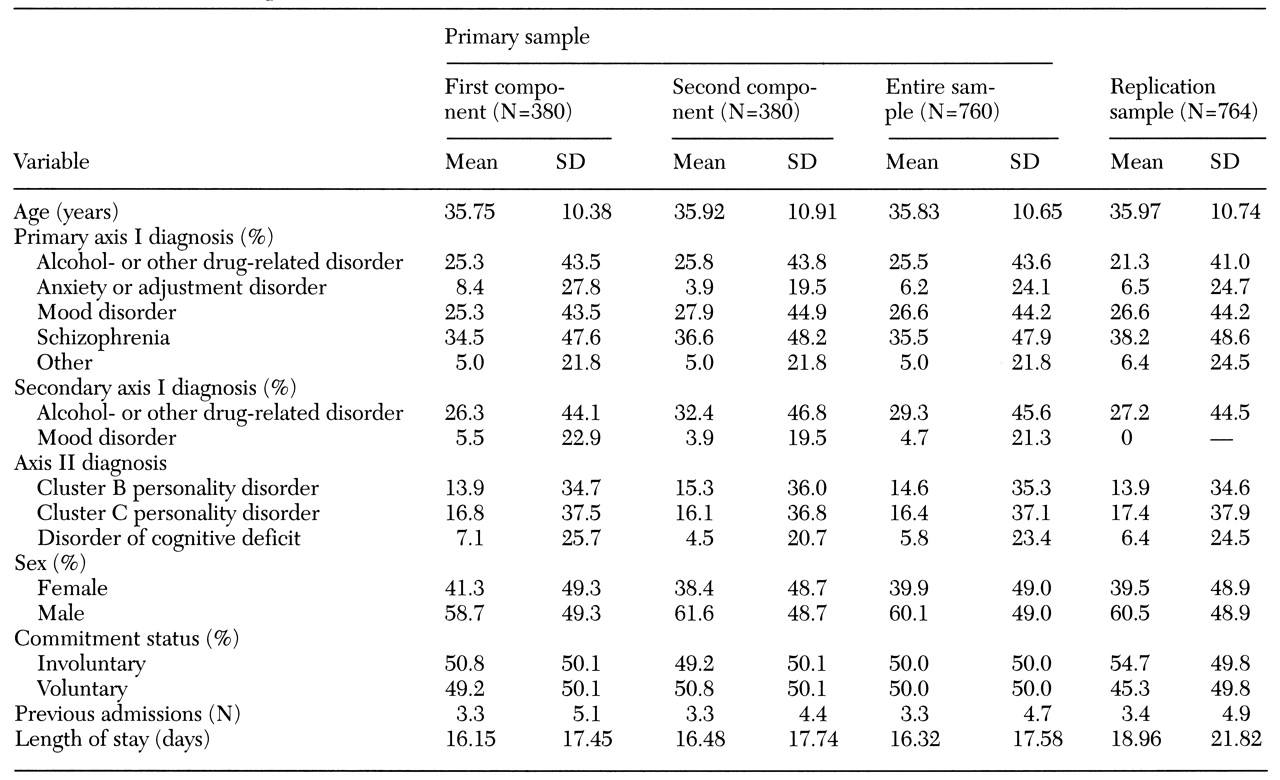
The data for this study were collected at the Metropolitan St. Louis Psychiatric Center in St. Louis, Missouri. The center provides acute psychiatric inpatient services to five eastern counties in Missouri. It has a bed capacity of 125, and during the study period the mean±SD length of stay was 16.3±17.6 days. In general, it has a relatively balanced proportion of male and female patients, 60 and 40 percent, respectively. Fifty percent of its patients are Caucasian, and 48 percent are African American. The mean±SD age of the patients during the study period was 35.8±10.7 years.
A substantial proportion of the patients at the center (about 35 percent) suffer from psychotic disorders, such as schizophrenia, schizoaffective disorder, and psychotic disorder not otherwise specified. About 25 percent have mood disorders, such as bipolar disorder and major depressive disorder. Comorbidity of these axis I disorders with secondary axis I alcohol or drug abuse or dependence occurs in about 30 percent of all patients. Comorbidity of the axis I disorders with axis II personality disorders also occurs in about 30 percent of patients.
For this study, data for 769 patients discharged between July 1, 1995, and December 31, 1995, were included in a primary dataset. The data, which were obtained from the center's internal database, consisted of each patient's age, primary axis I diagnosis, secondary axis I diagnosis, axis II diagnosis, gender, legal status, number of previous admissions, and length of stay. In addition, similar data for 764 patients discharged between January 1, 1996, and June 30, 1996, were collected in a replication dataset.
Patients admitted to the center are assigned to a physician on a rotating basis, with two minor exceptions. Court-ordered alcohol and drug admissions and patients eligible to participate in research studies are admitted to individual separate units. Taken together, these two groups of patients represent less than 10 percent of the center's admissions. Once admitted, each patient is evaluated by a physician and a treatment team to determine the patient's diagnosis, which is based on DSM-IV criteria. Other diagnostic systems are not routinely used.
Because of the assumptions underlying the distribution of values in a multiple regression analysis, patients with outlying values for length of stay, age, and number of previous admissions were eliminated from the primary dataset. These patients included two with lengths of stay of more than 180 days, three patients over age 75, and four patients who had 40 or more previous admissions to the center. Thus the primary dataset reflected a total sample size of 760 patients.
Next, the primary dataset was randomly divided into two subsets, one for derivation of the regression model and the other to test the repeatability of the regression model results. Each component of the primary dataset had a sample size of 380. Analyses were run separately on each of these dataset components and then on the entire primary dataset.
Several variables were included as candidates for predicting a patient's length of stay. In addition to age, gender, commitment status (voluntary versus involuntary), and the number of previous admissions, the variables included several axis I primary and secondary disorders and axis II disorders. Variables for axis I primary disorders were alcohol- and other drug-related disorders, anxiety and adjustment disorders, disorders of cognitive deficit, mood disorders, schizophrenia, and all other axis I primary disorders. Variables for axis I secondary disorders were alcohol- and other drug-related disorders, anxiety and adjustment disorders, disorders of cognitive deficit, mood disorders, schizophrenia, and other secondary axis I disorders. Axis II disorders were cluster A personality disorders (for example, paranoid personality disorder), cluster B personality disorders (for example, borderline personality disorder), cluster C personality disorders (such as obsessive-compulsive personality disorder), and axis II disorders of cognitive deficit (for example, mental retardation).
Several diagnostic variables were eliminated from consideration because the number of patients with the diagnosis was less than 5 percent of the total sample: axis I primary disorders of cognitive deficit, axis I secondary disorders of cognitive deficit, axis I secondary anxiety and adjustment disorders, all other axis I secondary disorders, axis I secondary schizophrenia, and cluster A personality disorders.
Results
Table 1 presents the mean and standard deviation values for all variables for the two components of the primary sample, the entire primary dataset, and the replication dataset.
Analysis of the primary dataset
A stepwise multiple regression analysis was first performed on the first component of the primary sample to derive a multivariate model to predict length of stay. The results revealed that a primary diagnosis of schizophrenia, age, a primary diagnosis of mood disorder, and the number of previous admissions accounted for 16 percent of the variance in length of stay (F=17.81, df=4,375, p<.001).
A second stepwise multiple regression analysis was performed on the second component of the primary sample to determine the repeatability of the model found for the first component. In this analysis, a primary diagnosis of schizophrenia, the number of previous admissions, a secondary diagnosis of alcohol- and other drug-related disorders, and a primary diagnosis of mood disorder accounted for 20 percent of the variance in length of stay (F=24.53, df=4,375, p<.001).
The models for both components had three variables in common that predicted length of stay: a primary diagnosis of schizophrenia, a primary diagnosis of mood disorder, and the number of previous admissions. Age contributed to predicting length of stay only in the first component, and a secondary diagnosis of an alcohol- or other drug-related disorder contributed to predicting length of stay only in the second component.
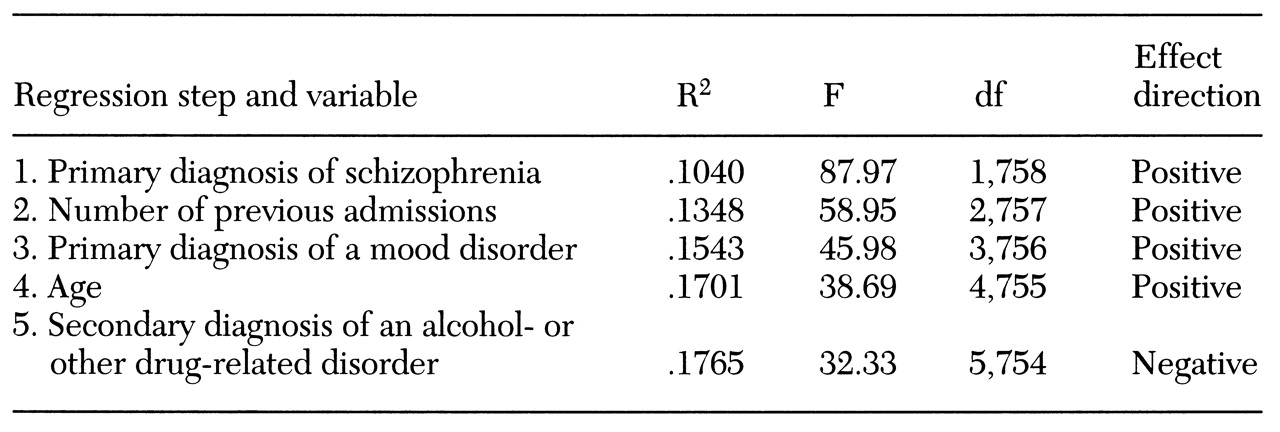
A third stepwise multiple regression analysis was then performed on the entire primary dataset. The results revealed that five variables accounted for 17 percent of the variance in length of stay (F=32.33, df=5,754, p<.001). They were a primary diagnosis of schizophrenia, the number of previous admissions, a primary diagnosis of mood disorder, age, and a secondary diagnosis of an alcohol- or other drug-related disorder.
Table 2 presents additional results from this multiple regression analysis.
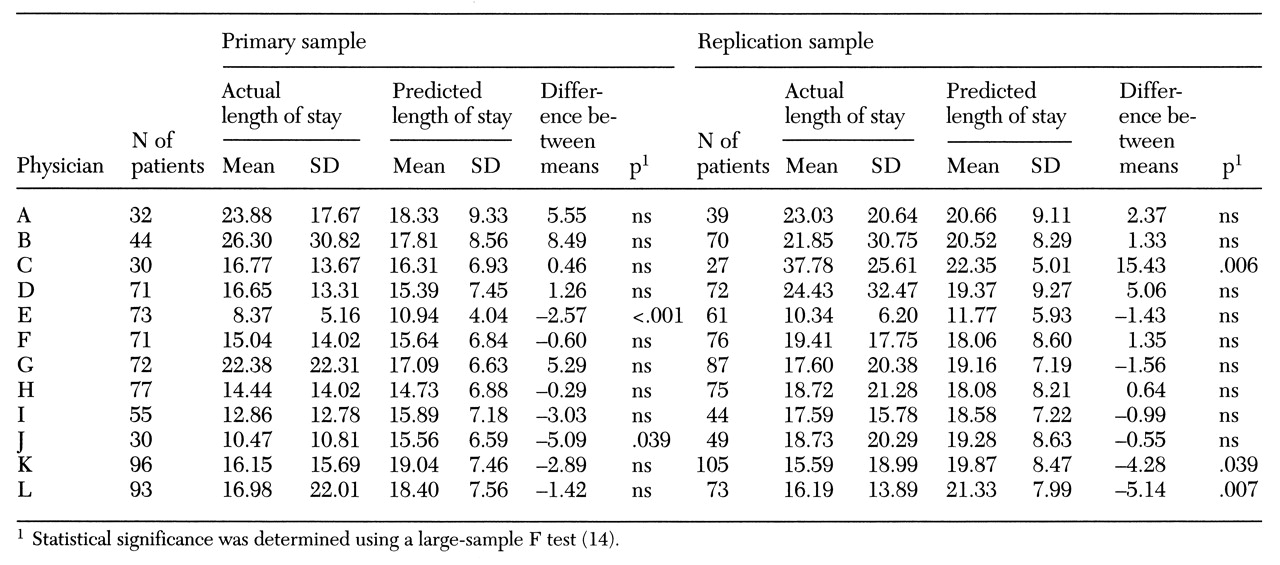
Using the equation generated from the stepwise multiple regression analysis of the entire primary sample, we then determined whether a significant difference existed between the observed mean length of stay and the predicted mean length of stay for each physician (see
Table 3).
Analysis of the replication dataset
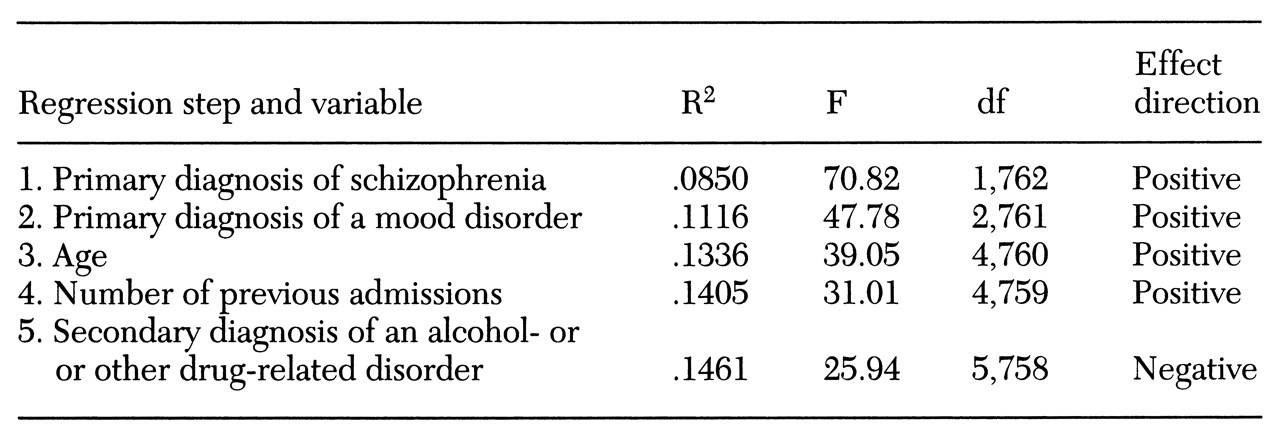
The analysis was replicated using data from the replication dataset from a second time period (N=764). As for the other analyses, data for subjects with outlying values were deleted. Results from the stepwise multiple regression analysis revealed that the same five variables from the primary sample predicted length of stay and accounted for 15 percent of the variance (F=25.94, df=5,758, p<.001).
Table 4 presents additional results of this analysis.
Using the equation generated from the replication dataset, we again compared the actual mean length of stay and the predicted mean length of stay for each physician. Results for both this dataset and the primary dataset are shown in
Table 3.
Significant differences between predicted and actual lengths of stay were uncommon. In four of five cases, the actual lengths of stay were shorter than the predicted lengths of stay. Also, in no case did the same physician have patients with outlying lengths of stay in both time periods.
Discussion
The results of this study demonstrate that patient-related predictors of length of stay in a single psychiatric hospital can be consistent across a large dataset and across two six-month periods. The percentage of variance in length of stay explained by the multivariate models ranged from 15 to 20 percent, which is in keeping with the results of other studies (
4,
5,
7,
8). Although limited, the percentage of variance explained by our model is also consistent with suggestions that an upper limit on predictive efficiency exists (
7). Unfortunately, most of the variance in length of stay cannot currently be explained (
7).
Like some previous investigators, we found that a primary diagnosis of schizophrenia (
2), a greater number of previous admissions (
1,
2,
6,
9,
10), and greater age (
5,
6,
11) predicted a longer length of stay. On the other hand, Schumacher and colleagues (
12) found age and the number of previous admissions to be only weak predictors of length of stay. Consistent with the results of Lyons and McGovern (
13) and Choca and associates (
7), but in contrast to the results of Chang and coworkers (
2), we also found that a comorbid alcohol- or other drug-related disorder predicted a shorter length of stay.
Interestingly, several variables in our dataset that our clinicians thought would be powerful predictors of length of stay were not. For example, we did not find that any comorbid axis II disorder predicted length of stay. Also, commitment status—voluntary or involuntary commitment—was not a predictor of length of stay. Such discrepancies between our results and clinical judgment, and between our results and the results of previous studies, suggest that the observations and predictions of one or even many clinical experts may be unreliable, and that predictors of length of stay may vary considerably across different hospitals (
7). Nonetheless, our results strongly suggest that patient-related predictors of length of stay in a single hospital can be stable over reasonable intervals of time and can be readily discovered using relatively simple statistical procedures.
Differences between observed and predicted length of stay for individual physicians were observed and were variable across time. As
Table 3 shows, in the cases of the physicians whose patients had statistically significant deviations from the predicted length of stay, the stays were generally shorter, and these physicians were not the same over the two time periods. The data do not suggest that the behavior of individual physicians was a significant factor in prolonging patients' length of stay.
These findings suggest that processes that had a significant impact on physicians' practice over time may already have been operating in our facility. Processes that produce change in length of stay may be unique to an individual physician—for example, the physician may treat many acutely ill patients or many patients with the same diagnosis. Alternatively, these processes may represent the interaction between an event affecting all physicians—for example, the availability of a new antipsychotic drug—and an individual physician's response to that event. The tendency for the physicians with outlying values in our study to have patients with shorter stays may also have been due to a general emphasis in our facility to shorten length of stay. Our analyses of data on length of stay should allow for a more systematic examination of such trends.
One may ask whether providing such data to individual physicians on a regular basis will, in and of itself, alter length of stay and thus reduce the costs of inpatient psychiatric care. We have begun to report data on length of stay to our psychiatric staff members and will soon be able to address such questions. In addition, one could hypothesize that the availability of new treatments and other changes in the health care system may also have a statistically significant effect on length of stay. In future studies, we will target such factors to improve our ability to account for a greater proportion of the variance in length of stay.
Conclusions
As pressures continue to mount to contain the costs of psychiatric inpatient treatment, modern tools of statistical analysis may be highly useful in identifying patient-related variables that determine length of stay. Once variance due to these variables can be understood, the length of stay of patients treated by individual physicians can be predicted. Comparisons between predicted and observed lengths of stay for individual physicians can then become a useful tool for identifying practitioners whose patients have unusually long stays and for reducing length of stay and the costs of psychiatric treatment.
Acknowledgments
The authors thank William Chase, Dean Klinkenberg, Kathy Davenport, Marie Harrison, Patricia O'Toole, Greg Dale, and Lynn Garvin-Huntley for assistance in preparing the data and reviewing the manuscript.