Discharges against medical advice (AMA) are common for psychiatric inpatients, occurring in 6 to 35 percent of cases, with a mean rate of 16 percent (
1,
2,
3,
4). Even though AMA discharges require physicians' time and can result in lack of discharge planning and scheduled outpatient follow-up, they have received little attention in the medical literature, especially in the post-
DSM-III era. Although clinical wisdom suggests that patients discharged AMA are more psychiatrically ill, less likely to be engaged in treatment, and more likely to have a poor outcome, findings about these issues are inconsistent.
The literature on AMA discharges from psychiatric inpatient units has suffered from small sample sizes and lack of a categorical diagnostic classification system. Most studies took place before managed care, when stays were longer. Finally, community support systems were not well established to provide continuing treatment for patients after discharge. Ten studies have examined characteristics of AMA discharges (
3,
7,
8,
9,
10,
11,
12,
13,
14,
15). Younger age (
3,
8,
10,
12), personality pathology (
3,
8,
12,
15), and substance abuse (
3,
10,
13,
14) have been the most consistent characteristics shared by patients discharged AMA. Socioeconomic status has been shown to be both higher (
8,
10) and lower (
11) for patients with AMA discharges. One study found higher suicidality (
8). Two studies were unable to find any differentiating characteristics of patients discharged AMA (
7,
16).
Methods
Sample
Subjects were 2,425 severely ill and largely indigent patients voluntarily admitted to three inpatient psychiatric units at a general hospital, Harborview Medical Center in Seattle, over a four-year period from April 1993 to April 1997. Because this study is based on data routinely collected as part of the clinical evaluation and care of all patients, no informed consent was obtained. Use of this routine data for research purposes is approved by the University of Washington human subjects committee.
Women made up 40.9 percent of the sample. The mean±SD age of the sample was 36.6±11.6 years, with a range of 18 to 92 years. The sample was primarily Caucasian (70.8 percent), followed by African American (20.1 percent), Asian (3.5 percent), Latino (2.9 percent), Native American (1.7 percent), and other (.9 percent). Primary axis I psychiatric diagnoses were bipolar disorder, depressed phase (342 patients, or 14.1 percent); unipolar depression (1,144 patients, or 47.2 percent); schizophrenia and schizoaffective disorder (395 patients, or 16.3 percent); acute mania (141 patients, or 5.8 percent); and other diagnoses (403 patients, or 16.6 percent)—mostly atypical psychotic, affective, and impulse control disorders. Of the 2,425 patients, 42.5 percent had a concurrent active DSM-IV diagnosis of substance abuse or dependence. The mean±SD length of stay was 11.1±8.8 days, with a range from 1 to 132 days. The median stay was nine days.
Assessments
All patients received standardized assessment batteries (
20) administered by the attending psychiatrist within 24 hours of admission and discharge. The assessment elicited information about demographic characteristics and psychiatric history.
DSM-IV psychiatric and substance use diagnoses (
21) were obtained by using a checklist of symptoms. An expanded 32-item version of the Psychiatric Symptom Assessment Scale (PSAS) (
22) was also used. Each PSAS item or subscale (for example, anxious mood) is rated on a 7-point scale, with 0 indicating not present and 6 indicating most severe. The assessment battery has been shown to be both reliable and valid for use with inpatients (
20). The internal consistency reliability was .76 for both admission and discharge.
Additional items on denial of psychiatric illness and substance abuse were also assessed. A patient's denial of psychiatric illness or understanding of illness was rated on a 7-point scale, with 0 indicating a full understanding and 6 indicating denial of problems or confabulation about the reason for hospitalization. An item on dysfunctional consequences of alcohol or drug use was rated by the attending psychiatrist on a 7-point scale, with 0 indicating no consequences and 5 or 6 indicating that the patient's use of substances shows dependence, such as compulsive use and loss of control. A variable measuring both frequency and quantity of current substance use was rated on a 7-point scale, with 0 indicating abstinence for more than 12 months and 6 indicating current use more often than weekly in a large quantity, such as consuming three or more drinks at a time or using multiple drugs.
The Mini Mental State Examination (MMSE) (
23) was administered at admission to assess cognitive functioning. The physician-rated Social and Occupational Functioning Assessment Scale (
20), which is similar to the original Global Assessment of Functioning (
21), was also administered at admission. The Lehman Quality of Life Interview (
24,
25) was administered at admission and discharge by the nursing staff using a structured interview procedure. This instrument has been shown to be reliable and valid for use with severely ill psychiatric inpatients (
26).
All irregular discharges were classified as against medical advice, including patients who were discharged by signing out against medical advice, were absent without leave, and were administratively discharged.
Statistical analyses
To compare characteristics of patients who left against medical advice and patients with regular discharges, chi square analyses were performed on categorical variables based on admission data. For continuous variables (except for age) at admission, analyses of covariance (ANCOVAs) were calculated between the groups, with age, gender, and ethnicity as covariates. Because of the number of tests, a Bonferroni adjustment of the significance level to .001 was made; values greater than .001 are presented only for descriptive purposes.
To summarize admission differences between patients with AMA and regular discharges, variables that discriminated between the groups univariately (p<.05) were used as potential predictors in a stepwise logistic regression analysis. In this analysis, the dependent variable was AMA discharge (0=regular discharge and 1=AMA discharge). The model was examined for outliers, which were removed if necessary and the model refit. Odds ratios and their 95 percent confidence intervals were calculated for the significant predictors. A risk index of significant predictors of discharge status was created.
Differences in length of stay between the discharge groups were analyzed using an ANCOVA with gender, age, and ethnicity as covariates. Chi square analyses were used to determine group differences in rates of rehospitalization after the index stay. We also determined group differences at discharge on continuous variables measuring outcome. For these analyses we used ANCOVAs, with age, gender, ethnicity, symptom ratings at admission, and length of stay as covariates. Length of stay was used as a covariate because we were interested in determining if differences in outcomes existed independently of differences due to the typically shorter stays of patients with AMA discharges. Because of the number of tests, a Bonferroni adjustment of the significance level to .001 was made.
Results
Demographic characteristics
Of the 2,425 patients in the sample, only 195 (8 percent) had AMA discharges.
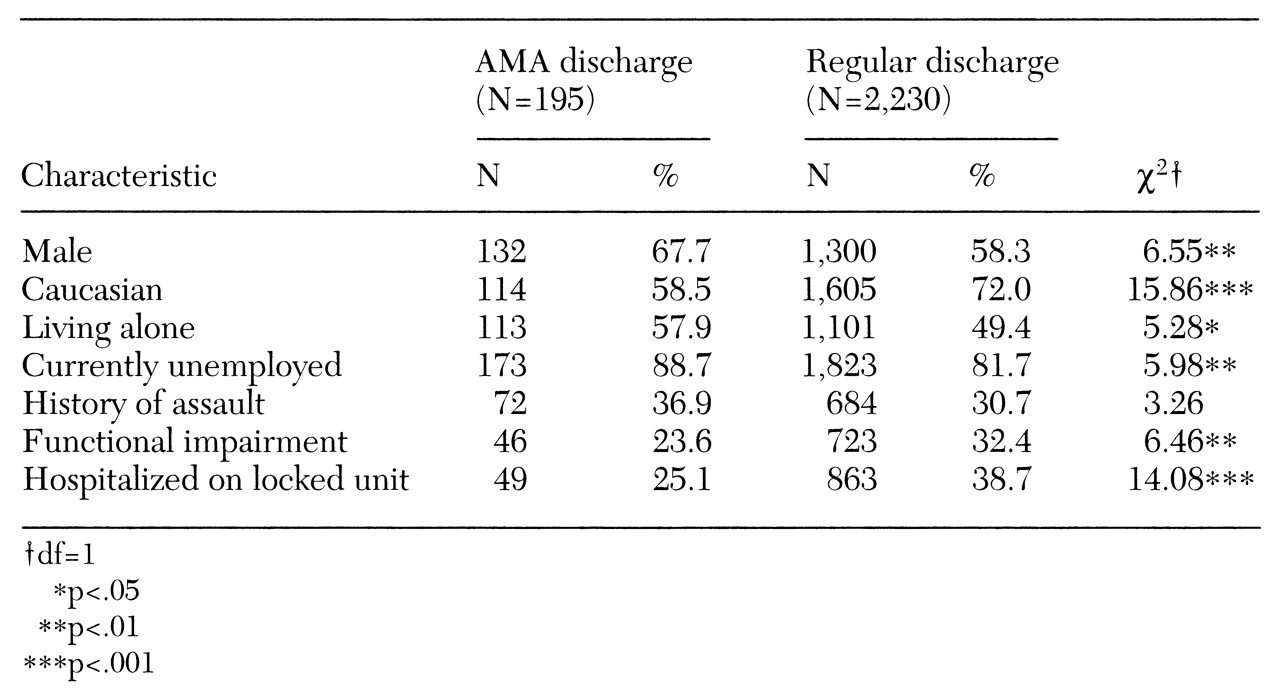
Table 1 presents information about demographic characteristics, functional impairment, and level of care for the groups. Compared with patients discharged regularly, patients with AMA discharges were significantly less likely to be Caucasian and to have been on the locked unit. They were more likely to be men and to be currently unemployed, and they were less functionally impaired by current physical illness; however, these differences were significant only at the trend level.
Characteristics at admission
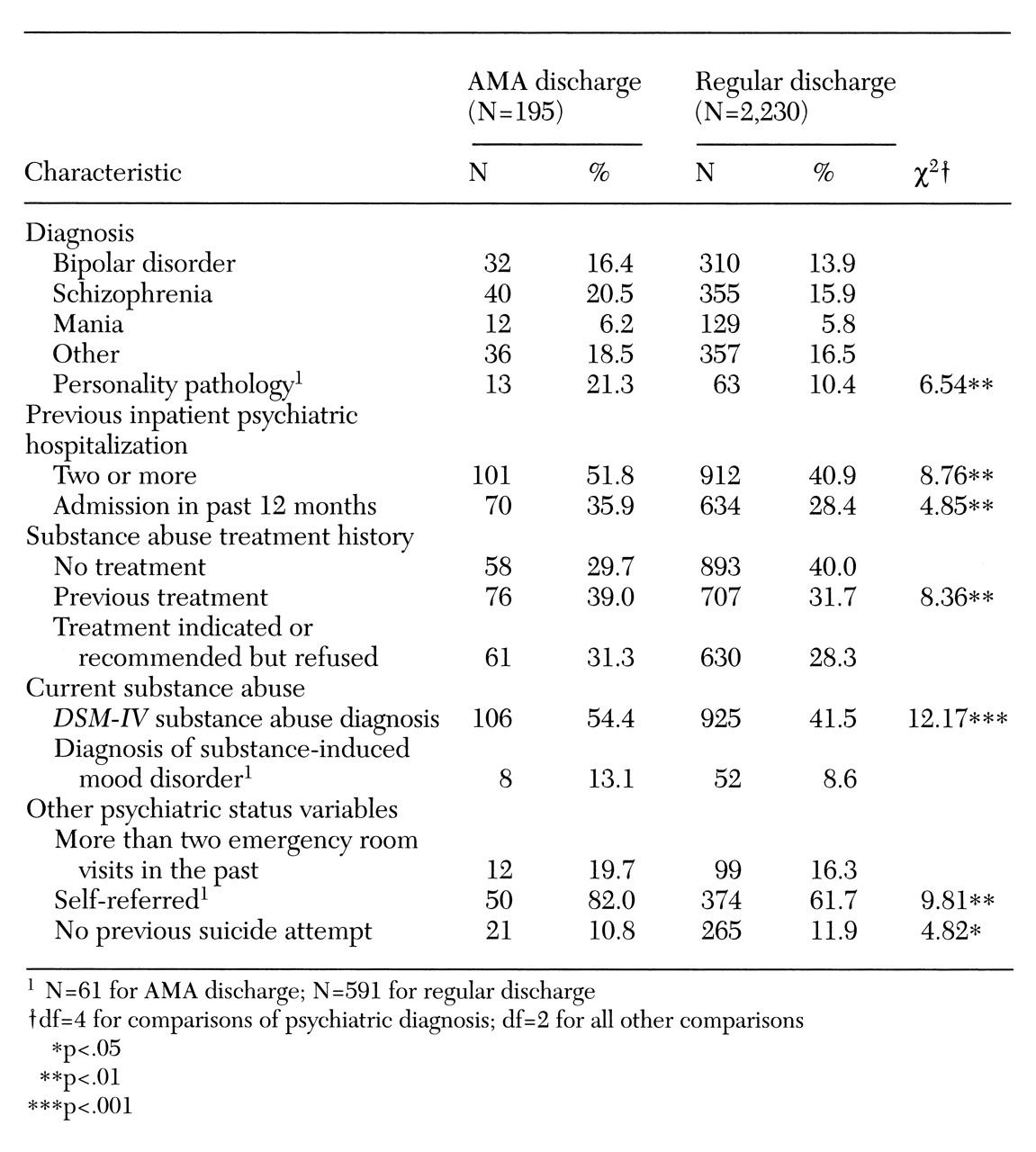
Table 2 presents information about psychiatric status and substance abuse. The discharge groups did not differ in primary psychiatric diagnoses. Although almost twice as many patients with AMA discharges had personality disorders, the difference was significant only at the trend level (p<.01). Trend-level differences also indicated that patients with AMA discharges were more likely to have two or more lifetime psychiatric inpatient admissions and to be self-referred to treatment.
As
Table 2 shows, patients with AMA discharges were significantly more likely to have a current
DSM-IV substance use diagnosis. More than half of the patients with AMA discharges had a current substance use diagnosis, compared with about 40 percent of the patients with regular discharges. No significant differences were found in the proportions of patients with a substance-induced mood disorder.
Patients with AMA discharges had a significantly greater frequency and quantity of substance use. No significant differences at admission were found in any measures of psychiatric symptoms, current functioning, or quality of life. Trend-level differences in suicidality, hostility, and dysfunctional consequences of substance use were noted. Patients who were discharged AMA tended to be less suicidal and more hostile and to have more dysfunctional consequences of substance use than regularly discharged patients as measured at admission.
Predictors of AMA discharge
Logistic regression was performed to predict discharge status from the admission variables. Fifteen variables were allowed stepwise entry into the equation: age, gender, employment status, ethnicity, residence (living alone versus with others), current functional impairment, previous inpatient psychiatric hospitalization (lifetime and past 12 months), previous substance abuse treatment, current substance abuse diagnosis, the dysfunctional consequences of substance use, the quantity and frequency of current use, suicidality, and hostility. Self-referral and personality pathology were not used because of missing data. However, a second model including these variables was tested on a reduced sample (N=652), and the results were similar. To facilitate the interpretation of the odds ratios, the continuous variables measuring substance abuse were dichotomized into low or high use and mild or severe consequences.
The overall model was significant (χ2 =62.34, df=6, p<.001) and contained six significant predictors of AMA discharge, all of which increased risk by a factor of 1 to 2. The predictors were use of a large quantity of the substance or substances abused (odds ratio=1.92, p<.001, 95 percent confidence interval=1.61 to 2.23), more than two previous inpatient psychiatric hospitalizations (OR=1.73, p<.001, CI=1.44 to 2.02), ethnicity other than Caucasian (OR= 1.86, p<.001, CI=1.45 to 2.19), absence of functional impairment due to physical illness (OR=1.47, p<.03, CI=1.12 to 1.82), male gender (OR=1.38, p<.05, CI=1.07 to 1.69), and mild to no suicidality at admission (OR=1.59, p<.003, CI=1.30 to 1.88).
The risk index created from the six predictors was significantly related to discharge status (χ2 =53.67, df=6, p<.001); scores ranged from 0 (having no risk factors) to 6 (having all the risk factors). Patients with regular discharges were nearly three times as likely as patients with an AMA discharge to have no risk factor or only one risk factor (20.4 percent versus 7.7 percent). In contrast, patients with AMA discharges were more likely than patients with regular discharges to have four to six risk factors (25.6 percent versus 16.8 percent).
Outcomes
The patients with AMA discharges had a mean<SD length of stay of 6.41<6.01 days, compared with 11.37< 8.86 for the patients with regular discharges.
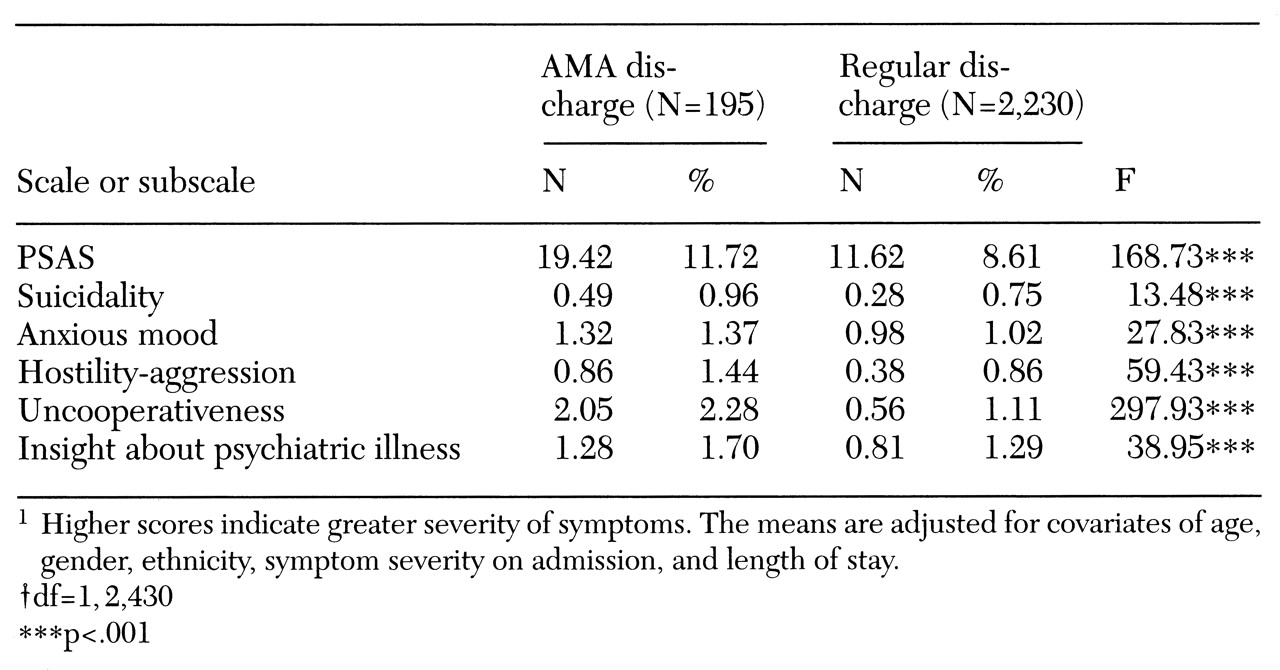
Adjusted mean scores for the total PSAS and for five of its subscales that differentiated between the two discharge groups are shown in
Table 3. Rehospitalization rates within one month of the index hospitalization were significantly greater for patients with AMA discharges (χ
2 =18.32, df=1, p<.001). Twelve percent of patients with AMA discharges were readmitted within one month compared with only 5 percent of the regularly discharged patients.
When the analysis controlled for ethnicity, gender, age, admission levels of symptoms, and length of stay, the cumulative global measure of psychiatric symptoms at discharge, as well as measures of some individual symptoms, was significantly different between the groups. Patients with AMA discharges had higher overall PSAS scores at discharge and were more suicidal, anxious, and hostile-aggressive at discharge. Not surprisingly, they were rated as four times more uncooperative than patients with regular discharges, even after the analysis controlled for level of uncooperativeness at admission. Although the groups did not differ in the quality of their denial about their illness at admission, patients with regular discharges had significantly less denial at discharge.
Although quality-of-life variables did not differ significantly between the groups, two trend-level differences were found. Patients with AMA discharges reported more satisfaction at discharge with their living arrangements and personal safety than did regularly discharged patients.
Discussion
This study measured predictors of discharge against medical advice from an inpatient psychiatric service and outcomes of patients discharged AMA. We identified six significant predictors of AMA discharge. They were use of a large quantity of a substance or substances, more than two previous inpatient admissions, ethnicity other than Caucasian, absence of functional impairment due to medical illness, male gender, and mild or no suicidality at admission. We found patients discharged AMA to have significantly worse outcomes at discharge, with higher PSAS scores, greater suicidality, and more anxiety and hostility-aggression. They were also more uncooperative and had poorer insight into their illness than patients with regular discharges.
Our study was a replication of previous studies showing an association between substance abuse and AMA discharge status. We add to this literature by showing that a greater current quantity and frequency of substance use, not merely a diagnosis of substance abuse or dependence, independently increases the risk of leaving the hospital against medical advice. We found that this high level of substance use placed patients at a two-times-greater risk of leaving AMA than patients with a lower level of substance use before admission.
Two previous studies found patients with AMA discharges to be more likely to have a history of substance abuse than patients who were discharged regularly. In one study, 61 percent of patients with AMA discharges had a history of substance abuse, compared with 47 percent of those discharged regularly (
27). In another, patients with AMA discharges were statistically more likely to have a history of alcoholism and to have been admitted for treatment of alcohol-related problems (
14).
Only one other study, on a dual disorders unit, examined the relationship between quantity of substance use and AMA discharge and found no correlation (
15). The discrepancy between that study and ours can be explained by the difference in case mix. Our sample was drawn from general psychiatric units rather than from a dual diagnosis unit, where the rate of substance use disorders was high.
Patients with multiple previous psychiatric hospitalizations were at a higher risk for AMA discharge. Hospitalization may be a way to deal with an immediate stressor. Once the stressful situation is resolved to the patient's satisfaction, the patient may request a discharge that seems premature to the psychiatrist (
9,
13). Perhaps these patients are not adequately treated during admission and come back repeatedly for episodes of partial treatment. Although we did not collect data on patients' history of AMA discharges, studies suggest that patients leave against medical advice repeatedly (
13,
18,
28).
In our sample, being other than Caucasian increased the risk of AMA discharge. Only four previous studies examined race—three found that it was not a significant predictor (
1,
2,
9), and one found African-American patients to be almost twice as likely as Caucasians to leave AMA (
29). It is unclear whether the association with race represents an independent contribution or reflects the known association between lower socioeconomic status and AMA discharge (
5,
30).
Patients who were functionally impaired by physical illness left against medical advice less frequently than those who were not impaired, probably because patients who can easily walk out of the hospital are at an obvious advantage to do so compared with those who are in a wheelchair, for example. Patients with greater functional impairment may have limited ability to care for themselves independently.
Finally, patients living alone were more likely to have an AMA discharge. Some studies have suggested that more isolated patients are at greater risk for leaving AMA than patients with stronger social ties (
11). It is possible that patients living alone do not have support available from family and friends to continue hospitalization until treatment is complete.
Our study adds to the previous literature showing that patients who leave the hospital AMA have worse outcomes than those with regular discharges. Their response to inpatient treatment was worse in that they did not improve at the same rate. This finding is similar to results of a previous study showing that although treatment response of patients discharged AMA increases with length of stay, it still falls short of that of regularly discharged patients (
16). In other words, the poorer outcome of these patients is not entirely due to leaving the hospital in fewer days.
One study found qualified support for the hypothesis that patients discharged AMA would have poorer outcomes than regularly discharged patients (
27). On two scales and at two of six follow-up points—at one year on the Health-Sickness Rating Scale and at two years on the Historical Information Form—the regularly discharged patients did significantly better than the patients who were discharged AMA. A second study found no difference in follow-up variables between patients with AMA discharges and matched controls (
7). In addition, patients with AMA discharges are rehospitalized more often than regularly discharged patients. This result has been found in four of five studies addressing this issue (
4,
13,
18,
30).
Two studies have attempted to assess the dangerousness of patients discharged AMA. One study found higher mortality among these patients (
14). The other concluded they were no more dangerous than patients discharged regularly because no casualties occurred in the group with AMA discharges (
30). Our data showed a higher level of suicidality at discharge among patients discharged AMA, which suggests a potential for greater dangerousness. This finding is consistent with other measures indicating that these patients do not improve to the same degree as regularly discharged patients. This issue is important because one reason that physicians ask patients to sign discharge papers when they leave the hospital against medical advice is their concern that patients will suffer excessive morbidity and mortality by not continuing their inpatient treatment.
The relative strengths of our study include a large sample size and the use of a standardized psychiatric assessment form to make diagnoses based on DSM-IV criteria. In addition, use of the Psychiatric Symptom Assessment Scale allowed us to collect information from each patient about a large number of symptoms, as well as a range of information about substance use and outcomes. The sample is representative of patients and lengths of stay encountered in an urban general hospital's inpatient psychiatric units.
We recognize a number of limitations of our study. The data were collected as part of routine patient care at a busy urban general hospital and not as part of a controlled prospective study. To directly measure outcome, previous studies in this area have attempted to locate patients with AMA discharges after they left the hospital, which we did not do.
An important issue is whether we can intervene to improve the outcome of patients discharged AMA even though they do not complete their hospitalization. This high-risk group (
31) must be identified early so that discharge planning can begin immediately. Perhaps a more permissive approach to these patients should be taken, because it is clear they have multiple hospitalizations. It would probably be in their best interest for clinicians to facilitate a transition to outpatient treatment regardless of their discharge status.
In an effort to facilitate this transition, Targum and associates (
32) attempted to design an intervention to reduce the rate of AMA discharges. Anticipating that such patients were more likely to be inadequately prepared for admission, to have negative preconceptions about hospitalization, and to expect hospital staff to be of no help, these authors instituted a patient advocate system to intervene when a patient asked to leave against medical advice. AMA discharges were reduced from 11.6 percent to 7.6 percent.
More attention should be paid to risk factors for AMA discharge, and we can focus future work on patients with four to six of the risk factors. Interventions should either deter patients from leaving or improve their chances of successfully following up with outpatient treatments. In this way patients may be more likely to complete treatment and less likely to repeatedly use high-cost inpatient services for crisis management.