In a health care system such as the Department of Veterans Affairs (VA) health system, appropriate treatments that facilitate a return to full occupational functioning among unemployed and underemployed individuals are potentially valuable. Not only is there a societal benefit from increased productivity of veterans, but employment may also be an important patient-centered outcome. However, there is little research on links between mental disorders and employment among veterans. Studies of the relationship between emotional distress and employment among VA service users are based on small clinic samples (
1) that are not representative of the VA patient population. Understanding how mental disorders are associated with employment among VA patients is important because these disorders are highly prevalent (
2).
Although small studies have reported a negative impact of mental disorders on employment and job performance, further research is needed (
3). Findings of VA studies are similar to findings of occupational health research conducted in nonveteran populations; these studies indicate that common mental disorders negatively influence workforce status and productivity (
4). However, studies comparing employment status of veterans receiving VA health services, other veterans, and the general U.S. population are lacking.
Mental disorders may result in early retirement among older veterans and increased unemployment among younger veterans. For younger veterans, recent military service may be a source of significant job stress, which may be related to both mental disorders and poor work performance (
5). For older veterans, persistent mental distress may be associated with more negative work outcomes than acute episodes, which are more likely to improve with time or treatment (
6). Because VA patients are more likely to have service-connected disabilities or limited income (which qualifies them for benefits), the relationship between mental disorders and employment status may be unique and complex in this vulnerable group of veterans.
Mental health may be associated with both staying in the military workforce and acquiring civilian employment after military service (
7). Studies have demonstrated the benefits of psychiatric treatment in improving work functioning among individuals with emotional disorders (
8), and access to VA psychiatric care may be associated with improved employment outcomes for veterans. Given the crucial role of employment in readjustment to civilian life for military personnel and the importance of decreasing long-term disability and early retirement among veterans, it is important to understand both mental distress as a potential barrier to employment and the benefits that may be associated with treatment.
This study examined the employment experiences of veterans and evaluated the relationship between mental health and employment status in a nationally representative sample of veterans who received VA health care. The study also provided important information by comparing the employment status of VA patients, other veterans, and the general U.S. population.
Methods
The Survey of Healthcare Experiences of Patients (SHEP) evaluates the quality of VA patient care and solicits patient responses to questions about their most recent outpatient treatment episode in the VA health care system. It is a mailed survey that uses a stratified random sample without replacement design to ensure that the sample is representative of patients seen in primary and specialty care (
9).
To be included in the study sample, veterans needed to have completed the SHEP during fiscal year (FY) 2005, have valid employment data during that period, and be of working age (18–64 years). Survey data were linked to VA administrative data on diagnosis and sociodemographic characteristics. We also included 2005 data from the U.S. Bureau of Labor Statistics (BLS) on the employment status of nonveterans and of veterans in the U.S. population (
10).
The dependent variable was employment status, which was based on a SHEP question about whether the respondent was currently employed for wages, self-employed, looking for work and unemployed for more than one year, looking for work and unemployed for less than one year, a homemaker, a student, retired, or unable to work. Respondents are allowed to mark all responses that apply. On the basis of prior research on labor force participation (
11), we created mutually exclusive employment categories (employed, unemployed, "other employed" [a homemaker or a student], disabled, or retired). The BLS defines "in the labor force" as either being employed or unemployed and "out of the labor force" as being disabled, retired, or other employed (
10).
The key independent variables of interest were diagnoses of mental disorders. We used
ICD-9 diagnoses in administrative data to identify patients with anxiety disorder, depression, bipolar disorder, posttraumatic stress disorder (PTSD), schizophrenia, or a substance use disorder during the study period (October 2004–September 2005). [A list of the
ICD-9 diagnosis codes is available in an online appendix to this brief report at
ps.psychiatryonline.org.] Covariates of interest included age, gender, service-connected disability (yes or no), general medical comorbidities measured with the Charlson Comorbidity Index (
12) (a validated mechanism for conducting risk adjustment using administrative databases), an indicator of whether the veteran had participated in Operation Enduring Freedom or Operation Iraqi Freedom (OEF-OIF), race (white or nonwhite), marital status (married or not married), and education level (less than college education versus at least some college).
We present descriptive statistics on the employment status of VA patients, veterans, and nonveterans in FY 2005. We compared demographic and clinical characteristics of VA patients by employment status using chi square tests and t tests. We conducted a multivariable multinomial logistic regression analysis to model the association between mental disorders and employment status (employed, unemployed, other employed, disabled, or retired), adjusting for sociodemographic characteristics. Sample weights adjusted for survey nonresponse and for complex sampling design.
Results
Survey data were from 98,867 patients who met eligibility criteria; they represented 5,954,262 VA patients nationwide. Employment status was as follows: disabled, 36%; employed, 35%; retired, 20%; unemployed, 7%; and other employed (student or homemaker), 2%. VA patients had a lower rate of labor force participation than both the general nonveteran U.S. population and the overall veteran population: 42%, 78%, and 81%, respectively). [A table with comparative data is available in the online appendix at
ps.psychiatryonline.org.]
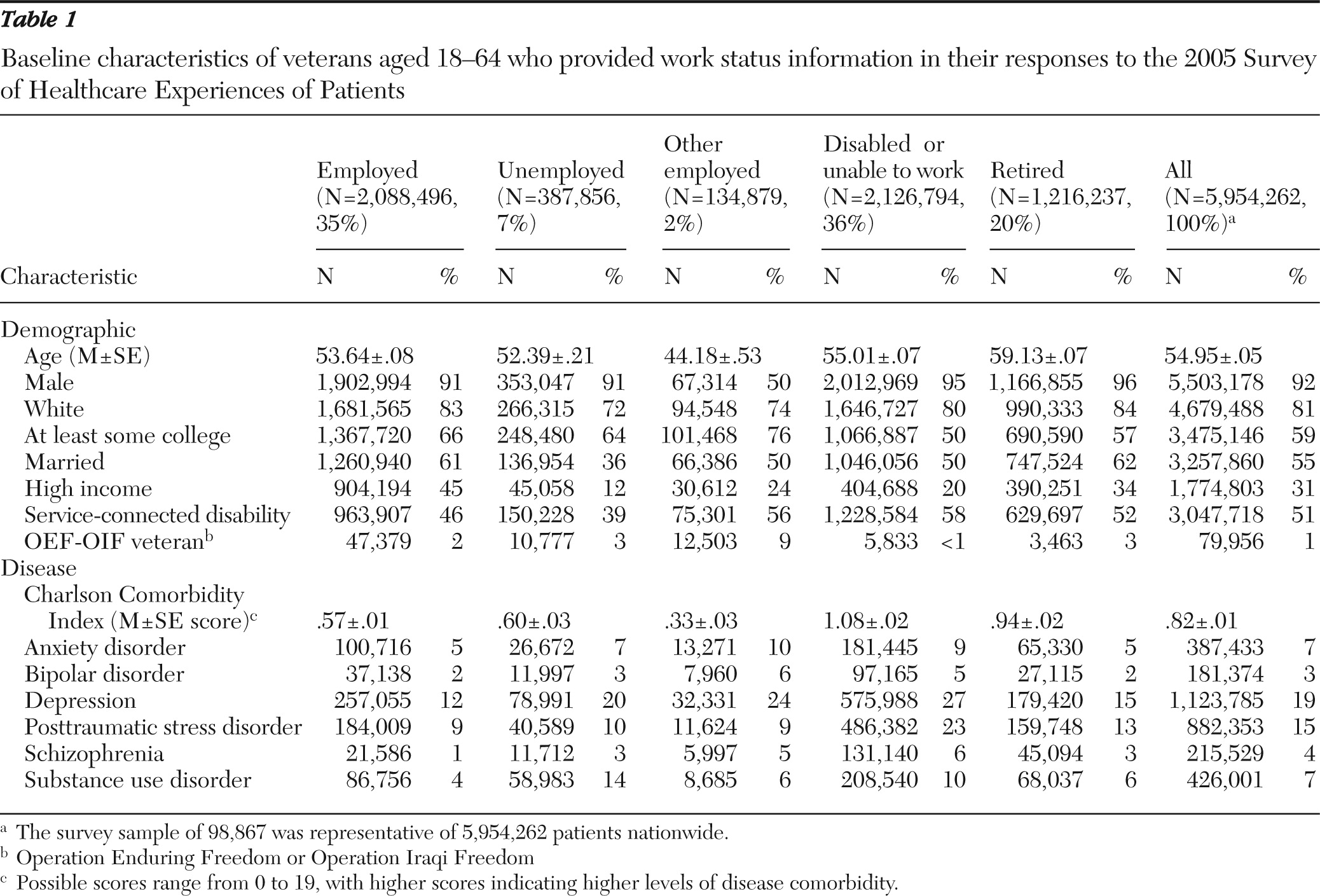
Demographic and clinical characteristics associated with work status among VA patients are shown in
Table 1. Compared with all other employment status groups, retired respondents were more likely to be male and white, whereas students or homemakers were more likely to be women. SHEP respondents in the labor force were more likely than retired or disabled veterans to be college educated. Unemployed persons were less likely to be married and had lower income than all other groups. Disabled VA patients had the highest rates of service-connected disabilities and the greatest number of medical comorbidities. The group with the largest proportion of OEF-OIF veterans was students or homemakers.
Mental disorders were highly prevalent among these VA patients: 19% had depression, 15% had PTSD, 7% had a substance use disorder, 7% had anxiety, 4% had schizophrenia, and 3% had bipolar disorder. Rates of all mental disorders were highest in the disabled population (except for bipolar disorders, which were highest in the other employed group), whereas substance use disorders were highest among the unemployed.
Results from multinomial logistic regression analyses adjusted for clinical and demographic characteristics indicated that rates of mental disorders among VA patients were significantly higher among those who were unemployed, disabled, retired, or students or homemakers than among those who were employed. [A table presenting results of these analyses is available in the online appendix at
ps.psychiatryonline.org.] Compared with employed patients, VA patients who were disabled were more than five times as likely (odds ratio [OR]=5.6) to have schizophrenia, followed by PTSD (OR=2.5), bipolar disorder (OR=2.2), and depression (OR=2.0). Those who were unemployed were twice as likely as employed patients to have schizophrenia or a substance use disorder (OR=2.2 for both) Patients in the retired group were more likely than employed patients to have schizophrenia (OR=3.4) or PTSD (OR=1.5).
Discussion
VA patients were much less likely to be in the labor force than veterans in the overall U.S. population and persons in the nonveteran U.S. population. Although many VA patients in this sample were old enough to retire (58%), the results indicated that the working-age veterans were a relatively disadvantaged population with potentially unique service and supportive care needs. The results highlight the disabling nature of mental disorders among VA patients; such disorders are substantially more prevalent among veterans than in the general population (
13).
The large proportion of VA patients who were not in the work force as a result of being disabled (36%) deserves further discussion. Veterans may qualify for VA benefits on the basis of a disability; however, receipt of these benefits may be a disincentive for seeking employment. Although being disabled may decrease the likelihood of employment, veterans may be afraid of losing their benefits and avoid entering the workforce even if they are physically or emotionally capable of doing so (
14). The relationship between VA disability payments and employment is undoubtedly complex, particularly among veterans with mental disorders who could benefit from supported employment opportunities but may also have valid concerns about the financial impact of employment on access to benefits.
This study took advantage of a large survey conducted in the VA and its linked administrative data. However, it had several limitations. Because the data are cross-sectional and we did not have repeated measures of employment status, we cannot determine how mental disorder status or employment status influenced each other over time. Future work should assess rates of treatment and follow-up care to determine whether treatment for mental disorders influences work status and decreases disability. The survey data analyzed were collected during 2005, and thus we have limited information on veterans from the Gulf War II era—veterans who served from September 2001 onward—who accounted for only 1% of the sample. However, our data indicate that veterans in this group were more likely to be employed than to be disabled or retired and were no more likely than other VA patients to be unemployed.
Finally, it is important to remember that the majority of veterans do not receive VA health care; those who do are often poor or have service-connected disabilities. This helps explain the much lower prevalence of employment in this VA sample. However, the sample may not be representative of all VA health service users because some VA patients did not complete the SHEP survey or receive VA care during the study period. However, a strength of this study is that we identified a high-risk population of veterans who may be in need of services to help them improve their mental health and their ability to gain and maintain employment.
Conclusions
This study has provided important new findings about the relationship between mental disorders and work force participation in a national sample of veterans treated in the VA health system. The results indicate a negative relationship between mental disorders and employment among veterans. Future research should assess the relationship between mental disorders and work experiences over time, including the influence of work environment, type of job, and supportive employment programs or work therapy.
In addition, more studies of the impact on employment outcomes of particular clinical services or interventions are needed. Research indicates that veterans with substance use disorders who completed a vocational rehabilitation program were more likely to be employed than those who did not complete the program (
15). Supported employment services have traditionally focused on patients with serious mental illness; however, given the high prevalence of depression and the relatively similar burden that both serious mental illness and depression had on unemployment in this study, it may be worthwhile to expand the focus of return-to-work programs to veterans with any mental disorder and to target unemployed veterans, who may be most able to resume employment. Future research should examine the employment experiences of veterans to obtain better data on their experience in the workforce. This work would allow health providers and policy makers to better understand challenges or barriers associated with employment among veterans and help them target treatments to the unique needs of veterans.
Acknowledgments and disclosures
This study was funded in part by the Health Services Research and Development Service (HSR&D), of the Department of Veterans Affairs (CD2 07-206-1 and HSR&D 07-115).
The authors report no competing interests.