The lifetime prevalence of posttraumatic stress disorder (PTSD) has been estimated to be between 8% and 14% in the general population (
1). However, the prevalence of PTSD among those diagnosed as having severe mental illnesses, including schizophrenia, bipolar disorder, and severe unipolar depression, is much higher. People with severe mental illness are more likely to have experienced abuse in childhood and are more likely to be victimized in adulthood than the general population (
2,
3). In studies conducted in mental health clinics, 48% to 98% of clients with severe mental illness reported having experienced at least one traumatic event (
4–
6), and 19% to 43% were diagnosed as currently having PTSD (
6,
7).
Untreated PTSD among individuals with severe mental illness is linked to increased symptom severity for both the PTSD and the comorbid disorder, increased hospitalization, extended treatment, poorer overall health outcomes, increased likelihood of being diagnosed as having substance use disorders, and tendency to use expensive psychiatric services (
8,
9).
There has been minimal investigation of standard PTSD treatments, such as prolonged exposure and cognitive-processing therapy, among severely mentally ill populations. One study found cognitive-processing therapy to be as effective in treating PTSD among clients with and without major depressive disorder (
10). A randomized trial compared usual care for PTSD plus cognitive-behavioral therapy versus usual care alone among a sample of clients with severe mental illness (schizophrenia or schizoaffective disorder, 16%; major depression, 61%; and bipolar disorder, 23%). The addition of cognitive-behavioral therapy was found to reduce PTSD, anxiety, depression, and other psychiatric symptoms more than usual care alone; it did not eliminate the PTSD diagnosis or all mental health problems (
11).
Another study incorporated exposure therapy within a multicomponent, cognitive-behavioral intervention developed to treat those with severe mental illness, specifically, schizophrenia or schizoaffective disorder, and PTSD (
12). Of those who completed treatment (N=13), 77% (N=10) no longer met PTSD criteria at the three-month follow-up. Thus it seems that treatment can result in substantial symptomatic change, and expansion of PTSD treatment has been recommended in treatment settings for persons with severe mental illness (
1,
13).
Despite the high prevalence rate of PTSD and the existence of effective interventions, PTSD remains underdiagnosed and inadequately addressed, especially for those with severe mental illness. PTSD and traumatic experiences are often undocumented and likely unrecognized by mental health clinics (
14). Several studies have shown that only a fraction of clients, a mere 2% to 5%, with PTSD had a PTSD diagnosis in their medical record (
6,
15,
16). The lack of attention and treatment may be due in part to funding limitations among community mental health clinics. However, one study found that clinicians were aware that PTSD is scarcely addressed in this population and that trauma has adverse effects on clients (
17). They agreed that PTSD needs to be systematically addressed but reported having little confidence in their abilities to effectively treat it in this population. They also reported fearing discussing traumatic experiences with clients with severe mental illness because of a general perception that bringing them up would worsen clients' psychiatric symptoms or appear insensitive. In addition, clinicians reported having little or no training about how to effectively bring up, discuss, and treat trauma in this population (
17).
Another reason for the underdiagnosis of PTSD among those with severe mental illness is that clinicians first address other psychiatric symptoms, such as delusions and hallucinations, that are considered more detrimental than trauma-related problems (
18). However, these clients often state that PTSD symptoms co-occur with the onset of psychosis (
16). One study found that PTSD symptoms are commonly reported in reaction to both the experience of psychosis and to the inpatient and outpatient treatment of psychotic symptoms (
16).
Findings suggest that a lack of self-disclosure by clients to the clinician could be detrimental to the therapeutic process (
19,
20). Self-disclosure by clients as well as available treatment are important because disclosure can predict a decrease in distress about one's symptoms as well as a decrease in concerns about life tasks such as work, school, or family roles (
19). In brief counseling, client disclosure has shown a significant negative association with perceived stress and symptomatology throughout treatment (
20).
This study examined the extent to which dually diagnosed clients with severe mental illness at outpatient community mental health facilities had disclosed their trauma history and the extent to which trauma and its consequences were a focus of treatment. It also studied whether addressing trauma in treatment was desired by the client and whether discussing trauma was experienced by the client as upsetting. It was predicted that both a desire to address trauma in treatment and the extent to which trauma was a focus of treatment would be predicted by female sex, mood disorder diagnosis (versus schizophrenia), more severe PTSD symptoms, more categories of trauma experienced, a desire to address trauma and its consequences in treatment, and being less upset when discussing traumatic experiences.
Methods
Participants
This study was conducted as part of a larger study conducted from 1998 to 1999 at a recovery and rehabilitation program integrating mental health and substance abuse treatment housed in a large outpatient community mental health center. The program served clients with severe and persistent axis I psychiatric disorders and clients who were heavy consumers of inpatient psychiatric services and who had a current or past psychoactive substance use disorder. Through the center's clinical database, all clients with continuous enrollment of at least two years and one clinic visit in the month preceding the start of the study were identified. A random subsample of 260 clients was identified and put in random order for recruitment. [The study CONSORT chart is available in an online appendix to this report at
ps.psychiatryonline.org.] Because there were only three participants without a major affective or psychotic disorder, they were not included. No one was excluded on the basis of PTSD diagnosis.
Measures
Traumatic experiences.
Traumatic experiences were measured by the Trauma Assessment for Adults (TAA) (
21–
24), an interview instrument that assesses the lifetime incidence of various traumatic events including violence in the military, accidents, natural disasters, physical assaults, sexual assaults, loss of a family member or friend to violence, and other incidents involving death or injury to oneself or one's friends or family. The TAA assesses for the presence of each trauma category, age of onset of traumas, and age of the participant when the trauma last occurred. Previous psychometric analysis (
24) demonstrated clinical utility with a small sample of adults within a mental health center as well as validity of the scale compared to medical records. The TAA has also shown adequate temporal stability and item-level convergence with existing measures of trauma history in a college and clinical sample (
23). The number of categories of trauma was included to measure the extent of trauma.
Posttraumatic stress symptoms.
Posttraumatic stress was measured by the Posttraumatic Stress Diagnostic Scale (PDS) (
25), a 49-item self-report measure that assesses the presence and severity of posttraumatic stress symptoms. Symptoms are assessed by yes or no questions regarding symptoms corresponding to
DSM-IV criteria for all traumas experienced (
26). A symptom severity score can be calculated using 17 symptom items. Total possible symptom severity scores range from 0 to 51. Scores <10 indicate symptoms of mild severity, scores 10–20, moderate, scores 21–35, moderate to severe, and scores ≥35, severe. The PDS has high internal consistency (Cronbach's
α=.91) and moderate one-month test-retest reliability (r = .74). Although the PDS was more conservative in diagnosing PTSD than an interview version of the same scale (Posttraumatic Symptom Scale Interview), it had convergent validity with a diagnosis by lay interviewers on the basis of the Structured Clinical Interview for DSM-IV (
27).
Treatment experiences.
Treatment experiences were assessed using the Treatment Experiences Questionnaire, an 11-item survey developed for this study to determine clients' subjective experience of mental health services with respect to physical and sexual assault and its consequences. Because of the large number of traumatic events experienced by dual diagnosis clients and the difficulty for clients to differentiate symptoms in relation to a particular trauma, participants were asked to report all symptoms they experienced, regardless of the traumatic events they associated with them. Participants rated each question on a 5-point Likert-type scale, from 1, not at all or not upsetting, to 5, always or very upsetting. An additional question asked how many treatment providers had addressed trauma in treatment.
Procedures
Clients were recruited by their case manager if it was determined that the study would be clinically appropriate both in terms of whether the client's symptoms would preclude being interviewed and whether participation would prove too distressing. When appropriate, the case manager facilitated contact by the study staff with the client. Trained bachelor's- or master's-level research staff completed the informed-consent process with interested individuals. Consenting participants were interviewed at that time or at a subsequent session. All measures and procedures were approved by institutional review board of the University of Washington.
Statistical analysis
Statistical analyses were completed using the SPSS data system. Several multiple regression models were used to analyze the data. Model 1, after controlling for the influence of sex, assessed the ability of primary diagnosis to predict how much community mental health care focused on trauma or its consequences. Primary diagnosis was dummy coded as bipolar disorder versus schizophrenia or major depression versus schizophrenia, and the reference group was schizophrenia. Responses to five questions from the Treatment Experiences Questionnaire were averaged to create a dependent variable for focus of treatment. The questions regarded how often trauma and its consequences were discussed in treatment and how much trauma was a focus of aspects of treatment, such as medications, contact with case managers, and exposure to group or individual therapy.
In model 2 the effect of the number of categories of trauma experienced and the PTSD severity score were added. Model 3 added a measure of the clients' desire to discuss trauma and its consequences in treatment determined by averaging responses to two items from the Treatment Experience Questionnaire about how much the client wanted to discuss trauma and the consequences of discussing trauma in treatment. Model 3 also included an average of responses to the two Treatment Experience Questionnaire items about how upsetting it felt to discuss trauma and its consequences. An alpha level of p<.05 was set to determine statistical significance.
Results
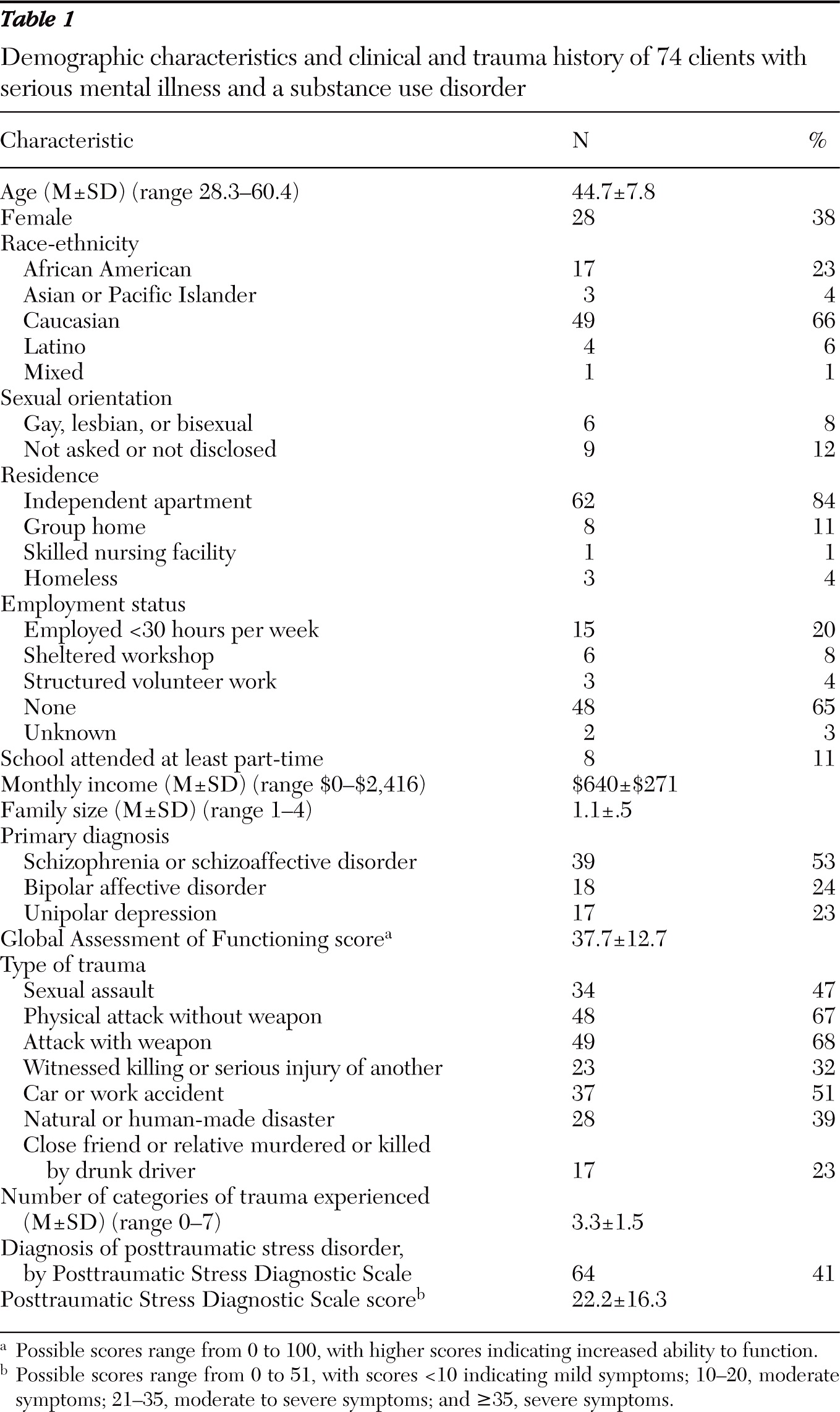
A total of 74 clients completed the assessment instruments and were interviewed for the study. Demographic characteristics and clinical and trauma history of the sample are presented in
Table 1. The majority of participants were male (62%), Caucasian (66%), and unemployed (65%). More men (N=32) than women (N=7) had schizophrenia, and more women (N=21) than men (N=14) had mood disorders. Most (53%) participants had diagnoses of schizophrenia or schizoaffective disorder, and the mean±SD score for the Global Assessment of Functioning was 37.7±12.7, indicating that a majority had major impairment in several areas of functioning. The sample was also highly traumatized, having experienced a mean of 3.3 categories of trauma.
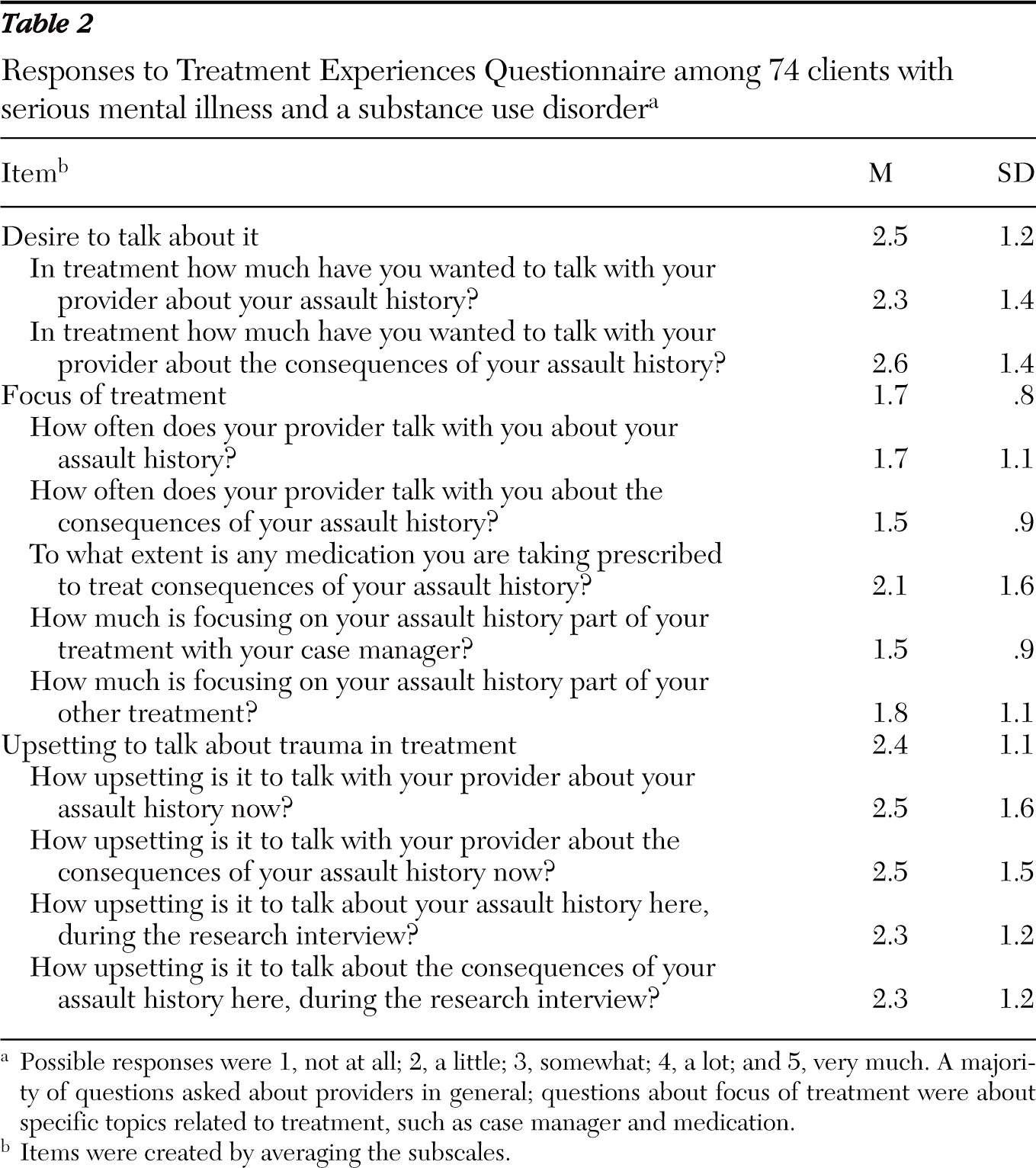
The median number of providers who asked participants about their physical or sexual assault history was zero (interquartile range 0–2 providers). Mean responses to questions about treatment experiences are presented in
Table 2. A total of 59% reported that their assault history was not at all a part of treatment; 66% reported that the consequences of trauma were not a part of treatment. Smaller proportions of participants (42% and 29%, respectively) reported not wanting to discuss assault history or its consequences in treatment. Many participants reported not being upset at all (41%) or feeling a little or somewhat upset (31%) discussing trauma with their provider. Similarly, many reported not being upset at all (34%) or feeling a little or somewhat upset (40%) discussing the consequences of trauma.
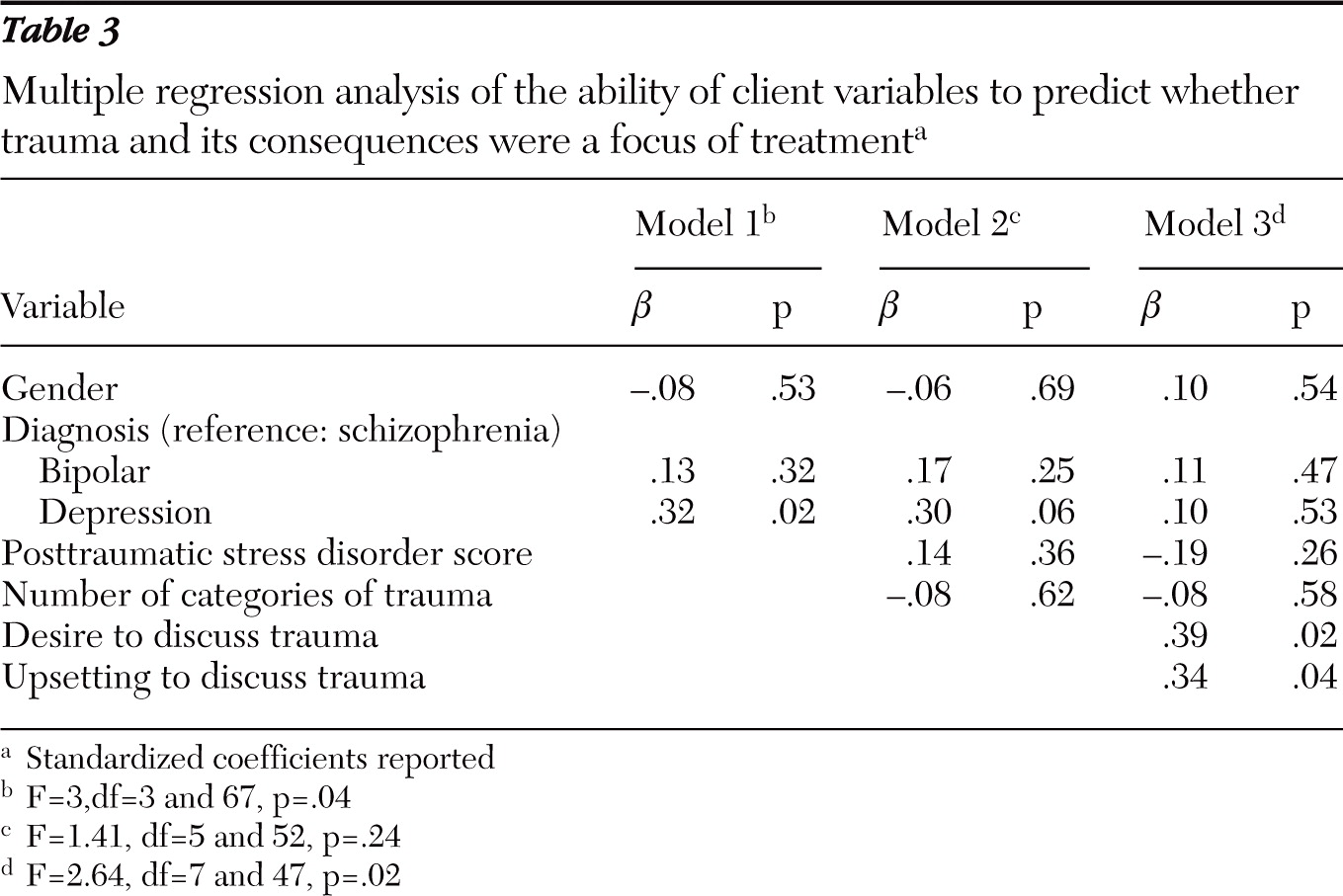
Multiple regression was used to identify the variables that might predict whether trauma and its consequences were a focus of treatment (
Table 3). Model 1, which evaluated the impact of sex and diagnosis alone, explained 12% of the total variance. In the only statistically significant finding, a diagnosis of depression was more likely than a diagnosis of schizophrenia to be related to a focus on trauma in treatment.
Model 2 evaluated four measures (sex, diagnosis, PTSD severity as measured by PDS score, and number of categories of trauma experienced) to predict how much community mental health care focused on trauma or its consequences. The model explained 12% of the total variance, but none of the predictors were statistically significant. Depression was more predictive than schizophrenia of a focus on trauma, but the trend did not reach statistical significance.
Model 3 evaluated six measures (sex, diagnosis, PTSD severity as measured by PDS score, number of categories of trauma experienced, desire to discuss trauma, and the extent to which discussing trauma was upsetting). The total variance explained by the model as a whole increased to 29%. Diagnosis was no longer a predictor, but both the desire to discuss trauma and how upset the client became when discussing trauma were significant predictors of the degree to which trauma and its consequences were a focus of treatment.
Discussion
As in previous studies, trauma and PTSD were not found to be a focus of treatment in community mental health clinics. In a previous study, clinicians reported a fear of discussing traumatic experiences with clients with schizophrenia because of a general perception that doing so would worsen clients' psychiatric symptoms (
17). A majority of clients interviewed in this study wanted to talk about trauma, at least somewhat, and were generally not upset by doing so. Thus clients' and clinicians' perceptions of whether to discuss trauma may vary.
This study found that treatment was more likely to focus on trauma among clients with diagnoses of depression than among clients with diagnoses of schizophrenia or schizoaffective disorder. Clinicians have reported having little or no training about how to effectively bring up, discuss, and treat trauma among psychotic populations (
16). Limitations in training may be a key factor explaining why clinicians made trauma less of a focus of treatment for clients with schizophrenia, although that possibility was not accounted for by this study.
This study examined factors suggested by previous research as predictors of whether trauma was a focus of treatment, including sex and diagnosis of client, diagnosis of PTSD, number of categories of trauma experienced, the client's desire to discuss trauma, and how upset the client felt when discussing trauma. PTSD severity and the number of categories of trauma experienced by the client were not predictors of how much trauma and its consequences were a part of treatment, findings that were the opposite of what was hypothesized. An alternate possibility was that avoidance, commonly seen among clients with PTSD, may have explained why those who were more traumatized did not seek help for trauma during treatment. That possibility, although not addressed by this study, should be studied in the future.
In model 3, which included all the factors, only desire to discuss trauma and how upsetting it was to discuss trauma were significant. This finding suggests that clients' direct or indirect communication with their treatment providers—rather than their symptom or trauma severity—is associated with whether trauma becomes a focus of treatment. The two client experience factors, desire to discuss trauma and feeling less upset about discussing it, were hypothesized to explain how much trauma was a focus of treatment. The results showed that desire to discuss trauma was a predictor of whether trauma was a focus of treatment, even when PTSD symptoms and number of categories of trauma experienced were not.
Contrary to prediction, the focus on trauma during treatment was greater among clients who were more upset by discussing trauma and its consequences than among those who were less upset by it. The addition of these factors in the model explained more than twice as much variance in the extent to which trauma was a focus of treatment, and diagnosis was no longer a significant predictor. A possible explanation for this result, converse to the hypothesis, is that clinicians whose clients became more upset when trauma was mentioned were cued to address it. It is also possible that clients who felt more upset by discussing their traumas became increasingly sensitive to each attempt by the clinician to address trauma, resulting in their reporting higher scores for how much trauma was a focus of treatment. Additionally, the presence of PTSD symptoms of avoidance and numbing could account for this finding, given that clients with greater emotional numbing would feel less distress about trauma; only after beginning therapy would the numbing fade and greater feelings of distress occur. However, studying these interpretations requires further research.
This study had several limitations. First, it studied a relatively small sample of clients with a comorbid diagnosis of substance use disorder. Given that participants were recruited from a clinic for individuals with severe mental illness and comorbid substance use disorder, substance use disorders may be a possible predictor and is worthy of further research of other populations and larger samples. This sample included only clients who were enrolled for two years and who were regarded by the case manager as appropriate candidates for the study who would not become overly distressed by the interview. It is possible that traumatized clients who were not eligible for the study could have had more or different patterns of trauma; therefore, the results cannot be generalized to them. In addition, the Treatment Experiences Questionnaire focuses on physical and sexual assault, rather than on all traumas, and thus is not relevant to participants who did not experience assault. Nonetheless, because 93.3% of participants did experience a physical or sexual assault, the scale is relevant to the majority of the sample.
Another limitation of this study was that all data were based on client self-report. It is possible clients underreported or misperceived that trauma was a large focus of treatment. However, evidence-based trauma and PTSD treatments frequently use exposure and other unique procedures, making it likely that clients were aware that they were receiving such treatment. Future studies should include other sources of information about treatment components and should examine ways to train clinicians to address trauma in severely mentally ill populations.
Conclusions
Treatment for persons with severe mental illness often lacks sufficient focus on trauma and its consequences, despite a relationship between the onset of symptoms following trauma and the onset of psychosis. This is partly due to the need to examine, adapt, or develop effective treatments for those with both trauma and severe mental illness. There is also a need for increased education for clinicians about the relationship of severe mental illness and trauma symptoms. This study found that factors related to the clients' experiences predicted how much a focus on trauma was a part of treatment. This finding is important for clinicians to consider when addressing PTSD among severely mentally ill clients in order to strengthen their understanding of client behaviors and to more effectively help clients decrease symptoms associated with the trauma and the comorbid disorder.
Acknowledgments and disclosures
Funding for this study was provided by grant 28-0417-C from the University of Washington Alcohol and Drug Abuse Institute. The authors thank Karin Janis, B.A., and David C. Atkins, Ph.D., for their help with the preparation of the manuscript.
The authors report no competing interests.