Mental health service providers may be at increased risk of experiencing staff burnout, a syndrome consisting of emotional exhaustion, depersonalization, and decreased personal accomplishment (
1). Burnout is frequently discussed as a problem, with studies reporting that 21%–67% of mental health workers experience high levels of burnout (
2,
3). Moreover, burnout may be on the rise because government budget cuts and revenue shortfalls have led some mental health agencies to increase staff productivity standards for billable services within a given workday.
Burnout has been associated with a range of negative work consequences, including increased absenteeism and reduced satisfaction, commitment, and performance (
4). Burnout effects can also spill over to life outside of work, with burned out mental health workers reporting more strain on personal relationships (
5), poorer health and somatic complaints (
6), and mental health concerns, such as depression, anxiety, and substance abuse (
3). Burnout can also have a negative impact on employers—and ultimately consumers—with increased employee sick days and turnover and decreased empathy, continuity of care, productivity, and effectiveness. Burnout in mental health agencies has been shown to lead to economic inefficiencies and waste (
7).
Surprisingly little research has studied interventions for reducing burnout among mental health workers. For example, a systematic review of interventions designed to improve outcomes for mental health staff in inpatient or community-based residential psychiatric units found only four studies that directly measured burnout, and two found significant between-group differences in favor of the intervention (
7). Because of the small number of studies, additional research and development are clearly needed.
We tested the feasibility and preliminary outcomes of a day-long training retreat to reduce burnout (Burnout Reduction: Enhanced Awareness, Tools, Handouts, and Education—or BREATHE). Building on a conceptual framework of burnout (Morse GM, Salyers MP, Monroe-DeVita M, et al., unpublished manuscript), we included training on mindfulness and contemplative practices as well as breathing and visualization exercises, and we incorporated materials on setting priorities and boundaries. We hypothesized that the training would result in decreased burnout, increased job satisfaction, and more positive views toward consumers.
Methods
Initially, we planned a randomized trial with a wait-list control group, but staff scheduling conflicts made randomization difficult. We then shifted to a pre-post design, whereby staff selected one of several dates of training. We also added an additional baseline assessment to examine change over time before any intervention (sequenced as an AAB within-subjects design).
Participants were employed at a public agency providing comprehensive mental health and substance abuse services in a large Midwestern city. At the time of the study, the agency had 530 employees, of which 60% were white and 79% were female. All employees, including direct-care staff, administrators, and support staff, were eligible to participate and were recruited through e-mails and flyers advertising a test of a burnout reduction program. Potential participants were directed to a Web site to learn more about the study, provide informed consent, and register for training. Once participants registered, a research assistant contacted them via e-mail to confirm participation and sent reminder e-mails before the training and the follow-up surveys.
Participants were asked to complete a baseline survey at registration and a second baseline survey on the morning of the training session (participants from the first training session completed only one baseline survey at registration). The same measures were readministered six weeks after training. Participants received a $15 gift card for each survey completed. All procedures were approved by the authors' institutional review board. Burnout was assessed with the Maslach Burnout Inventory (
8), a widely used measure of emotional exhaustion, depersonalization, and personal accomplishment. The subscales have shown good internal consistency, stability over time, and convergent validity with related constructs (
8). Job satisfaction was assessed with five items from the Job Diagnostic Survey, which has shown good internal consistency (
9) and evidence of convergent and divergent validity (
10). Intentions to leave their position were assessed by two items: “How often have you seriously considered leaving your job in the past six months?” (rated from 1, never, to 6, several times a week) and “How likely are you to leave your job in the next six months?” (rated from 1, not likely at all, to 4, very likely). Staff views of consumers were measured with the Consumer Optimism scale. Staff were asked to think about consumers with whom they currently work and estimate how many of them they expect will have specific outcomes (for example, housed or employed) on a 5-point scale ranging from 1, almost all, to 5, none, with items recoded such that higher scores indicate more optimism. This 16-item scale has good internal consistency and correlates with related constructs (
11).
The training was provided as a one-day workshop (six hours long) at a local hotel. Training included a brief introduction, burnout prevention principles, and experiential exercises and skill building in six major areas: contemplative practices (for example, mindfulness and meditation), social (for example, developing support and setting limits), physical (for example, body scan), cognitive-philosophical (for example, cognitive restructuring and values clarification), imagery, and other self-care activities. Information was presented in a lecture format, interspersed with individual, dyadic, and group activities. A conceptual framework for understanding burnout was presented and consisted of a functional analysis and steps for relapse prevention. Participants were provided with a toolkit with which they were encouraged to identify personal burnout warning signs and triggers and to outline a follow-up personalized burnout prevention plan. Each participant attended only one workshop. Attendance at the five workshops ranged from ten to 28 participants. At the end of the training day, 91% (N=76) of the participants rated the overall training as moderately helpful or very helpful.
The primary purpose of the pilot study was to examine the feasibility and preliminary effectiveness of the training program. First, we identified participants and compared them with those who registered for the training but did not attend. Next, we examined changes over time in scores related to burnout, job satisfaction, intentions to leave the position, and staff views of consumers. For the total sample, we used paired t tests to compare the results of the first baseline survey with those of the six-week follow-up. For the subsample that had two completed baseline measures (N=58), we used repeated-measures analyses of variance to examine changes over time, with post hoc comparisons between time periods.
Results
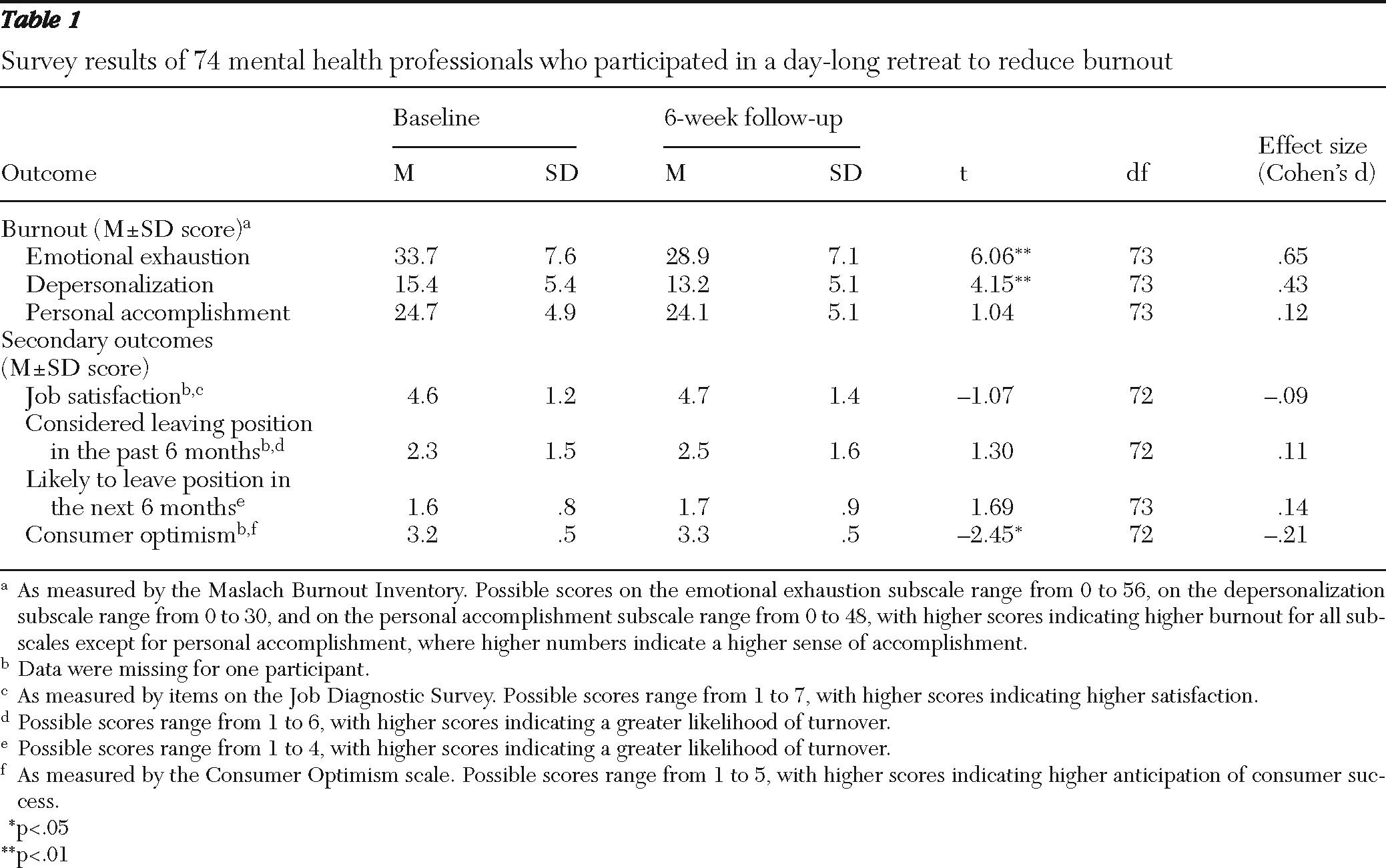
A total of 103 people registered for the training, and 84 attended a session. The 79 attendees with demographic information included whites (N=62, 79%), blacks (N=15, 19%), and persons of “other” race or ethnicity (N=2, 3%). In addition three persons (4%) were Hispanic. Most participants were female (N=69, 87%). Nonparticipants were more likely than participants to be from a racial or ethnic minority group (N=12, or 63%, versus N=17, or 22%) (p<.01) and to have a greater percentage of adults in their caseload (mean of 94%±15% versus 77%±39%) (p<.05). For participants who completed the six-week follow-up (N=74), we found significant reductions in two of the three components of burnout (
Table 1). As we hypothesized, emotional exhaustion was significantly lower at follow-up than at baseline, with a large effect size (d=.65). Depersonalization was also significantly lower at follow-up than at baseline (moderate effect size, d=.43). Personal accomplishment did not differ significantly from baseline to follow-up. Participants also reported a significant but small effect for increased consumer optimism at follow-up. Other secondary outcomes of job satisfaction and turnover intentions did not change over time. For participants who completed both baseline surveys and the follow-up (N=58), we also found significant decreases in emotional exhaustion and depersonalization and significant increases in consumer optimism. Post hoc comparisons showed follow-up scores to be significantly different from both baseline scores, but the two baseline scores did not differ from each other. [An appendix showing detailed dropout analyses and post hoc comparisons is available as an online supplement to this report at
ps.psychiatryonline.org.]
Discussion
This preliminary, quasi-experimental examination of a new burnout intervention showed promising results. We found that a one-day workshop to reduce staff burnout was well received. Of the 103 persons who initially registered, 82% attended—a positive finding in itself, given the hectic pace of community mental health work. Participants reported significant reductions in emotional exhaustion and depersonalization and significant increases in consumer optimism six weeks after the training. In a stronger test of our hypotheses, the subsample who completed two baseline assessments showed the same posttraining changes, with no difference between the two baseline assessments. This increases confidence that improvements may be related to the intervention rather than being a function of the assessment or maturation.
We found large effect sizes for reductions in emotional exhaustion, moderate effects for depersonalization, and no changes in personal accomplishment. In prior research, emotional exhaustion was the most robust dimension and diminished personal accomplishment the least robust, leading some to argue that burnout is better conceptualized as a two-dimensional phenomenon or even a single dimension of emotional exhaustion (Morse GM, Salyers MP, Monroe-DeVita M, et al., unpublished manuscript). Others, including Maslach (
12), have argued for a temporal relationship between the components, suggesting that emotional exhaustion may lead to depersonalization and later to reduced personal accomplishment. If that is the case, six weeks may not have been enough time to see changes in that dimension. Also, the training may need an enhanced focus to improve a sense of personal accomplishment.
We found little or no change in job satisfaction or intentions to leave the position—outcomes that we viewed as secondary to and distal from our intervention. Both job satisfaction and intention to leave are complex constructs, with multiple determinants (for example, pay) that were not the target of our intervention. In addition, prior studies have found mixed results in terms of burnout predicting job satisfaction or turnover (
3,
4).
The finding of increased consumer optimism is encouraging and may reflect broader benefits of the burnout intervention beyond staff morale. Other studies have shown that staff expectations of consumers are related to consumer outcomes (
13). If staff members are taking better care of themselves and feeling better, they may be able to respond more compassionately and positively toward those with whom they work. It is interesting to note that we did not explicitly include training concerning consumer expectations. However, mindfulness techniques directly targeted at reducing stigmatizing attitudes have resulted in reductions in burnout as well (
14).
Our ability to draw firm conclusions is limited by the lack of a controlled comparison group. Although a subsample completed two baseline measures, changes may not necessarily be related to enhanced skills from the training. Future studies will need to include a randomized control group and assess the effects of burnout prevention over a longer follow-up period. Positive outcomes from a one-day workshop are encouraging, but more lasting changes may require more frequent or intensive training, spaced over a period of time. We were also limited in our ability to engage and retain participants from racial and ethnic minority groups. Although minority status was not directly related to outcomes, we found an interaction such that persons from racial-ethnic minority groups had lower depersonalization scores at baseline and no significant decrease in the depersonalization score at follow-up. Emotional exhaustion decreased regardless of minority status. However, interventions may need to be adapted to encourage greater participation of racial and ethnic minority groups.
Conclusions
With a one-day workshop, we found large reductions in emotional exhaustion, moderate reductions in depersonalization, and small but significant improvements in consumer optimism six weeks later. Future work is needed to ensure acceptability and feasibility with certain populations (racial and ethnic minority groups) and to assess the durability of positive effects over a longer follow-up, but our initial work shows that the training was helpful and that participants reported using the techniques in practice. Given the demands of mental health work and the potential negative effect of burnout, successful burnout interventions are critical, and this is a promising intervention.
Acknowledgments and disclosures
This study was funded by Interventions and Practice Research Infrastructure Program grant R24 MH074670 (Recovery-Oriented Assertive Community Treatment) from the National Institute of Mental Health.
The authors report no competing interests.