Deliberate self-injurious behavior is distinct in concept from suicidal behavior and usually lacks lethal intent (
1,
2). Behaviors include cutting, burning, hitting, head banging, ingesting or inserting foreign objects, and even self-amputation or enucleation, but not tattooing, piercings, or autoerotic acts (
3). Despite absence of lethal intent, self-injurious behavior can lead to death (
4,
5). Characteristics of those who engage in self-injury in noninstitutionalized, community populations have been described (
6–
10). Nosologies proposed are based on psychopathology or context (
8), motivation (
6), or categories labeled major, stereotactic, and moderate (
9). Associated disorders include borderline personality disorder (
6), those in the autism spectrum (
11), or psychoses such as schizophrenia (
12). Community-based prevalence studies have reported a 4% rate of self-injurious behavior within adult, nonclinical samples (
7,
13) and rates of 14%–17% among adolescents and young adults (
10).
Self-injurious behavior in correctional settings may differ in situational context, incidence, intent, and environmental impact (
14,
15), and management of this behavior consumes significant clinical and custodial resources (
5,
16). Most publications on self-injury in corrections facilities are descriptive or based on case reports (
17–
20). Research has estimated that 30% of inmates engage in self-injurious behavior during their incarceration (
21), that 50% of female prisoners have a history of one or more episodes of self-injury (
22), that 75% of prison-based events consist of cutting (
23), and that 50% of incidents occur in punitive or restricted housing units (
23). The sample size or methodology (or both) used in the studies limits the generalizability of these estimates. Growing evidence reflects a strong association between self-injury and frank suicidality (
6) and overt, externally directed violence (
24,
25).
A modified correctional nosology (
15) defines categories of manipulative, angry, and dissociative self-injury. Although clinically descriptive, this approach has not been widely adopted. Several studies have defined limited characteristics of the prevalence and correlates of self-injurious behavior in correctional settings, but a national assessment of the problem in the U.S. prison system has not been conducted. The survey reported here sought information about the prevalence and nature of self-injurious behavior and interventions used to manage it, which could better inform clinicians and administrators about the extent of and response to these behaviors across the country.
Methods
Using records available online and in print, we identified statewide and federal directors of correctional mental health services and e-mailed them information about the study and a link to a 30-item questionnaire available online (available from the authors on request) that elicited information about self-injurious behavior events, including their definition, frequency, tracked data, impact on operations and resources, diagnoses, management, and the roles of mental health and custodial staff. Survey content areas were guided by a national work group on correctional mental health research (
26).
We used data from the U.S. Department of Justice's Bureau of Justice Statistics (BJS) to confirm and update inmate census statistics and collect system-specific information on operational capacity (the number of inmates that can be accommodated based on the size of a facility's staff and existing programs and services) and design capacity (the number of inmates that planners or architects intended for a facility) (
27). The National Association of State Budget Officers 2008
State Expenditure Report was used to collect system-specific corrections expenditures (
28).
Four of the study's coinvestigators with significant correctional experience (KA, RT, JM, JB) pilot-tested the initial survey. We e-mailed to the mental health directors of the 51 state and federal prison systems a letter explaining the purpose of the study and a link to the online survey. Guided by Dillman's tailored design method (
29), we e-mailed a reminder letter to nonrespondents (or their designees) approximately two weeks later. Full survey packets were mailed (or e-mailed as attachments) to nonrespondents on request for ease of completion by some states. Persisting nonrespondents were contacted approximately two to three weeks after the first reminder. Approximately one month after that follow-up, we e-mailed a personalized final letter thanking the recipients who completed the survey and offering them a copy of results once tabulated or, for nonrespondents, encouraging them to complete and return the survey. Data were collected between November 2009 and March 2010. The University of Massachusetts' Institutional Review Board approved the study and waived informed consent.
Data were analyzed with SPSS-PC statistical software, version 17.0. We used univariate statistics to describe the prison systems in our study sample and self-injurious behavior events and their management, and we used bivariate statistics to examine relationships between these variables. On the basis of whether the data were categorical or continuous, we used chi square tests, t tests, and correlation coefficients, as appropriate, to assess significance at the .05 level.
Results
Participating prison systems
Of the original 51 systems contacted, 39 (77%) responded. There was a fairly even distribution of system size and location. The populations of these systems ranged from 2,064 to 201,280 inmates, with a mean±SD of 31,421±46,824 and median of 20,661. The federal system responded, as did 12 states from the West, ten from the South, and eight each from the Northeast and Midwest. Six states refused to participate, and six did not respond. Compared with states that completed the survey, these 12 states were not significantly different in terms of prison population size, geographic location, operational or design capacity, total annual expenditures, or annual noncapital expenditures.
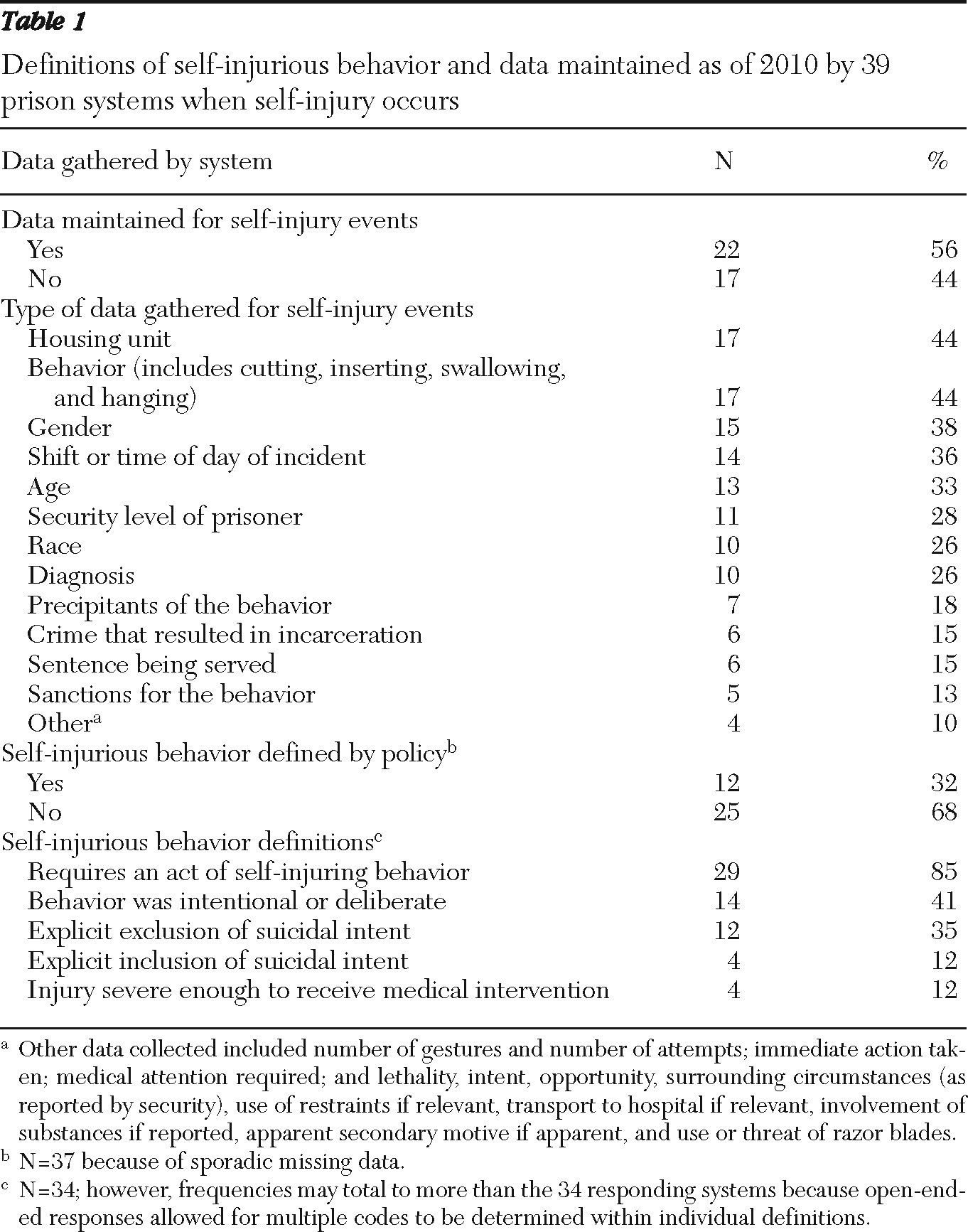
Unfortunately, only 56% of the systems that responded to the survey reported that they maintain any data on self-injurious behavior events (
Table 1). As a result, respondents often had to provide their best estimates for many questions on the survey, and not all systems responded to every item on the questionnaire, which led to a sample of less than 39 on some items. When queried whether their corrections system records specific inmate demographic, clinical, and behavioral characteristics and facility characteristics, respondents more often reported that their system collects data on the inmate's housing unit, behavior, and gender when a self-injury occurs. Less frequently collected were data on the inmate's crime, sentence, or sanctions for the self-injury incident.
Prison policies about self-injury
Just 32% of responding systems had policy definitions of self-injurious behavior. Most of the remaining systems used unwritten definitions, but five (13%) indicated that they have no definition or that they use “clinical judgment.”
Table 1 also shows the main themes within the definitions provided by the other 34 systems. Three-quarters of the systems (N=28 of 38, 74%) reported specifically that they distinguish between self-injurious behaviors and those thought to be suicidal. In 37 systems (95%), a mental health clinician can make the determination that an event qualifies as self-injurious behavior (the remaining two systems reported no data on this question). Twenty-one systems (54%) and nine systems (23%) allow medical clinicians and custodial staff to make this determination, respectively.
The number of individual inmates engaged in self-injury in each system during the previous calendar year (2008) ranged from two to 5,000 (mean±SD=321±948, median=92), representing .03%–8.93% of the prison census (mean±SD=1.30%±1.89%, median=.44%). For all 39 systems collectively, .71% of inmates (8,680 of 1.22 million) engaged in self-injurious behavior. Rates of self-injury did not differ significantly between states that distinguish self-injurious behavior from presumed suicidal behavior and those that do not. No significant relationship between fiscal expenditures and self-injury events was observed. However, although the design capacity of systems was also not related to prevalence of self-injurious behavior, there was a nonsignificant trend that operational capacity was positively correlated with rates of self-injurious behavior.
Frequency and nature of self-injury incidents
Although it appears that in the average prison system less than 2% of inmates per year in 2008 engaged in self-injurious behavior, these events occurred fairly frequently. Only five of 34 systems (15%) reported that self-injury occurred less than once a month. The remaining 29 systems (85%) reported that such events occurred at least once a week, with frequencies of several times per week, once per day, and more than once per day reported by 17 (50%), two (6%), and five (15%) systems, respectively.
Most of the 31 systems that responded to this item reported that inmates needed medical treatment outside of the prison facility after self-injurious behavior events either less than 5% of the time (N=12, 39%) or 5%–10% of the time (N=7, 23%). Only one system reported a need for outside medical treatment more than 50% of the time.
Although most self-injurious behaviors did not require outside treatment, they were disruptive to facility operations at least “minimally” in seven systems (18%) and “somewhat” in an additional 13 (34%). The remaining half (N=18, 47%) described these events as “moderately” (N=11, 29%) or “extremely” (N=7, 18%) disruptive. Most systems also reported these incidents as either moderately (N=16, 43%) or extremely (N=10, 27%) significant on consumption of mental health services or resources. Only three (8%) described self-injury events as just minimally affecting mental health services and resources.
Two-thirds of systems (N=24, 63%) handle incidents of self-injurious behavior as rule infractions. Both mental health and custodial staff are responsible for dealing with these incidents in more than half of the systems (N=23, 59%), with mental health staff alone being primarily responsible in the remaining 16 (41%). Mental health and custodial staff are “somewhat collaborative” (N=12, 31%) or “mostly collaborative” (N=26, 67%) with each other when there is a self-injury incident, although one system reported a “somewhat conflictive” relationship. Degree of collaboration did not correlate with which staff had primary responsibility for dealing with self-injurious behaviors.
Diagnoses of self-injurers and use of medications and restraints
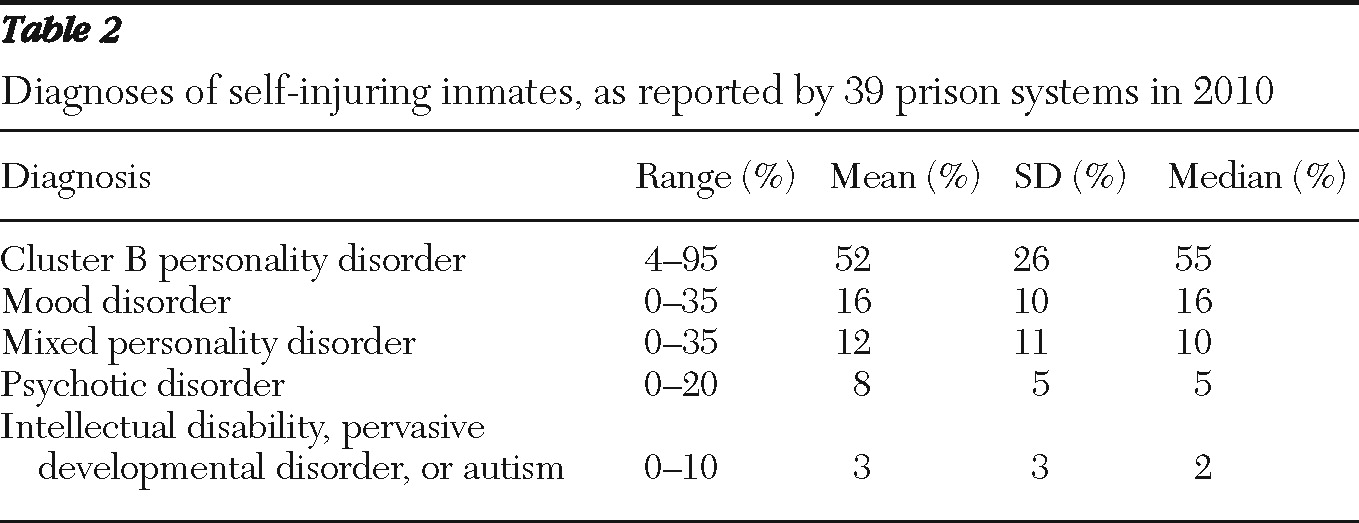
Responses indicated that most inmates who self-injure have one or more psychiatric diagnoses, with cluster B personality disorders most prevalent, followed by mood disorders, personality disorders presenting with features of more than one specific disorder, psychotic disorders, and intellectual disability, pervasive developmental disorder, and autism (
Table 2).
Segregation and other lockdown units, in which inmates are often confined to their cells for disciplinary reasons for 23 hours a day and routinely come out only for showers and solitary exercise, had the highest rate of occurrence of self-injurious behaviors in most systems (N=22 of 29, 76%). Among general population units, self-injury incidents occurred more often in maximum-security settings, which typically provide heightened supervision and restrictions. Twice as many systems (N=11 of 23, 48%) reported that maximum-security units had either the first or second highest rates of self-injury, and only six of 26 respondents (23%) reported that nonmaximum settings had the first or second highest rates of self-injury.
No system used the surveyed classes of medications (that is, antipsychotics, anticonvulsants, naltrexone, selective serotonin reuptake inhibitors [SSRIs], anxiolytics, and beta blockers) “all of the time” to treat inmates who engage in self-injurious behavior. Although the questionnaire asked about the use of medications in the management of self-injurious behavior, several respondents commented that medications are used only to treat underlying psychiatric disorders. SSRIs, beta blockers, antipsychotics, and anticonvulsants were reportedly used “most of the time” by eight (36%), one (5%), one (5%), and one (4%) system, respectively. Antipsychotics, anticonvulsants, and SSRIs are mainly used “sometimes” by 17 (74%), 12 (57%), and 11 (50%) systems that provided data on this portion of the survey, respectively, and anxiolytics and beta blockers were used only “infrequently” or “never” by 16 (76%) and 12 (62%) systems, respectively. Naltrexone was reported as “never” used by 12 (55%) respondents.
Nearly all responding systems (N=33 of 35, 94%) have policies and procedures for the use of medications without the inmate's consent. Most systems (N=33 of 39, 85%) use involuntary medications, but most that do (N=20 of 29 respondents, 69%) use them for nonemergencies on the basis of substituted decision making (for example, court order) less than 5% of the time. Systems reported that they enforce use of medication in emergencies infrequently, with most reporting use less than 5% of the time (N=17 of 31, 55%), followed by 5%–25% of the time (N=5, 16%) and 26%–50% of the time (N=3, 10%). The remaining five respondents on this item (16%) never use emergency, involuntary medications.
Many systems reported using restraints for managing episodes of self-injurious behavior, and all of them have related policies and procedures for doing so. Just over one in ten systems (N=4 of 31, 13%) and one in five (N=6 of 30, 20%) systems reported that they never use security-ordered or mental health-ordered restraints, respectively. Few systems reported that they use them nearly all of the time (76%–99% of the time), with three (10%) systems using security-ordered restraints and two (7%) systems using mental health-ordered restraints. The most prevalent frequency of restraint use reported was less than 5% of the time for both security-ordered restraints (N=14, 45%) and mental health-ordered restraints (N=14, 47%). We found no association between use of restraints and fiscal expenditures or census as a percentage of either design or operational capacity, with the exception of borderline statistical significance between mental health-ordered restraints and the system's operational capacity.
Among management strategies, individual behavior management plans had the greatest variability. Some systems use them infrequently: six (17%) less than 5% of the time and ten (29%) 5%–25% of the time. Others use them very frequently: six (17%) 76%–99% of the time and six (20%) all of the time. Behavioral management programs or units, with bed sizes ranging from 15 to 630 beds (mean±SD=136.4±182.1, median=52), exist in 18 systems (49%). Nearly an equal number of systems use behavioral reinforcements never or less than 5% of the time (N=7, 22%) or 76%–99% of the time or all of the time (N=8, 25%). The most prevalent frequency for use of behavioral reinforcements was 5%–25% of the time (N=9, 28%).
Finally, as a measure of the perceived importance of self-injurious behavior, 31 of 37 respondents (84%) indicated a willingness to participate in future empirical studies on its epidemiology or management, and 34 (92%) voluntarily provided direct contact information.
Discussion
This study is the first survey of statewide directors of prison mental health services regarding the national prevalence, impact, and management of self-injurious behavior by inmates. The high response rate attests to the perceived importance of this issue as a problem facing the U.S. prison system. All regions of the country participated, including states with inmate populations of all sizes, which adds to the strength of our findings. The lack of a widely and consistently used definition of self-injurious behavior has complicated research in this area, and our findings demonstrate several important definitional differences among states, including on criteria such as overt actions, intent, and need for medical treatment. Although most systems attempt to distinguish between self-injurious behavior and suicide attempts, others include presumed suicide attempts in their definition of self-injurious behavior.
Over the past 20 years, attempts have been made to distinguish between self-injurious behavior with and without suicidal intent in correctional settings (
4,
18,
30–
35). Many behaviors have clear and explicit intent to inflict limited self-harm, typically superficial cutting or burning, as a coping or negotiating mechanism (
4,
31,
32,
35). Other behaviors have the clear intent to end one's own life (
33,
34). Some people engage in both behaviors at different times (
30,
31). Effective management requires an assessment of each event, an understanding of the motive, and a treatment plan based on clinical diagnosis and current mental status of the inmate (
3,
31). This kind of management is complicated by the fact that even if there is no intent to commit suicide, mistakes happen and people intent on modest self-injury nevertheless die. Further, those with a history either of self-injurious behavior or of suicide attempts have an elevated risk of both in the future (
34). Although treatment plans should be put in place, each event must be assessed appropriately and independently of the inmate's history because motivation and context change over time. There is no simple solution. All inmates who engage in self-injurious behavior pose a risk of lethality regardless of their motivations, and they all require clinical assessment and appropriate interventions.
A relatively small proportion of inmates are responsible for frequent episodes of self-injury. On average, just over 1% of inmates per year engage in self-injurious behavior. However, most systems experience these events at least once per week, in half of all systems they occur several times per week, and in another 21% they occur either once a day or more than once a day. Any incident, however, can seriously compromise safety and adversely affect services and budgets. In addition to sometimes severe injury to the inmate, harm can be done to other inmates and to correctional staff when intervening or through exposure to body fluids. Serious incidents require a freeze in normal facility operations. Injuries that need outside medical attention create additional security risks, including potential escape attempts. The interruption of normal operations, diversion of custodial staff, need for mental health and medical assessments, frequent transfers to infirmary or crisis cell settings, need for special monitoring, and cost of outside care all deplete resources and have substantial fiscal consequences. Responses to the survey indicate that these behaviors frequently result in moderate to extreme disruptions of custodial and mental health operations.
The high rate of occurrence of self-injurious behavior in segregation and other lockdown units is also noteworthy. It is important to determine whether these units cause or contribute to these events or whether their inmate population merely has a higher prevalence of risk factors, such as other aggressive behaviors or mental illness, associated with self-injury.
We also found that management approaches for self-injurious behavior lack widespread consistency. Although there is considerable variability, interventions such as restraints, medications, and behavior management plans and programs tend not to be used in most instances. When self-injurious behavior is a symptom of an axis I diagnosis, treatment should target the disorder and may require housing in a special needs unit. More commonly, however, self-injury is associated only with a personality disorder.
Some correctional systems provide minimal, if any, treatment to inmates with behavioral problems associated with personality disorders. Self-injury is often a maladaptive form of communication or an attempt to achieve an outcome that may be covert or overt. Staff frequently view such inmates as manipulating the system, but this perceived or actual manipulation should be addressed in treatment and not be seen as a contraindication for treatment. The finding that two-thirds (N=24, 63%) of systems handle self-injurious behavior events as a rule infraction is consistent with a “correctional” approach in contrast to a treatment response. We recommend that inmates with these behaviors qualify for mental health services.
Many of these inmates, however, are housed in lockdown units or maximum-security units that are not built with treatment programming space in mind. Self-injury is often just one of several types of maladaptive and frequently dangerous behaviors related to the high-security status of these inmates. Thus there are obstacles to providing these inmates adequate treatment in a confidential and safe manner.
Several correctional health care systems have attempted treatment in behavioral management units. In the experience of one of the authors (JM), these programs often fail because they are designed and run by custodial staff, with inadequate involvement of mental health staff. Custody rules, regulations, and practices can also make it difficult to provide effective positive reinforcements, such as suspension of disciplinary lockdown time, increased out-of-cell time, congregate recreation time, or loaner TVs. More recently, some systems have begun to establish behavioral management units that address these shortcomings. Similar programs, as well as innovative therapeutic communities in which violent inmates with personality disorders participate in frequent community meetings and play an active role in group decision making, have met with success in other countries, although one or two years of treatment may be needed before significant improvements occur (
36,
37).
Our study has some limitations. Although statewide correctional mental health directors have considerable knowledge of the areas covered in this survey, the general absence of tracked data makes their responses mostly impressionistic, and the lack of a consistent definition of self-injurious behavior means that each director may have been measuring different phenomena. Directors also might have skewed their responses in a more socially desirable direction despite assurances that data would be reported only in aggregate.
Our high and representative response rate suggests an absence of regional or system-size bias in our findings, but given the still small number of systems, our study may have been underpowered to find some correlations and differences. For example, if relationships exist between measures of crowding or funding levels and the rate of self-injurious behavior and use of restraints, our study may have had too small a sample to have identified them.
Conclusions
Self-injurious behavior by correctional inmates can have serious health, safety, operational, security, and fiscal consequences. A relatively small number of inmates account for frequent events. Despite the problems associated with self-injurious behavior, relatively little is known about its epidemiology or about effective interventions. The wide difference in how systems manage these incidents and the inmates who engage in them suggests a lack of best-practice models. The response rate to this survey and nationwide participation by prison systems from all regions of the country and of all sizes indicates the perceived importance of self-injurious behavior to the statewide directors of mental health in our nation's prisons. The large percentage of systems willing to participate in future discussions and research on this topic underscores that interest, along with the need for greater understanding of the root causes of this behavior and best ways to manage it.
Acknowledgments and disclosures
The authors thank the Office of Survey Research staff at the Center for Health Policy and Research and Elizabeth O'Connell, M.S., for their assistance with identification of study participants, fielding the survey, and tracking participant responses.
The authors report no competing interests.