Epidemiological studies have shown higher prevalence rates of alcohol and drug disorders among some sexual minority populations (
1–
7). Similarly, the prevalence of some commonly occurring mental disorders appears to be elevated among persons from sexual minority groups (
3,
8,
9). However, it is not clear whether these groups also have higher rates of treatment seeking for common mental disorders than heterosexuals. Prior research has shown that lesbian and bisexual women have higher rates of help seeking for alcohol problems than heterosexual women, even among those with lower levels of alcohol-related problems (
4,
10,
11). Similarly, some studies have shown that lesbians tend to utilize mental health services at higher rates than heterosexual women (
12).
Cochran and Mays (
13) found that men and women who reported same-gender sex partners were more likely than their respective counterparts to have sought mental health or substance abuse services in the past year. However, a study of gay men in Geneva showed that nearly half of those with a psychiatric disorder (including substance use disorders) had never sought treatment, which is comparable to rates found in other general population studies (
14). In contrast, studies of persons receiving substance abuse treatment have found more severe substance use problems and higher rates of psychiatric treatment among persons from sexual minority groups than among heterosexuals (
15). But clinical studies using targeted subgroups, such as gay men who use methamphetamine, have suggested that levels of psychopathology are elevated in these subgroups compared with population-based samples of persons from sexual minority groups (
16,
17).
There is disagreement about the factors that prompt individuals to seek treatment for psychiatric disorders (
18). Several national surveys have found a lack of concordance between the presence of a psychiatric disorder and the receipt of treatment services (
19,
20). Most individuals with these disorders neither receive treatment for them nor perceive a need for it (
21,
22). Individuals most commonly state that they can manage these problems on their own (
23) or are “not ready” to stop using substances (
24). Moreover, national epidemiological surveys have demonstrated that some individuals who do not have a diagnosable disorder seek treatment (
25) or perceive a need for it (
26), especially when they have high levels of psychological distress or impairments in functioning (
27–
29).
The goal of the study reported here was to examine the effects of sexual orientation on perceived need for treatment for mental and substance use disorders and unmet need for treatment, taking into consideration whether this relationship is differentially influenced by gender and by the presence of a diagnosed disorder. Because of previous research that showed more treatment seeking among persons from sexual minority groups and higher rates of health services utilization among women (
30), we hypothesized that persons from sexual minority groups, particularly women, would be more likely than heterosexuals both to perceive a need for treatment and to receive it. Thus we predicted that persons from sexual minority groups would have overall lower levels of unmet need for treatment, after analyses controlled for other sociodemographic characteristics that might be independently associated with treatment access and utilization.
Methods
Study design and sample
Data for this study were from the 2004–2005 California Quality of Life Survey (Cal-QOL) (
31), which is a follow-back to the 2003 California Health Interview Survey (CHIS). The parent CHIS is a stratified, multistage, random-digit telephone health surveillance interview of more than 42,000 adults aged 18 and older that has been conducted every other year since 2001. Information collected covers a wide range of topics, including health status, health conditions, health-related behaviors, health insurance coverage, and access to and use of health care services.
The Cal-QOL follow-back survey used a subsample of the original CHIS survey sample to obtain more detailed information about specific topics (in this case, sexual orientation). The overall CHIS response rate was 34% according to the response rate 4 method of the American Association for Public Opinion Research (
32), which is consistent with other recent random-digit telephone interviews. In the CHIS, all adult respondents aged 18 to 70 were asked about the gender of their sexual partners during the past year, and those aged 18 and older (with no age limit) were asked about their sexual orientation identity. Seventy-six percent of respondents were willing to participate in additional health surveys. From the CHIS sample, 4,165 individuals were selected by probability methods. Eligible individuals had completed a CHIS interview in either English or Spanish and were willing to be recontacted. The sampling method overselected for sexual minority status. Of the 4,165 individuals, 2,322 were successfully interviewed between October 2004 and February 2005 (56% response rate according to the response rate 1 method of the American Association for Public Opinion Research [
32]). Detailed information about Cal-QOL methods is available elsewhere (
31,
33).
This study received institutional review board approval from the University of California, Los Angeles, and Westat (the survey subcontractor).
The study reported here used data from 2,079 (unweighted) individuals aged 18 to 64 at the time of the CHIS interview; those who were likely eligible for Medicare were excluded, as were individuals with missing data on the diagnostic variables. Overall, the weighted sample was about equally divided between men (48.5%) and women (51.5%).
Measures
Treatment-related measures.
Need for treatment was assessed by two questions: “In the past 12 months, did you think you needed help for alcohol or other drug problems?” and “In the past 12 months, did you think you needed help for emotional or mental health problems, such as feeling sad, blue, anxious, or nervous?” A positive response to either question was coded to indicate a perceived need for treatment.
Treatment received was assessed by several questions. The first asked whether the respondent had “received any treatment for emotional, mental health, alcohol, or other drug problems” in the past 12 months. Subsequent questions referred to treatment received for a mental or substance use disorder in specific venues, including hospitalization, residential substance abuse treatment, emergency department, a mental health provider or substance abuse specialist (that is, a psychiatrist, psychologist, social worker, psychiatric nurse, or counselor), a self-help group, alternative medicine, and a nonresidential alcohol or other drug treatment program.
Unmet need for treatment was derived by coding as “yes” all those who perceived a need for treatment in the past 12 months but who did not receive any during that time and coding as “no” all others who perceived a need for treatment and who had received it.
Presence of a disorder.
Diagnoses were derived by using the Composite International Diagnostic Interview-Short Form (CIDI-SF) (
34). The CIDI-SF, administered by trained lay interviewers, provides screening assessments of community samples for common mental disorders. Studies have found moderate agreement between CIDI-SF diagnoses and those obtained by face-to-face diagnostic clinical interviews on the basis of
DSM-III-R criteria (
35,
36). Probable diagnoses were obtained for past-year major depression, generalized anxiety disorder, and panic disorder on the basis of these criteria (
37).
Two additional CIDI-SF modules assessed past-year symptoms of drug and alcohol dependence. All respondents who indicated any use of illicit drugs or nonprescribed medications in the previous 12 months were administered the drug module, which assesses seven symptoms from six of the core symptom areas of substance dependence: using in larger amounts or for longer periods than intended, being under the influence or recovering from use while engaged in social obligations, experiencing emotional or physical problems from use, having an irresistible urge to use, spending a great deal of time using or getting over using, and developing tolerance. Those reporting three or more of the seven symptoms received a positive diagnosis for past-year probable drug dependence disorder consistent with modified
DSM-IV criteria (
38). Seven similar questions were asked about alcohol use, with the addition of an item on alcohol-related withdrawal symptoms. A diagnosis of past-year probable alcohol dependence disorder was made if the respondent reported symptoms in three or more of the seven core areas consistent with
DSM-IV criteria. This diagnostic screening method was shown to have excellent reliability and validity in identifying individuals with substance use disorders in the National Comorbidity Survey (
39).
For descriptive purposes, disorders were classified into two non-mutually exclusive groups: mood or anxiety disorders (21.7% of the weighted sample) and alcohol or drug use disorders (7.1% of the weighted sample). A composite variable indicating presence of any disorder versus no disorder was used in the multivariate analyses described below.
Sexual orientation.
Sexual orientation was determined by information obtained about behavioral history and self-identification. Behavioral questions asked about the gender of sexual partners since age 18 and during the past year. Individuals were also asked their sexual orientation identity. Respondents were classified into one of four categories. In the first category were lesbian, gay, or bisexual women or women with homosexual experience, hereafter referred to as “lesbian and bisexual women” (13.8% of the unweighted sample and 5.2% of weighted sample). In the second group were gay or bisexual men or men with homosexual experience, hereafter referred to as “gay and bisexual men” (15.3% of the unweighted and 7.0% of the weighted samples). The third group included exclusively heterosexual women (37.7% of the unweighted and 46.2% of the weighted samples), and the fourth included exclusively heterosexual men (33.1% of the unweighted and 41.6% of the weighted samples).
Statistical analyses
Data were analyzed with SAS, version 9.1.3. We applied sample weighting to adjust for selection probability, nonresponse, and poststratification to generate estimates representative of the California population. We first used chi square tests to investigate rates of past-year treatment need, treatment received, and unmet need by groups classified by gender, sexual orientation, and presence of a disorder. When cell sizes were less than five, Monte Carlo estimates of exact tests were used to assess their significance. Second, to test the hypothesis about the relationship of gender, disorder, and sexual orientation status with treatment use, we modeled unmet need for treatment in the past year as a dependent variable in logistic regressions. Age, race-ethnicity (white versus other), and education level (some college versus none) were entered as covariates. Interaction effects were examined by the specified-levels approach, which can be used when the modifier has two levels (
40). This approach omits the predictor from the model and includes the modifier and two product terms—that is, the product of the predictor with each level of the modifier. The coefficients estimated for these two product terms can then be interpreted as the effect of the predictor for each level of the modifier.
Odds ratios (ORs) and 95% Wald confidence intervals (CIs) are presented. Statistical significance was set at .05. The logistic regression models presented all had acceptable fit, as indicated by the Hosmer-Lemeshow goodness-of-fit statistic (
41).
Results
Sample characteristics
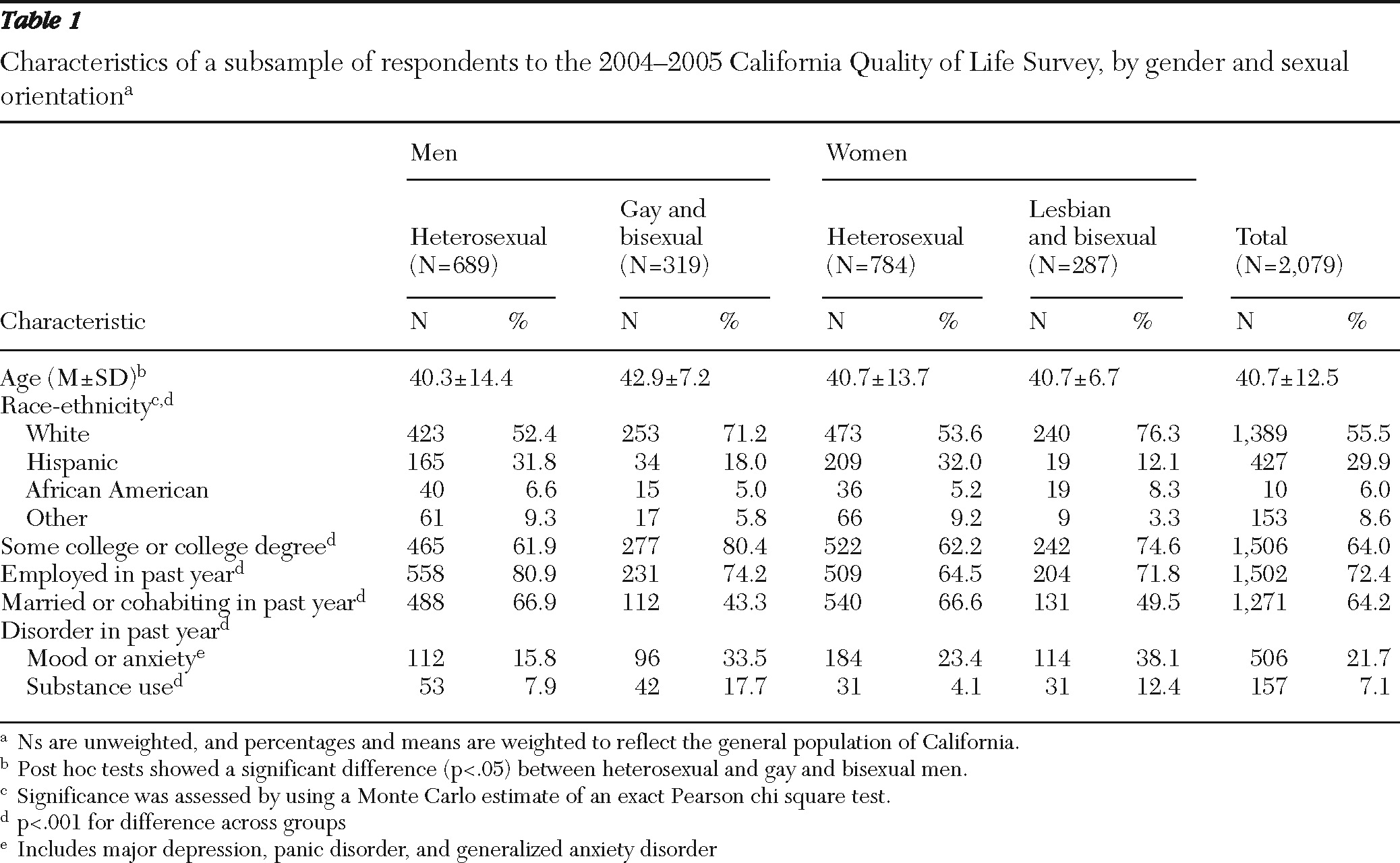
As shown in
Table 1, the racial-ethnic distribution was approximately 56% white, 30% Hispanic, 6% African American, and 9% other racial-ethnic groups (Asian-Pacific Islander or Native American). The mean age was 40.7 years. Most respondents (72%) were currently employed and 81% (unweighted N=1,773) had health insurance (including both public and private insurers). Sixty-four percent had at least some college education. Approximately two-thirds (64%) were currently married or cohabiting with a partner.
Differences among sexual orientation groups
Overall, respondents from sexual minority groups reported higher rates of mental and substance use disorders (
Table 1). Lesbian and bisexual women had the highest prevalence of mood and anxiety disorders (38.1%), followed by gay and bisexual men (33.5%), heterosexual women (23.4%), and heterosexual men (15.8%). Gay and bisexual men had the highest prevalence of substance use disorders (17.7%), followed by lesbian and bisexual women (12.4%), heterosexual men (7.9%), and heterosexual women (4.1%).
Significant differences were found among the groups in age, race-ethnicity, education, employment status, and being married or cohabiting. In general, compared with the heterosexual groups, the sexual minority groups had a significantly higher proportion of whites and lower proportions of Hispanics and respondents in the “other” category, a higher level of education, and a lower proportion of married or cohabitating respondents. Gay and bisexual men were also significantly older than heterosexual men. Regardless of sexual orientation, a greater proportion of men than women were employed in the past year.
Treatment status by disorder, gender, and sexual orientation
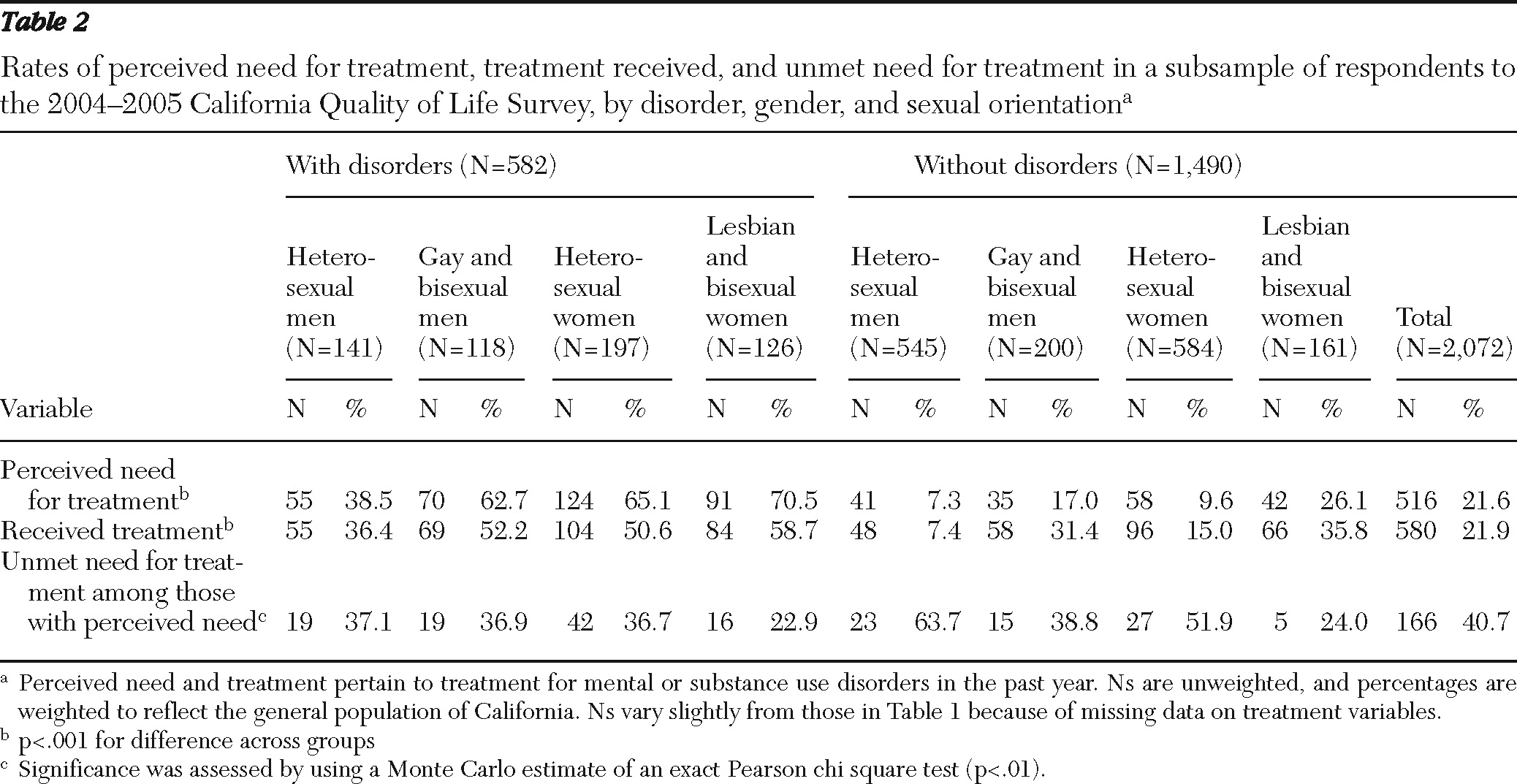
The three treatment-related outcomes were examined by gender, sexual minority status, and disorder status (
Table 2). As expected, a greater proportion of respondents with mental or substance use disorders than those without such disorders perceived a need for treatment. Among those with at least one disorder, lesbian and bisexual women had the highest proportion reporting perceived need for treatment (70.5%), followed by heterosexual women (65.1%), gay and bisexual men (62.7%), and heterosexual men (38.5%). Similarly, among those without any disorder, lesbian and bisexual women had the highest proportion reporting perceived need for treatment (26.1%), followed by gay and bisexual men (17.0%), heterosexual women (9.6%), and heterosexual men (7.3%).
Overall, about 22% of the sample reported having received some form of treatment for a mental health or substance use problem in the past year. A greater proportion of respondents with disorders than those without disorders reported having received treatment. Lesbians and bisexual women had the highest rates of treatment participation regardless of disorder status; heterosexual men had the lowest rates of treatment among those with and those without disorders.
About 41% of respondents who perceived a need for treatment met the criterion for unmet need. Unmet need was highest among heterosexual men and women without disorders and lowest among lesbian and bisexual women regardless of disorder status. About 40% of gay and bisexual men regardless of disorder status had an unmet need for treatment.
Logistic regression models of unmet need for treatment
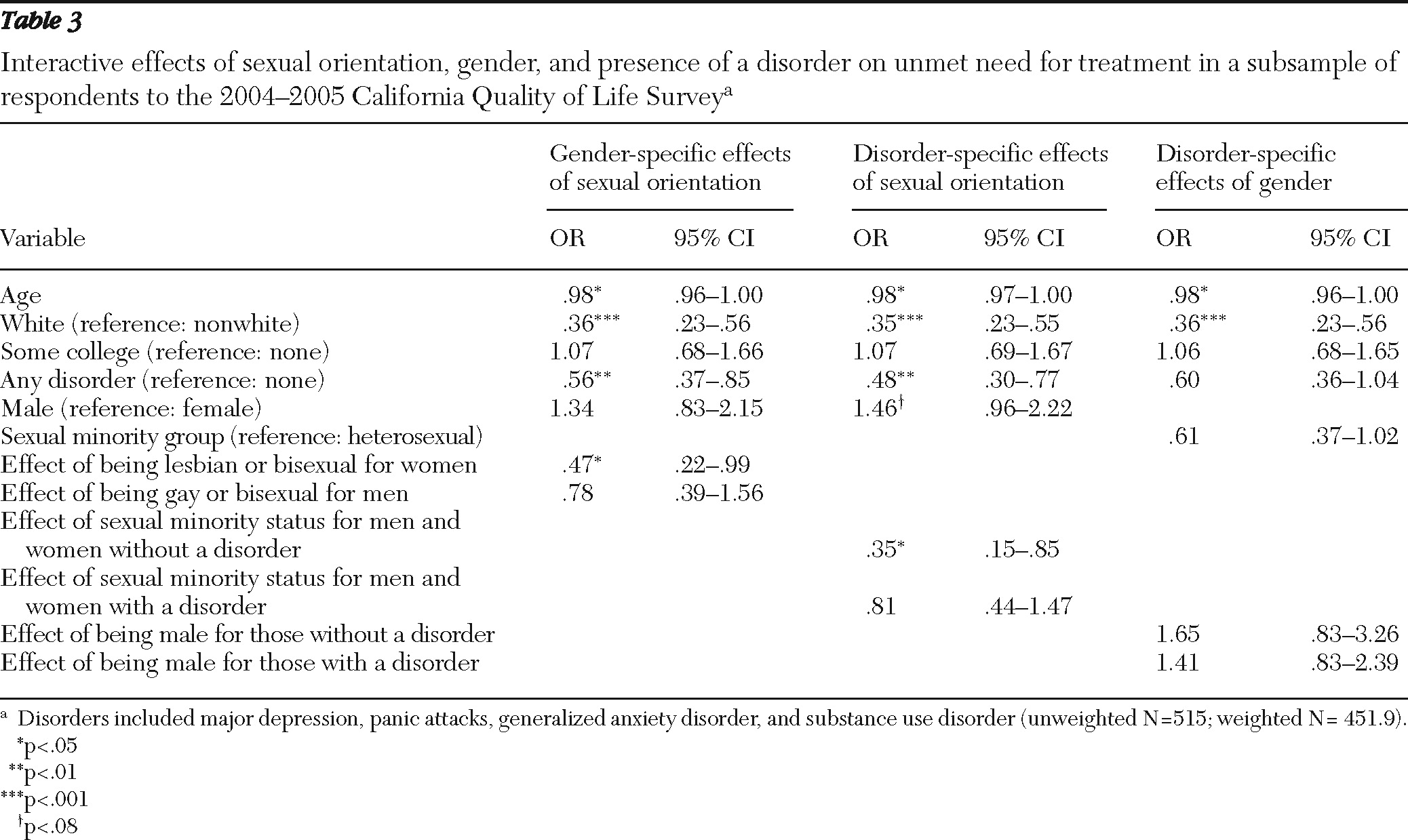
Unmet need for treatment was modeled in a logistic regression in which interactions among disorder status, gender, and sexual orientation were examined. All models were adjusted for the effects of age, race-ethnicity (white versus nonwhite), and education level (some college or none).
Using the specified-levels approach, we examined the effect of sexual orientation within gender categories and the effects of sexual orientation and gender within disorder categories (
Table 3). The results indicated that lesbian and bisexual women were about half as likely as heterosexual women to have unmet need for treatment (OR=.47). However, no significant effects of sexual orientation on unmet need for treatment were found for men. Among respondents with no disorder, those from sexual minority groups were about a third as likely to have unmet need for treatment (OR=.35). No significant interaction effect of gender and disorder status on unmet need for treatment was found.
We also estimated this model without interaction terms in order to examine the main effects of gender, sexual orientation, and presence of a disorder (data not shown). Findings indicated that compared with women, men had higher odds of having unmet need (OR=1.69, CI=1.10–2.58, p<.05) and that respondents with a disorder had lower odds of having unmet need than those without a disorder (OR=.57, CI=.37–.87, p<.05). However, there was no significant main effect of sexual orientation on unmet treatment need. Also, consistent with prior research (
42), older individuals and whites had significantly lower odds of having unmet need for treatment than younger and nonwhite respondents, respectively.
Discussion
This study extends prior research on the effects of sexual orientation on the prevalence of substance use and mental disorders to examine the relationship of prevalence with perceived need for and receipt of treatment services. Consistent with prior research, the study findings indicate that individuals from sexual minority groups had higher prevalence rates of several disorders compared with rates among heterosexual men and women. In addition, persons from sexual minority groups had higher levels of perceived need for treatment and higher rates of treatment utilization and therefore were least likely to have unmet need for treatment. However, when the analyses adjusted for sociodemographic variables, such as race-ethnicity and education, the main effect of sexual orientation on unmet need was no longer significant. The effect of sexual minority status was evident, however, in its interactions with gender and disorder status. Lesbian and bisexual women were significantly less likely than heterosexual women to have unmet treatment need, although among men no difference in unmet need was found by sexual orientation. Sexual minority status was also significantly associated with unmet need for treatment among those without a diagnosed disorder, but the association was not significant among those with a disorder.
These findings suggest that sexual minority status may promote help seeking for psychiatric disorders (
43,
44) but that its effect is moderated by gender. This finding is similar to results of a recent study that used national survey data and showed that the effects of sexual minority status on substance use and dependence were larger for women than men (
45). Moreover, in the study reported here, the effect of sexual minority status was most apparent among women without a mental or substance use disorder.
The findings from this population-based study suggest that diagnostic criteria may be less relevant in determining perceived treatment need and treatment use among sexual minority populations. This finding deserves more exploration in regard to factors that may lead persons in sexual minority groups to seek care (such as placing a greater value on therapeutic services and having higher perceived stress that does not reach diagnostic thresholds), particularly in the face of the limited availability of services tailored for these groups and barriers to providing these services (
46–
48).
This study encountered limitations typical of telephone-based follow-back surveys. Although the Cal-QOL follow-back survey oversampled for sexual minority status, the weighted sizes of sexual minority groups were relatively small. Statistical power may have been limited in determining significance for some relationships because of the small sizes of some subgroups. Although data were obtained for the most prevalent mental disorders among population-based samples (
49), namely mood and anxiety disorders, it is possible that those who were classified as “without disorders” had other mental disorders that were not included in the Cal-QOL assessment, leading to their misclassification. Including variables on sexual orientation and sexual behavior in larger-scale national probability studies of mental health and substance use problems would provide important opportunities to investigate the robustness of our findings.
Conclusions
This study provided evidence that perceptions of need for treatment for either a mental or substance use disorder are highly influenced by sexual orientation and that treatment use is further influenced by both gender and sexual orientation. Moreover, the influence of gender and sexual orientation was more pronounced among those who did not meet diagnostic criteria for either type of disorder but who nonetheless perceived a need for treatment. This suggests that the relationship of diagnostic criteria to determinations of treatment need among individuals from sexual minority groups should be reevaluated in order to better understand and more fully address the factors that influence treatment seeking among those who perceive a need for care.
Acknowledgments and disclosures
Financial support for this work was provided by grants DA-15539 and DA-20826 from the National Institute on Drug Abuse and grant MD-000508 from the National Center for Minority Health and Health Disparities. The authors thank staff of the California Health Interview Survey for their assistance in making the Cal-QOL survey possible.
The authors report no competing interests.