The therapeutic relationship between patient and clinician is essential to the practice of psychiatry. Although the term was first used in psychotherapy, the concept of the therapeutic alliance and its role in engaging patients in psychiatric treatment are now well recognized (
1–
5). In the literature, the therapeutic relationship is broadly defined as the relationship between the patient and any clinician involved in the patient's care. It can reflect relationships that “last for seconds or decades” and can have positive or negative effects on treatment outcome (
4,
5). Patients have identified the therapeutic relationship as the most crucial factor for good psychiatric care (
6) and for the establishment of a “safe and therapeutic milieu” during treatment (
7). The use of coercion in psychiatry has been hypothesized to undermine this therapeutic relationship between patient and clinician (
7–
9).
Psychiatry is one of the few areas of medical practice where the use of coercion is legally and ethically sanctioned under limited conditions (
10,
11). This remains one of the most controversial issues in mental health care policy (
9,
12–
15). Some argue that legally mandated treatment is beneficial because it helps to alleviate illness and restore an individual's ability to make autonomous decisions (
16). Others believe that individuals subjected to coercion may not engage in treatment and may avoid future contact with mental health services for fear of being subjected to involuntary care again (
17). A qualitative study of patients' experiences during psychiatric hospitalization by Gilburt and colleagues (
7) concluded that “coercion was always experienced negatively and had a negative impact on relationships” between patients and staff.
The lack of a standard definition of coercion in psychiatric care has hampered the investigation of its impact on psychiatric care. The primary issue is how to operationalize and measure the experience of coercion. Some studies use legal status at admission, either voluntary or involuntary, as a proxy for experience of coercion (
18–
20). However, more recent research has determined that legal status is a poor measure of patient experience (
21–
24) and that coercion is not necessarily a function of the legislation that mandates treatment but of the relationship with those who enforce that legislation (
7).
The incongruence between legal status and experience of coercion led to the development of a subjective measure of perceived coercion, the MacArthur Perceived Coercion Scale, which assesses patients' beliefs about the influence, freedom, control, or choice they had in the decision to enter treatment (
8,
23,
25). Research using this measure indicates that patients' “experiences of coercion are largely shaped by their social experiences in the process of treatment entry” (
9).
Despite the hypothesized association between the therapeutic relationship and the experience of coercion, this is the first study to our knowledge to quantitatively examine this association. The study was conducted in England, where psychiatric care is provided to patients in small geographical catchment areas by a dedicated multidisciplinary team. When hospitalization is required, this team usually organizes the admission and remains responsible for the patient while he or she is hospitalized. The Mental Health Act, used in involuntary admission, also promotes the involvement of psychiatrists with prior knowledge of the patient.
In this study, we interviewed a consecutive sample of patients admitted to a psychiatric hospital and investigated the association between the therapeutic relationship and perceived coercion. Taking a patient-centered approach, we used validated subjective scales to measure patient experiences of both the therapeutic relationship and perceived coercion.
Methods
We conducted a cross-sectional cohort study of perceived coercion in a consecutive sample of admissions to five acute adult wards at two psychiatric hospitals in Oxford, England. Ethics approval was granted by the Mid and South Buckinghamshire Research Ethics Committee.
Sample
All patients admitted between January and May 2005 and August and December 2005 were assessed for inclusion in the study. Participants were interviewed only if they had been admitted to a participating ward within the previous seven days, and patients were excluded from the recruitment process if discharged within 24 hours of admission, insufficiently proficient in English to participate in an interview, or deemed by ward staff to be too ill or dangerous to take part. Ward staff introduced the researcher, who was independent of their care team, to eligible patients. After receiving a complete description of the study, interested patients provided their written informed consent. Patients were approached up to three times in the week after their admission but were interviewed only once, even if readmitted during the study period. Interviews took place on the ward in a location that was private and amenable to the patient (such as an examination room or bedroom). Interviews took between 30 and 60 minutes to complete.
Instruments
The interview schedule was designed to collect data on sociodemographic and clinical characteristics and on variables about the admission experience. Data collected during the interview were verified and supplemented by a review of case notes and computerized medical records. The following instruments were used.
The MacArthur Admission Experience Survey (AES) consists of 14 items that require a patient's true or false response to statements about being admitted to the hospital (
23). It has three subscales: perceived coercion (AES-PC, with five items; scores range from 0 to 5, with higher scores reflecting a high degree of perceived coercion), negative pressure (AES-NP, with six items; scores range from 0 to 6, with lower scores reflecting high levels of negative pressure) and procedural justice (AES-PJ, with three items; scores range from 0 to 3, with higher scores reflecting low levels of procedural justice). The scale has good internal consistency with respect to variation in site, instrument format, patient population, and interview procedure (
23).
The Helping Alliance Scale (HAS) is a therapeutic relationship measure that was modified for use in an inpatient setting (
3). It consists of five items examining the extent to which the patient feels understood by his or her clinician and how much the patient's treatment reflects mutually agreeable goals. The HAS has been found to be a simple, brief, and reliable measure of therapeutic alliance and is acceptable to patients with acute psychiatric illness (
26,
27). Patients were asked to name the clinician they felt was most responsible for their admission and to respond to the HAS items on the basis of their relationship with this individual.
The Global Assessment of Functioning (GAF), which takes into consideration the patient's psychological, social, and occupational functioning, was used to measure overall functioning on a continuum of mental health to mental illness (
28).
Statistical analysis
Data were analyzed with the Statistical Package for Social Sciences (SPSS 14.0). Descriptive statistical analyses were performed on baseline sociodemographic and clinical characteristics. The sample was divided into low (AES-PC score 0–2) and high (AES-PC score 3–5) perceived coercion groups by dichotomizing scores at the midpoint of the scale, as in previous studies (
23). Associations between perceived coercion level and sociodemographic and clinical characteristics were tested with t and Mann-Whitney tests for continuous variables and chi square tests for categorical variables.
Multiple-variable logistic regression analysis was also conducted to investigate the relationship between variables that were significantly associated with perceived coercion in the univariate analysis. Hierarchical logistic regression analyses were used to evaluate the relative contributions of sociodemographic and clinical characteristics and the therapeutic relationship to the prediction of perceived coercion level (
24,
29). The order of inclusion of variable blocks was based on previous studies of perceived coercion (
24,
29,
30).
Results
Recruitment
There were 342 admissions during the study period, of which 122 were ineligible: 46 patients were discharged or transferred shortly after admission, 34 were readmissions, 13 had insufficient proficiency in English for participation, 11 had originally been admitted to nonparticipating wards, 11 were too ill to provide informed consent, four had intellectual impairment, and three were too dangerous to approach.
Of the 220 eligible admissions, 217 were approached to take part (three were not contactable). Interviews were obtained from 164 (response rate 75%). Fifty patients refused to participate because they “did not feel like talking” or were “too tired,” and three agreed to take part but were unwilling to sign the consent form. Participating patients were asked to identify their admitting clinician and respond to statements included in the HAS with respect to this individual. Most patients identified the consultant psychiatrist (N=127, 77%) or junior psychiatrist working with their consultant (N=9, 5%). The other patients identified their psychiatric nurse (N=20, 12%), social worker (N=6, 4%), or general practitioner (N=2, 1%).
Sample characteristics
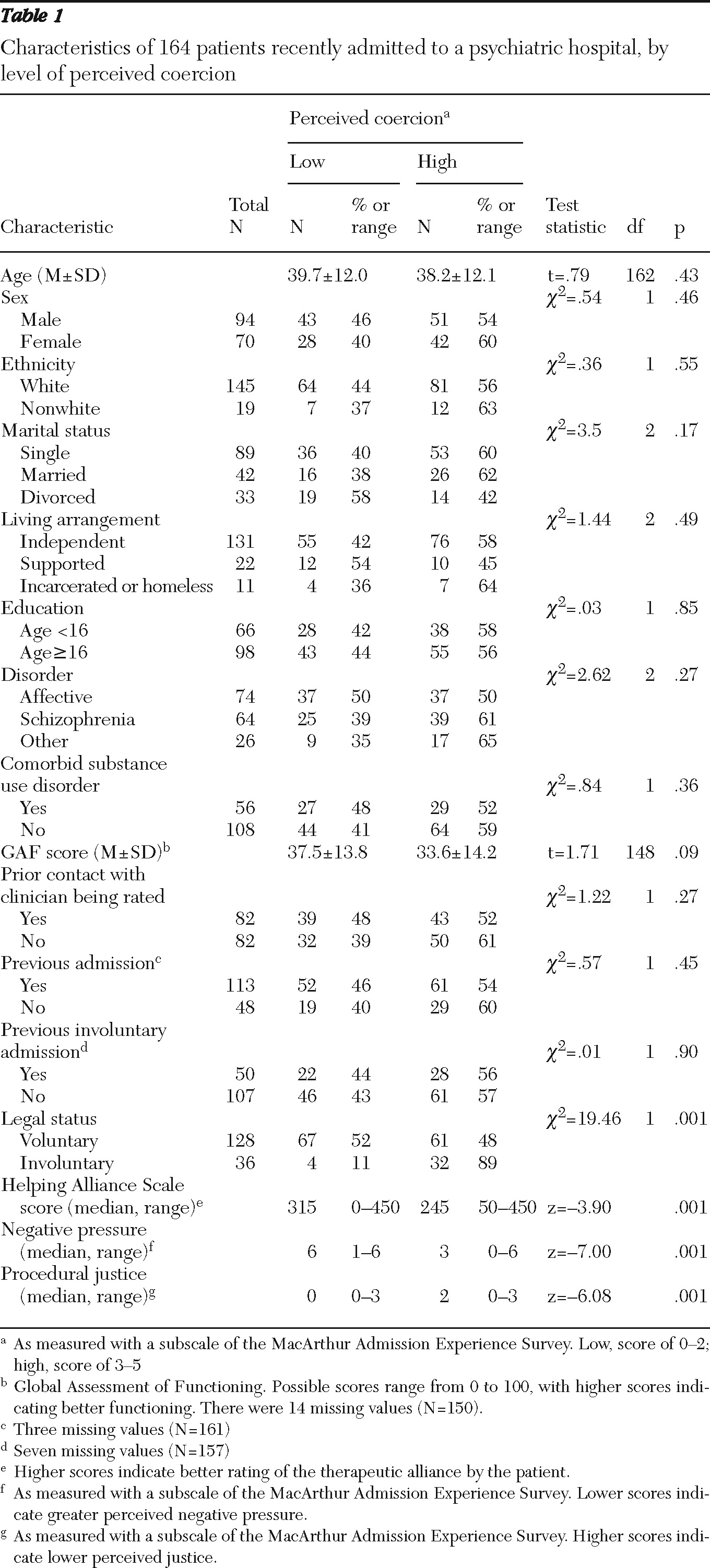
As shown in
Table 1, the sample was predominantly male (N=94, 57%), white (N=145, 88%), middle aged (mean±SD age 38.8±12.0 years), single (N=89, 54%) and living independently (N=131, 80%). Over half had completed at least basic secondary education, which in England is completed by age 16 (N=98, 60%). Almost half had an affective disorder (N=74, 45%), and approximately one-third had a co-occurring substance use disorder (N=56, 34%). The mean GAF score was 35.3±14.1. A total of 82 patients (50%) reported that they had previous contact with their admitting clinician. Most patients (N=113, 70%) had been previously admitted to the hospital, although less than one-third (N=50, 32%) had ever been detained under the Mental Health Act. Over three-quarters (N=128, 78%) were admitted to the hospital voluntarily, with 22% (N=36) admitted involuntarily under a section of the Mental Health Act.
Perceived coercion
McArthur AES-PC, AES-NP, and AES-PJ scores were calculated. The mean AES-PC score was 2.8±1.8, with a median of 3.0. The distribution was relatively even across the range of scores, although a majority experienced high levels of coercion. The mean AES-NP score was 4.3±2.0, with a median of 5.0. The distribution was negatively skewed; almost half of the patients (N=76, 46%) reported no negative pressure. The mean AES-PJ score was 1.1±1.1, with a median of 1.0. The distribution was positively skewed, with 66 (40%) patients experiencing the maximum AES-PJ score.
Associations with perceived coercion
There were no significant associations between any sociodemographic characteristics and perceived coercion level (
Table 1). Compared with patients who were voluntarily admitted (48%), a significantly higher proportion of involuntarily admitted patients (89%) reported high coercion (p<.001). HAS scores were significantly associated with level of perceived coercion (p<.001). Patients experiencing low levels of perceived coercion had higher ratings on the HAS therapeutic alliance scores (
Table 1). Low levels of coercion were significantly associated with less negative pressure (p<.001) and with higher ratings of procedural justice (p<.001) (
Table 1).
Logistic regression model of perceived coercion
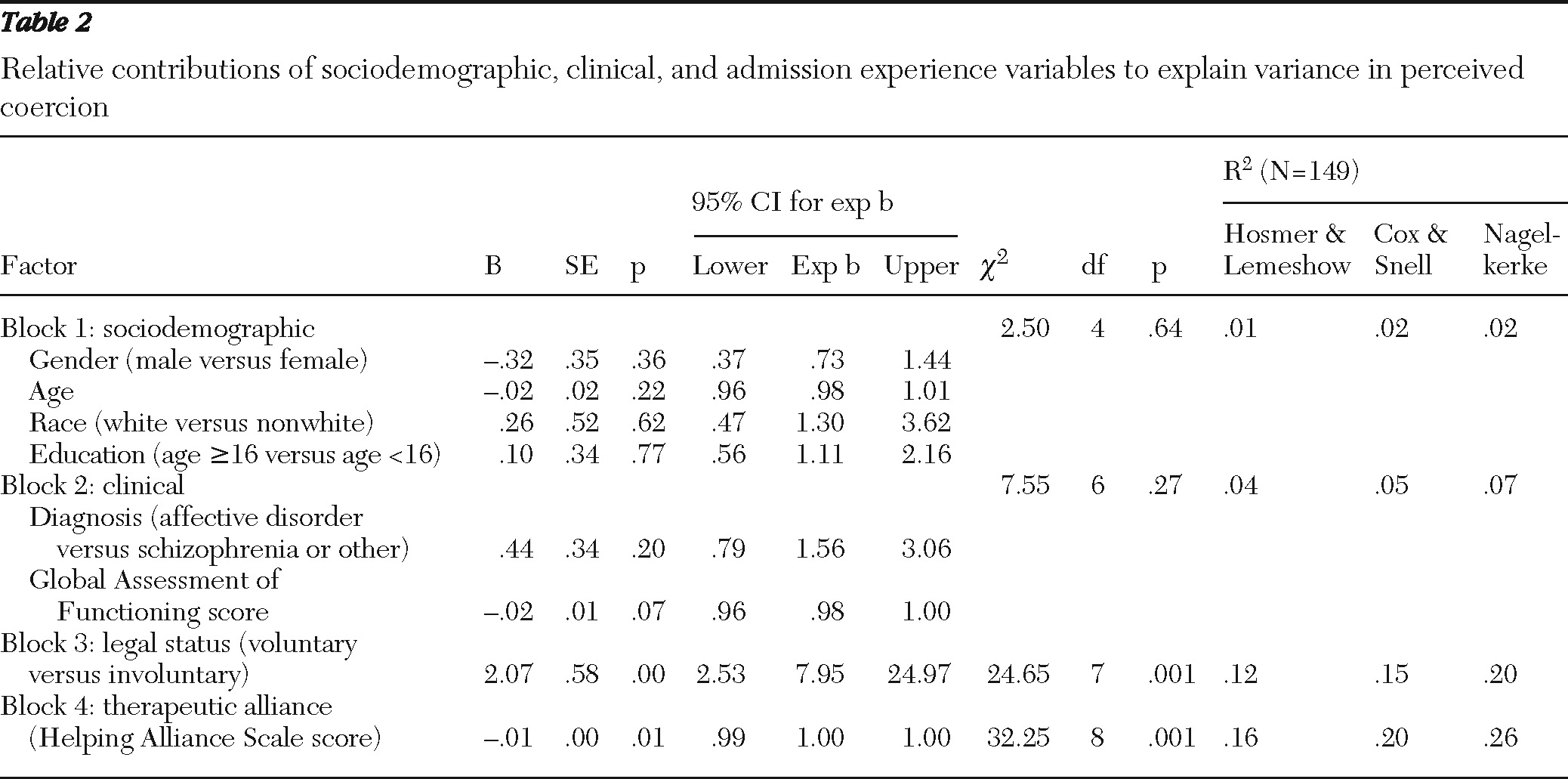
Table 2 shows the blockwise decomposition of the hierarchical logistic regression analysis. In the first block, sociodemographic characteristics (gender, age, race [white or nonwhite], education [below age 16 and age 16 and above] were entered. These variables did not significantly improve the prediction of perceived coercion and explained approximately 2% of the variance in perceived coercion level. Clinical characteristics (diagnosis [affective disorder versus other disorder] and GAF score) were added in the second block but without significant improvement in the prediction of perceived coercion, explaining approximately 5% of the variance. In the third block, legal status (voluntary or involuntary admission) was entered and significantly improved the prediction of perceived coercion, explaining approximately 15% of the variance. Adding the HAS score in the fourth block increased the amount of variance explained to approximately 21%, significantly improving the prediction of perceived coercion level and partially confounding the effect of legal status.
Discussion
To our knowledge, this is the first study to quantitatively investigate the correlation between the therapeutic relationship and perceived coercion. The finding of a significant association between these variables indicates that similar factors affect the assessment of both. Whereas perceived coercion was also associated with legal status at admission, the multiple-variable analysis suggests that the therapeutic relationship may have modified these perceptions among patients regardless of whether their admission was voluntary or involuntary.
Therapeutic relationship and perceived coercion
Acquiring a better understanding of the association between the therapeutic alliance and perceived coercion is important because of the complexities of the relationship between patient and clinician in mental health care. In few areas of medicine do clinicians have the power, which is regularly exercised, to involuntarily hospitalize and treat their patients. The correlation between legal status and perceived coercion found in this study replicates the findings of other studies in this area (
24,
25,
31–
35). Of greater interest and clinical relevance is the association between the therapeutic relationship and perceptions of coercion. Patients who experienced high levels of coercion tended to rate their relationship with the admitting clinician more poorly than those who experienced low levels of coercion. This was true for both voluntarily and involuntarily admitted patients. This quantitative finding supports recent qualitative studies showing that coercion, as experienced by the patient, consistently had a negative impact on relationships (
7,
36,
37). Gilburt and colleagues (
7) concluded that coercion was the main barrier to the formation of a therapeutic relationship and that the coercive experience of involuntary admission is “not necessarily a function of the Mental Health Act, but of the relationship with the staff enforcing aspects of it.”
The cross-sectional nature of our study, however, does not allow the causality of this relationship to be determined. It is unclear whether patients felt less coerced because of their more positive relationship with their clinician or whether feeling coerced prompted them to rate this relationship more poorly. It is also possible that factors that contribute to these ratings influence each one independently of the other. There is some concern that several of the apparently distinct measures of psychiatric patients' assessments of their care (including their quality of life, satisfaction with services, and therapeutic relationship) may all reflect a more unitary disposition toward care (
38). Further research is required to investigate this association. It is not a question that can easily be tested in a controlled trial, but longitudinal studies should be able to determine the time sequence of the relationship and thereby suggest directionality.
The multiple-variable analysis demonstrated that the therapeutic relationship and sociodemographic and clinical variables explained approximately 21% of variance in perceived coercion level. This low percentage may reflect that the study addressed only the relationship between the patient and the clinician whom the patient felt was most responsible for the admission. Although most patients identified a psychiatrist as being most responsible, their experience may also be influenced by other individuals in their social network, including family, friends, and colleagues (
5). Moreover, clinicians are embedded within a complex mental health system. Patients' opinions of the system and other health professionals involved may also play a role in their experience of coercion. Exploring how these relationships interact and influence perceptions is a promising area of future research (
5).
Therapeutic relationship as a target for intervention
There has been only one published study reporting the development and testing of an intervention to reduce perceived coercion (
39). Sorgaard (
39) attempted to increase patients' sense of procedural justice by engaging them in formulating the treatment plan, performing regular evaluations of treatment progress, and renegotiating these plans when necessary. The intervention had no effect on perceived coercion. One possible explanation is that this type of intervention required a positive relationship between the patient and clinician to be effective.
Our study suggests that there may be opportunities for interventions to reduce perceived coercion by improving the therapeutic relationship. The ability of clinicians to establish and maintain a positive therapeutic relationship can be enhanced through training and supervision (
40,
41). Gask and colleagues (
40) found that general practitioners trained to assess and manage depression were rated by their patients as better at listening and understanding their concerns. However, there remains a paucity of research in this area. Priebe and McCabe (
5) have suggested that “studying and improving therapeutic relationships in psychiatry is a core task for social psychiatry.”
Limitations of this study
There are several methodological limitations in this study. First, a substantial number of patients were either excluded or refused to participate. Approximately 22% were excluded because they were discharged or transferred before they could be approached or were deemed by ward staff to be too ill or intellectually impaired to participate or had insufficient proficiency in English to enage in the interview. A further 15% refused to be interviewed. Although this nonparticipation rate is similar to rates reported in other studies of perceived coercion, it is important to recognize that the individuals who were excluded may have had different attitudes toward the hospitalization process (
8,
31,
32).
Second, the study was single site (one city) and may not be representative of patients in other countries or other areas of England. Thresholds for hospitalization and use of involuntary admission vary greatly within England and Wales, and our study included a greater proportion of voluntarily admitted patients and more white and highly educated patients than in the only published study of perceived coercion in the United Kingdom (
24,
42). Despite these differences, our results are closest to those of Bindman and colleagues (
24), suggesting that our findings may generalize to England and Wales.
Third, as previously mentioned, the cross-sectional nature of the study makes it difficult to determine causality. Further research is required to investigate this association and establish the directionality of the relationship. Finally, although the rating of perceived coercion made during the interview was retrospective, patients' assessment of the therapeutic relationship may have reflected an ongoing relationship with the clinician during hospitalization. To minimize this, all patients were interviewed during their first week of admission to the hospital, but it is still possible that the inpatient experienc may have influenced their responses to the HAS statements.
Conclusions
This was an initial quantitative study of the association between the therapeutic relationship and perceived coercion. The experience of coercion and the therapeutic relationship during psychiatric hospital admission were found to be correlated, suggesting that similar factors may influence the patient's experience of both. Hospitalization, even when voluntary, was viewed as more coercive when patients rated their relationship with the admitting clinician negatively.
Acknowledgments and disclosures
Dr. Sheehan was funded by scholarships from the Rhodes Trust and Christ Church, a college of the University of Oxford. The authors thank Helen Doll, D.Phil., for her statistical advice.
The authors report no competing interests.