Illness management and recovery is a curriculum-based approach to help adults with severe mental illness learn how to manage their illness and pursue recovery goals (
1). Developed as a part of the National Implementing Evidence-Based Practices Project (
2), illness management and recovery programs address national policy that encourages effective interventions for recovery from mental illness (
3). Initial research, including two randomized trials (
4,
5) and several pre-post studies (
6–
8), have shown improvements in self-management, achievement of personal goals, and coping. Salyers and colleagues (
9) also showed a reduction in hospitalization.
Assertive community treatment (ACT) is widely recognized as an evidence-based practice that engages consumers with severe mental illness in treatment, reduces hospitalization, and increases housing stability (
10,
11). ACT organizes services through a multidisciplinary team (which may include a psychiatrist, nurse, social worker, employment specialist, substance abuse specialist, peer specialist, and other case managers) to provide assertive outreach, frequent contact, and comprehensive services to meet the treatment needs of consumers who have not engaged in traditional, office-based treatment. ACT is usually reserved for consumers who are most disabled by their mental illness—those with a history of frequent hospitalization, homelessness, or incarceration. Although ACT has been effective in addressing these difficulties, ACT may not always be provided in ways that fully support illness recovery (
12), and critics have argued that ACT is coercive and paternalistic (
13,
14).
To address these concerns, ACT teams have begun to integrate illness management and recovery services (
7,
9). Illness management and recovery is built on the principle of self-determination—that by empowering consumers with self-management tools, they can be active partners in the treatment and recovery process. The program promotes effective strategies for teaching illness self-management, including psychoeducation, optimizing the use of medications, coping skills training, and relapse prevention techniques (
15). However, the impact of this program on the use of more costly services, such as hospital and emergency room visits, has not been widely studied.
Our objective was to assess the impact of illness management and recovery on health service utilization by mental health care consumers who participated in ACT programs. Medicaid health service utilization data were routinely provided to the ACT Center of Indiana for ongoing program evaluation. We hypothesized that consumers who received illness management and recovery and those who graduated from the program would use fewer hospital days and emergency room visits than those who received ACT alone. Although hospitalization and use of emergency services may be necessary at times, these events are generally viewed as negative consumer outcomes, both because of the disruption and turmoil involved for the consumer and the costliness of these services. Because ACT has been shown to reduce hospitalization (
10) and the model itself includes 24-hour access to the team to prevent psychiatric emergencies, any additional impact of a self-management program could be an important contribution.
Methods
Study design
This was a retrospective cohort study of consumers receiving services from five ACT teams in Indiana between July 1, 2003, and June 30, 2008. We chose these teams among the 32 certified ACT teams in the state because illness management and recovery services had been implemented at those sites in a systematic manner. Beginning in 2003, one community mental health center piloted illness management and recovery with one ACT team (
7); in 2006, two additional teams in the same center began providing illness management and recovery. Two other community mental health centers had participated in a study to integrate illness management and recovery into ACT teams beginning in 2004 (
9). This study and its procedures were approved by the institutional review board at Indiana University-Purdue University Indianapolis.
Program models
ACT.
ACT programs follow standards established by the state to maintain certification and funding. Staffing includes a master's-level team leader, a psychiatrist, and other specialist providers (including at least one registered nurse, a vocational specialist, and a substance abuse specialist). Standards also specify frequency, intensity, and type of services offered (such as symptom management, crisis assessment, and crisis intervention). ACT teams are designed to serve consumers with the most severe disabilities, including a diagnosis of a serious mental illness and extended or frequent hospitalizations or use of emergency services, criminal justice involvement, or homelessness.
Illness management and recovery.
Illness management and recovery is a curriculum-based approach to helping consumers set and achieve personal recovery goals and acquire knowledge and skills to manage illnesses independently (
1). The program incorporates five main evidence-based techniques for improving illness self-management and achieving personal goals, including psychoeducation, cognitive-behavioral approaches to medication adherence, relapse prevention, social skills training, and coping skills training (to cope with persistent symptoms, for example). These sessions are usually held weekly over a ten-month period and cover topics organized into ten modules. Each module includes an educational handout, checklists, and worksheets to enhance learning. Material is taught with a combination of educational techniques, motivational interventions, and cognitive-behavioral techniques. Fidelity to the model is assessed with the Illness Management and Recovery Fidelity Scale (
16). Each of 13 items is rated on a 5-point behaviorally anchored scale, ranging from 1, not implemented, to 5, fully implemented.
Integration of ACT and illness management and recovery.
Each of the ACT teams had at least one peer recovery specialist (a consumer doing well in recovery) providing services. Two of the teams also identified another clinician to provide illness management and recovery services. Regardless of provider type, all illness management and recovery specialists received a two-day training course that included didactic materials, discussion, viewing of practice videotapes, and role-playing and other experiential exercises. Specialists had access to technical assistance via phone and e-mail, and they participated in group supervision within their own agency. Illness management and recovery services were provided individually to consumers on the teams. Because of participation in prior studies, three of the teams had fidelity assessments, and by 12 months had reached a “good” level of implementation (that is, a score of 4 out of 5) (
8,
9).
Study sample
The sample included all consumers treated by the five ACT programs who also had Medicaid claims data indicating any services received between July 1, 2003 (the fiscal year that illness management and recovery first started in Indiana), and June 30, 2008. Consumers were included from the month they enrolled in ACT until either June 30, 2008, or the date of discharge. Illness management and recovery status was determined through a combination of archival data augmented with agency records to indicate which consumers received the services, start and end dates, and whether a consumer completed all ten modules (“graduated”).
Measures
From Medicaid claims, we created a data set using person-months as the level of analysis for the entire five-year period. For each observation month, we created variables for the number of days hospitalized and the number of days with one or more emergency room visits for psychiatric reasons. Events were classified as “psychiatric” if the primary ICD-9 diagnosis code for a visit was for a mental illness (ICD-9 codes 290 through 316, inclusive). The state annual reporting system included age, race, gender, education level, employment (employed or unemployed), primary mental health diagnosis provided by the ACT team (ICD-9 codes 293.81 through 293.82 and 295.00 through 298.90 covered psychoses, and 293.83 and 296.00 through 296.90 covered mood disorders), and concurrent diagnosis of a substance use disorder (present or absent). Because these data were collected annually, the most recent prior assessment was used for each observation month. For each month, we coded illness management and recovery status (categories were none, some, dropout, or graduate). For example, if a consumer began illness management and recovery in January 2004 and graduated from the program in December 2004, for the months prior to January, illness management and recovery status would be “none.” Beginning January 2004, the consumer's status would be “some,” and from December 2004 onward, the status would be “graduate.” The Medicaid data, the state reporting data, and the ACT Center data were linked with a unique identification number assigned by the state.
Data analysis
Separate models were fit for the number of inpatient visits and the number of emergency room visits. We used zero-inflated negative binomial models for several reasons. First, we were predicting count data, and the simplest of count regression models (Poisson) would underestimate the variance in our sample. The negative binomial model does not restrict the variance to be equal to the mean (
17) and therefore fit our data better than a Poisson regression. In addition, zeroes occur more frequently in the data than predicted by a Poisson model (that is, most people were not in the hospital or emergency room for most observation months). We accommodated this overrepresentation by using a zero-inflated model (
18,
19). This model entailed a two-part regression that both tested the probability of having no visits (a binomial model) and then predicted a count of the number of visits. Such a model allows zeroes to be accounted for by the binomial distribution and by the count distribution, thus allowing the model to fit the higher occurrence of zeroes in our outcome variables. The zero-inflated negative binomial model has been useful in predicting low base-rate phenomena in other studies (
20,
21). A Vuong test (
17) indicated that the zero-inflated negative binomial model fit better than the negative binomial model.
The data had a high level of heteroskedasticity; because each person-month was a separate data point, data nested within a participant varied less than data points for other participants. Heteroskedasticity causes the usual standard error estimates to underestimate the variance, thus resulting in alpha inflation. In order to avoid this, we used a robust covariance matrix estimator (
18) to better estimate the standard errors.
In each regression analysis, we controlled for demographic characteristics, employment, diagnosis, and concurrent substance use disorder. We also controlled for team effects by using dummy variables. Team 1 was the reference team.
Results
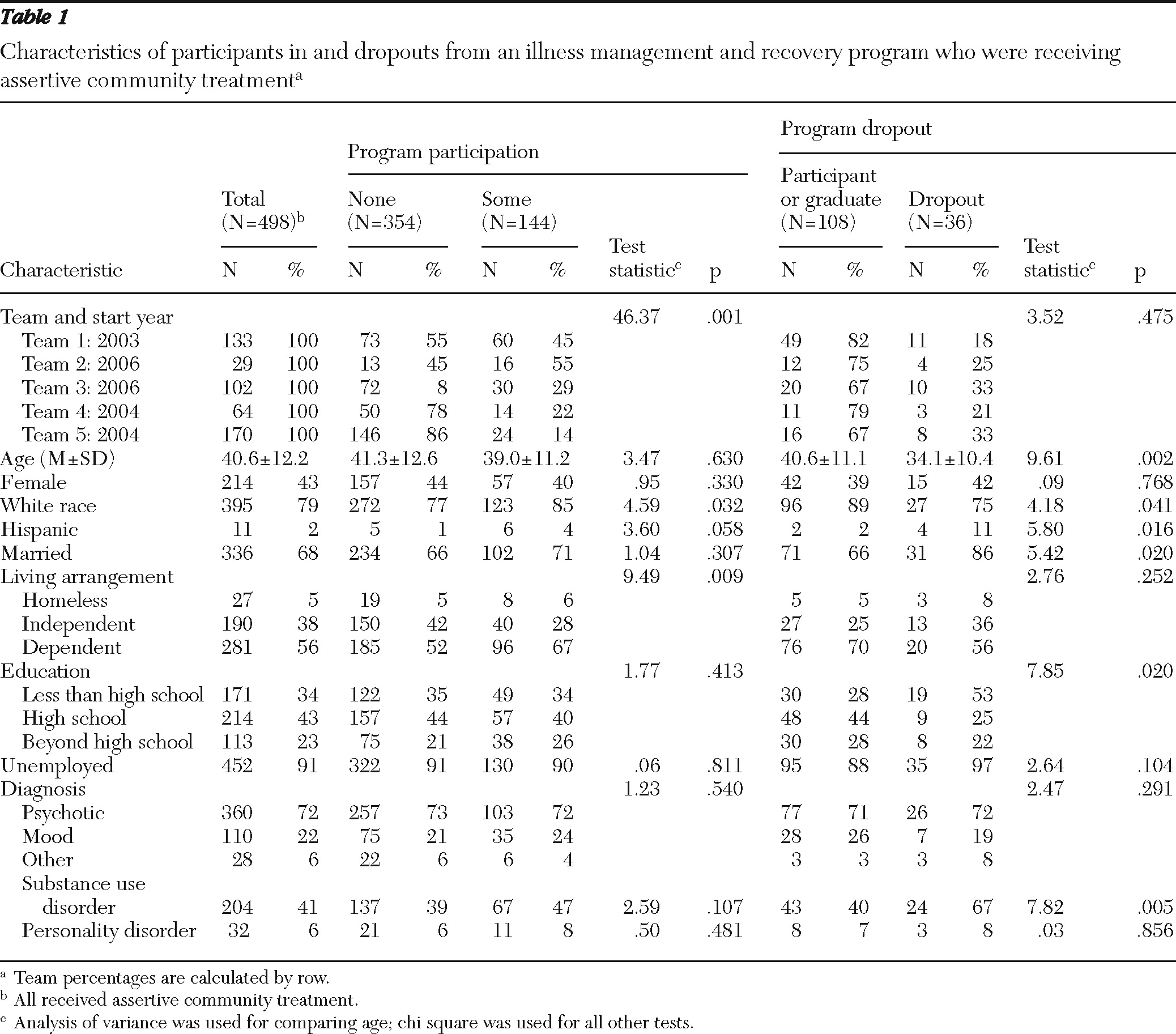
Of 645 consumers served by the ACT teams during the study period, 498 (77%) had both Medicaid claims and state data and were included in the study sample. The mean±SD length of time on ACT during the study period was 2.4±1.4 years. A total of 144 (29%) consumers received illness management and recovery services (
Table 1), with a mean service period of 10.0±6.3 months, a median of nine months, and a maximum of 37 months. Only one individual spent more than 24 months in illness management and recovery, and 105 (73%) received the service for 12 months or less. Although some participants took breaks from the program, we considered consumers to be in the program unless there was a discharge or graduation date. This approach allowed us to conservatively estimate the effect of illness management and recovery. The proportion of consumers who received at least some illness management and recovery ranged from 14% with team 5 to 55% with team 2. Of those participating, 47% completed the entire ten-module curriculum; graduation rates across teams ranged from 6% with team 2 to 67% with team 1 (the first team to have illness management and recovery).
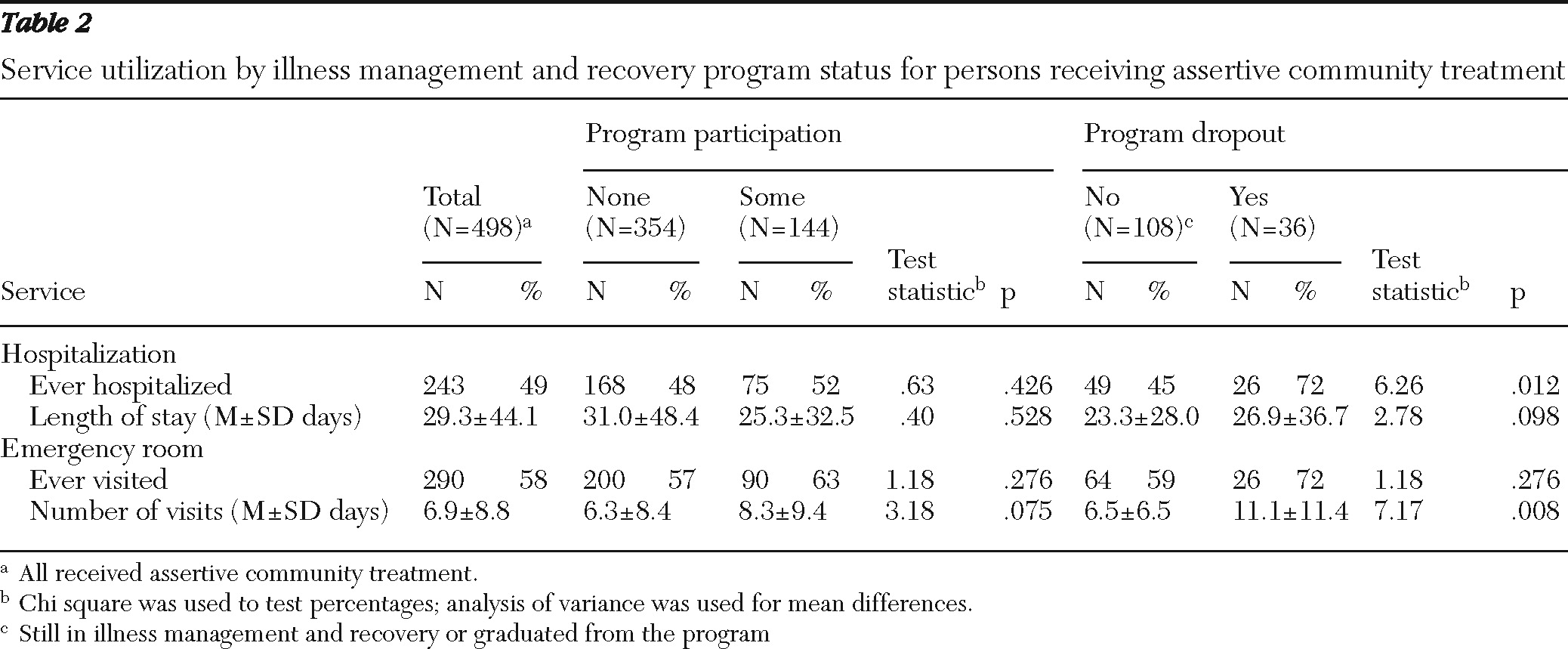
As shown in
Table 1, participants were about 40 years old; most were male and white. A majority had a primary diagnosis of a psychotic disorder; many also had a co-occurring substance use disorder, and some had a comorbid personality disorder. Illness management and recovery participants were significantly more likely than those who received ACT alone to be white. Participants were also less likely to be living independently. Compared with other illness management and recovery participants, consumers who dropped out of the program were significantly younger, less likely to be white and more likely to be Hispanic, more likely to be married, had lower education, and were more likely to have a substance use disorder. As shown in
Table 2, dropouts also were more likely to be hospitalized, and they used more emergency room days than consumers who did not drop out during the study period. All background characteristics were included as covariates in the regression analyses.
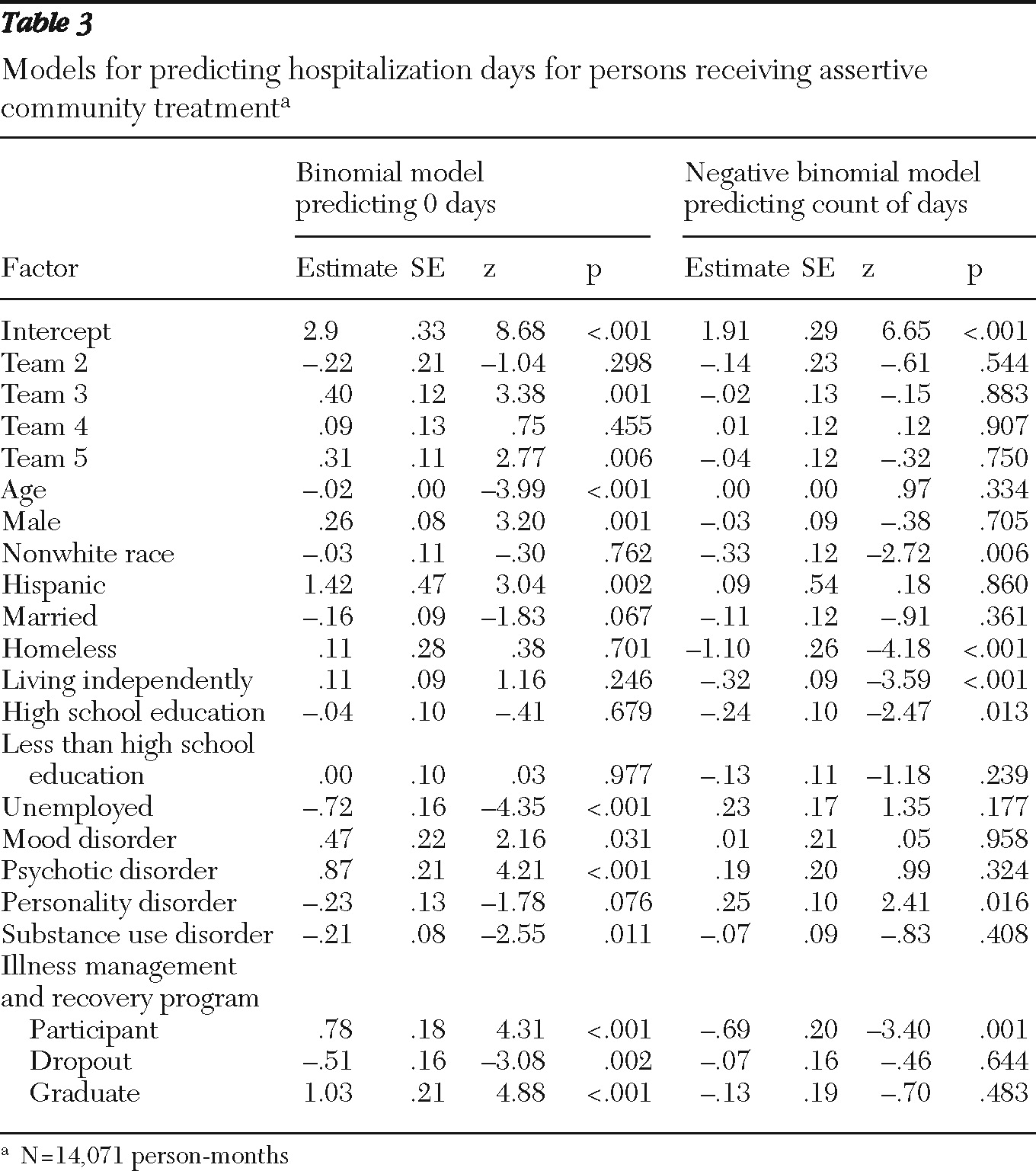
Hospitalization days
As shown in
Table 2, 49% of ACT consumers were hospitalized during the study period. As shown in
Table 3, enrollment in and graduation from the program were associated with a lower probability of being hospitalized (predicting zero hospitalizations), whereas program dropout was associated with a higher rate of hospitalization. In the count part of the prediction model, enrollment in illness management and recovery was significantly related to fewer hospitalization days compared with those who received only ACT services (
Table 3). For example, consumers enrolled in the program were significantly more likely to have zero days hospitalized (z=4.31, p<.001) in the first part of the model. Excluding the excess zeroes, we found that those consumers had 50% fewer days of psychiatric hospitalization each month compared with those enrolled in only ACT.
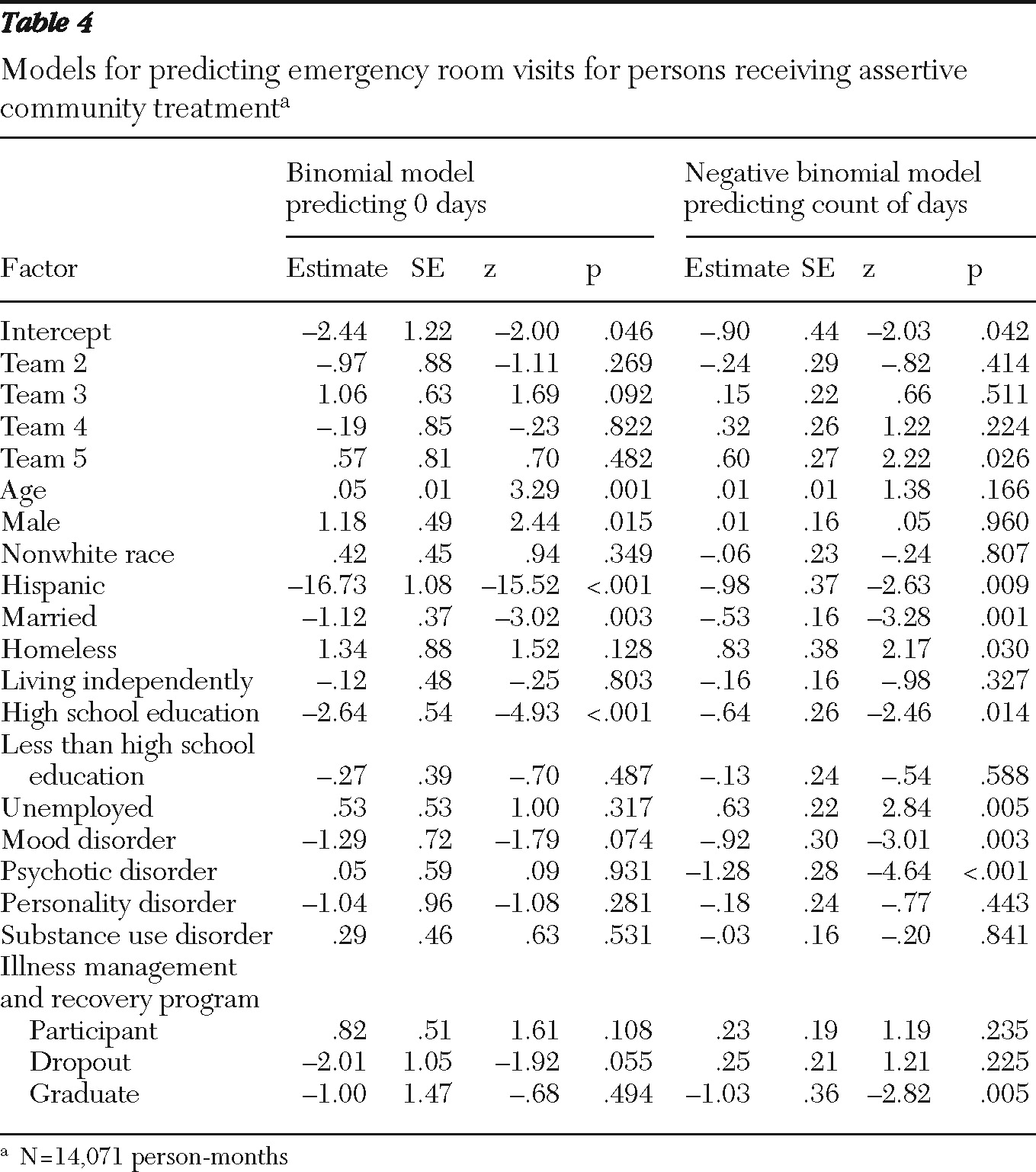
Emergency room visits
Illness management and recovery participation, dropout, and graduation were not significantly related to prediction of zero emergency room visits; however, in the count part of the model, graduation was significantly related to having fewer emergency room visits (
Table 4). Excluding the excess zeroes from the model revealed that program graduates had 64% fewer emergency room days than those enrolled in only ACT.
Discussion
This natural experiment was the first large-scale study to examine the relationship between illness management and recovery and health service utilization and the first to directly compare the combination of ACT and illness management and recovery with ACT alone. As hypothesized, illness management and recovery participation was associated with a significant reduction in the number of inpatient days, even after we controlled for site, demographic characteristics, employment, diagnosis, and concurrent substance use disorder. While in the program and after graduating, consumers in illness management and recovery were more likely to have no psychiatric hospitalizations. In predicting the number of days hospitalized, being enrolled in illness management and recovery was associated with fewer days. Graduation from the program was associated with a decrease in the number of emergency room visits.
Reductions in hospitalization and emergency room visits have both economic and humanistic value. From a personal recovery point of view, quality of life is lower for consumers in hospital settings compared with community settings (
22–
24). Moreover, it is difficult to pursue meaningful life goals while hospitalized. In addition, from a public policy perspective, the investment in recovery-based services may help manage treatment costs. An important step will be to examine the costs and offsets associated with illness management and recovery programs in order to assess the economic contributions of recovery-based services. Even more pressing, however, is the need for well-controlled trials of illness management and recovery in the population receiving ACT services.
Across five teams, there was a 25% dropout rate, which is within the range of rates reported in other studies (11%–50%) (
4,
6,
8). Notably, 47% of consumers who enrolled completed all ten modules. Given the population served by ACT teams, and the focus on individualized community-based services, completing a long, structured curriculum is impressive. We identified as graduates those who completed all ten modules. However, Levitt and colleagues (
5) used a more lenient criterion of “exposure to the program,” with participation in five or more modules (and 54% of their participants met that criterion). We do not know how much of the illness management and recovery program must be completed to realize and maintain gains. In our study, most people completed the program within a year, but a sizable minority (26%) took longer than a year to graduate. Anecdotally, we know that several consumers took breaks from the program and then resumed participation. Similarly, graduates would sometimes return for refresher modules.
Because this was an observational study and we could not control for who received illness management and recovery services, our findings may be subject to selection biases. We do not know how consumers were selected to participate. Sites had a kickoff presentation early in the implementation; some consumers may have been self-referred. Participants were more likely to be white and less likely to be living independently. Those who dropped out were more likely to belong to a racial-ethnic minority group and to be younger and married, have less education, and have a co-occurring substance use disorder. Clearly, more work is needed to examine and minimize the possible racial disparities in receipt and completion of illness management and recovery services, including attention to cultural sensitivity of providers and materials. The finding that education was a factor in engagement is also concerning. The program relies heavily on written materials, with worksheets and handouts. Clinicians have described adapting materials for reading level, but more work may be needed to ensure broader utility. Although we could not randomly assign people to receipt of illness management and recovery, we were able to control for several background variables in the regressions. Moreover, all were receiving ACT services and were likely to be more homogeneous than a general outpatient population.
The observational nature of the study also limited our control over the implementation of the services. All of the teams had peer recovery specialists, but two teams had an additional clinician. All providers received the same training and implementation support and, from our examination of available fidelity data, appeared to be implementing the model well. However, the impact of provider type is unknown. Teams differed on length of time to implement the program and geographic location, both of which could affect hospitalization or emergency room use. We were also limited by reliance on administrative data; diagnosis is often underreported and may result in underestimates of service utilization for mental health reasons (
25,
26). In addition, background characteristics captured in the state's annual reporting system may not reflect changes (such as in employment status) that could affect service use. Finally, the study is limited in its generalizability because most participants were white males in one state.
Conclusions
Prior research on illness management and recovery has shown positive results, primarily with self-reported or clinician-reported measures of illness self-management and coping (
4,
6,
8,
9). This study is an important next step in documenting the utility of the program by going beyond such measures and observing actual service use. Our findings are particularly robust because all consumers in the study were enrolled in ACT and most were enrolled in Medicaid. We had fairly complete data that were representative of the overall ACT population. Given that ACT participation has repeatedly shown decreased hospitalization (
10), the finding that illness management and recovery was associated with incremental benefit in this context is impressive. The program may be an important supplement in helping consumers learn effective ways to manage illnesses, resulting in lower utilization of costly acute care services. Further controlled research on the cost-effectiveness of recovery-based interventions may improve allocation of resources for consumers with serious psychiatric illness.
Acknowledgments and disclosures
This study was funded by Bristol-Myers Squibb and builds on an earlier study funded by the National Institute of Disability and Rehabilitation Research (H133G030106). The work was also supported by grant R24-MH074670 (Recovery Oriented Assertive Community Treatment) from the National Institute of Mental Health. The authors appreciate the participation of the Adult and Child Mental Health Center in Indianapolis, of Park Center in Fort Wayne, and of the Northeastern Center in Kendallville, Indiana.
Dr. Salyers reports being a former co-owner of Target Solutions, LLC, which provides consultation and training in illness management and recovery. Dr. Kim reports being a former employee and current shareholder of Bristol-Myers Squibb and being a current employee and shareholder of Novartis. The other authors report no competing interests.