People with schizophrenia experience serious health problems, social disadvantages, and unmet needs in multiple life domains. They need access to high-quality treatment in the community to enable them to go through life as valued citizens. Provision of such care requires a comprehensive system on a regional scale—a system that patients can readily understand offers potential benefits for their recovery (
1).
To some extent, service improvement is a matter of perception. Patients, their families, and clinicians, each have their own views on how systems should identify needs (
2) and prioritize services (
3). From a professional point of view, a service system should consist of evidence-based practices, such as assertive community treatment (ACT), and state-of-the-art pharmacotherapy. In reality, many patients are confronted with inadequate services. The introduction of treatment guidelines is an important step toward providing better services, but it is not sufficient. Implementing evidence-based practices involves many factors, such as leadership, training, outcome monitoring, and funding (
4).
The Netherlands is a small European country with a dense population of 16.6 million people; approximately 120,000 persons in the Netherlands have a diagnosis of schizophrenia. The mental health care system is comprehensive and accessible. Although most persons with severe mental illness receive community-based care, the number of hospital beds remains relatively high, at about 1.8 per 1,000 inhabitants (
5).
This study addressed the availability of mental health services for persons with schizophrenia in eight regions and satisfaction with these services among stakeholder groups. An assessment instrument was developed to identify the strengths and weaknesses of regional service systems and to provide a sound footing for efforts to improve these systems by promoting evidence-based practices. Whereas the baseline assessment can be considered as an evaluation of “regional care as usual,” the follow-up assessment was meant to identify changes in service provision after the introduction of the first multidisciplinary guidelines for schizophrenia in the Netherlands (
6).
Methods
The Quality Assessment of Regional Treatment Systems for Schizophrenia (QUARTS) consists of two questionnaires. The first contains more than 100 questions about 25 relevant aspects of schizophrenia care (
7,
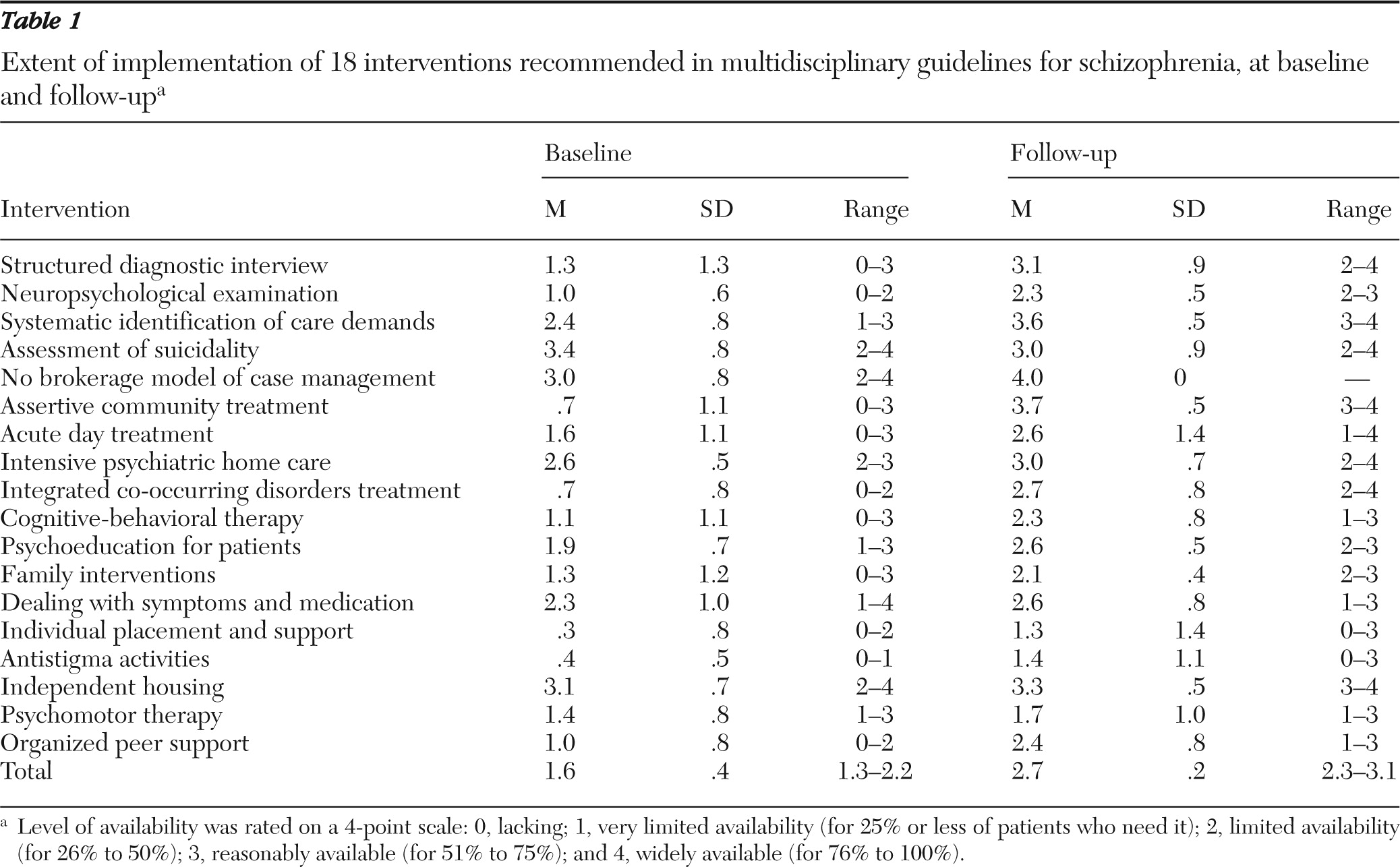
8), including the 18 major interventions that are recommended in the Dutch guidelines (see
Table 1). The first questionnaire determines the availability and coverage of these interventions in a region. The questionnaire has five sections: reaching the target group, diagnosis and treatment, rehabilitation and community support, focus on demand and patient rights, and organization of care. The questionnaire is completed during a group session that involves about ten clinicians. They must reach a consensus concerning the level of availability of each aspect of care; ratings are 0, lacking; 1, very limited availability (for 25% or less of the patients who need it); 2, limited availability (for 26% to 50% of patients); 3, reasonably available (for 51% to 75%); and 4, widely available (for 76% to 100%). The second questionnaire asks participants about their satisfaction with each aspect of care in the past 12 months: 1, poor; 2, moderate; 3, satisfactory; and 4, good.
During structured group sessions in a participating region, the questionnaire is completed individually by members of four stakeholder groups (about ten individuals per group): mental health professionals, patients with schizophrenia, family members, and representatives of community organizations (such as general practitioners, staff of homeless shelters, police, and staff of housing associations). During the group interviews, participants can expand on their individual responses by citing details of their experiences.
Mental health care institutions can participate on a voluntary basis and cover the costs of the review. The reviewing body is the Dutch Schizophrenia Foundation (since January 2010, the Phrenos Foundation). First, independent researchers gather all data (the first, second, and fourth authors were members of this group). Then a review committee of experts from another region of the Netherlands (psychiatrist, nurse, schizophrenia patient, and family member) discusses specific themes with all the stakeholders in the region during a day-long site visit. The committee gives an overall evaluation and appends its recommendations to the final review report. [Further details about the QUARTS process, including a table listing the care elements, are available in an online appendix to this report at
ps.psychiatryonline.org.]
This study was based on data obtained from groups of stakeholders and was judged exempt from review by an institutional review board. Both the board of the Schizophrenia Foundation and the boards of directors of the eight participating mental health organizations approved the study.
Results
From 2003 to 2009, eight regions of the Netherlands were assessed twice using QUARTS. Taken together, these eight regions are highly representative of all regions in the Netherlands. Seven regions consist of a city of approximately 100,000 inhabitants plus outlying rural or semirural areas; the eighth region is part of a major city. The mean±SD time between the first and second assessments was 44 months (range 28–72 months). At baseline an average of 38 persons per region (range 23–49 persons) participated in the QUARTS procedure. At follow-up the mean number of participants fell to 24 (range two to 36 persons); service users and representatives of community organizations in particular often dropped out at the last minute. Because of the pressure of work and budget restrictions, two regions opted for an abridged QUARTS procedure at follow-up, in which two to four key clinicians participated.
On average across all regions, availability of the entire range of care elements increased between the baseline and follow-up interviews. At baseline there was limited availability (for 25% to 50% of all patients who needed the service), and at follow-up availability had nearly reached reasonable limits (for 50% to 75% of patients who needed the service). At both assessments, availability was highest in the areas of “focus on demand and patient rights” and “diagnosis and treatment” and lowest in the areas of “rehabilitation and community support” and “organization of care.”
Table 1 shows that the availability of the interventions recommended in the guidelines improved significantly, with the total mean score increasing from 1.6 to 2.7 out of 4.0, which represents a slightly higher increase than for all of the 25 care elements in QUARTS (from 2.0 to 2.7; data not shown).
The largest improvements involved availability of the structured diagnostic interview (an improvement of 1.8 points), of integrated co-occurring disorders treatment (a 2.0-point improvement), and especially of assertive community treatment (ACT; a 3.0-point improvement). In contrast, at follow-up the individual placement and support (IPS) model of supported employment, antistigma activities, and psychomotor therapy were still rated at less than limited availability.
The availability of the 18 interventions in the guidelines increased more in the regions that had lower scores at the first assessments. As a consequence, the differences in availability between all regions became smaller at the second assessments; availability scores ranged from 1.4 to 2.2 (mean=1.7) at the first assessment and from 2.4 to 2.7 (mean=2.6) at the second.
Among all participants, the mean satisfaction rating for the provision of all 25 care elements increased slightly—from 2.5 to 2.7—approaching “satisfactory.” The lowest satisfaction rating at the first assessment was for rehabilitation and community support (mean=2.5). On average, ratings provided by mental health professionals were slightly higher than those provided by the other stakeholder groups (data not shown). A recurring theme in participants' explanations of their rating was the perception of substantial variation in the quality of care, which was particularly dependent on the performance of individual clinicians. Patients and family members were critical of the lack of information from clinicians; many were unaware of which elements of care were available and who was eligible for them.
At the follow-up assessment, all key clinicians in the assessed regions noted that the multidisciplinary guidelines stimulated them to focus on evidence-based interventions. Each region perceived as helpful the specific recommendations provided by the review committee of experts as part of the QUARTS assessment.
Discussion
In eight regions of the Netherlands, the perceived improvement in care provision over two to four years was substantial. Most aspects of care that were rated to have adequate availability at follow-up were those in the “core business” of psychiatry—for example, diagnostics and pharmacotherapy. This study also illustrated the rapid implementation of ACT. The ACT model provides a good peg for other evidence-based practices (
9), such as the IPS model of supported employment. Although IPS is feasible in the Netherlands (
10), it is not widely implemented, which indicates a lack of focus on the social inclusion of persons with mental illness. Overall, half of all patients in most regions had no access to some elements of the care standard. Partly for this reason, patients and family members rated many care elements as less than satisfactory. Case register data indicate that from one-quarter to one-third of all persons in the Netherlands with schizophrenia do not receive care from the mental health system. Thus only a small minority of the whole group stands to benefit from evidence-based practices.
These findings suggest that care for persons with schizophrenia in the Netherlands still has many deficits, as in many other countries. In the United States, nearly half of all people with schizophrenia receive no mental health care at all, and only a minority has access to effective interventions (
11). This science-to-service gap (
12) is less wide in the Netherlands because of more favorable social insurance regulations and more accessible mental health care. Patients with low incomes report far fewer financial barriers to service utilization in the Netherlands than in the United States (
13).
This study did not provide a decisive answer about which factors contributed to the improvements in the regions. The multidisciplinary guidelines for schizophrenia played a part in the overall improvements, although the Netherlands had not developed a plan to implement these guidelines nationwide or to offer substantial incentives to service providers to adopt them. Therefore, it is likely that the QUARTS procedure contributed to the progress made in the regions. Participants perceived the recommendations given by the review committee as offering genuine encouragement. They took action to implement these recommendations, such as reorganizing care along the lines of ACT and cooperating more closely with other care agencies. Clinicians were encouraged to take part in educational activities related to schizophrenia care. Five of the eight regions participated in projects that used the Breakthrough Method (
14). In this learning collaborative approach, several regional teams worked together in a structured way to implement specific elements, such as somatic screening or ACT.
The improvements occurred despite other, somewhat negative trends that also may have affected service provision in the eight regions. Dutch mental health care is being transformed from an integrated care system, financed by single-payer national insurance, to a more heterogeneous approach that is financed through several sources and subject to market forces. Concerns have been raised that these changes impede the development of rehabilitation services for people with severe mental illness (
15).
A strength of this study is that it examined the entire scope of regional care provision, not just that provided by a single agency. Another strength of the study is that the perspectives of four stakeholder groups were addressed. However, one limitation is that the groups of participants were small, which tended to undermine their representativeness. The study needs to be replicated with more participants per region, and preferably in other countries. Also, although QUARTS indicates which evidence-based interventions are available, it does not show whether these interventions are carried out with high fidelity. Thus the observed leveling out of the availability of care across regions does not imply that all differences in quality disappeared. Nevertheless, it is our hypothesis that a high QUARTS score is a prerequisite for favorable outcomes for individual patients. This could be tested by linking QUARTS scores to patient-specific data obtained by routine outcomes monitoring.
Conclusions
The multidisciplinary guidelines for schizophrenia were perceived by key clinicians as an important factor in the implementation of evidence-based interventions in the Netherlands, despite the lack of incentives from the government or other financial bodies. QUARTS was perceived as a helpful instrument for monitoring and development of services, leading to a higher quality of routine mental health practice and to a reduction of interregional differences. Nevertheless, Dutch schizophrenia care is still patchy. In particular, support for patients' desires for social inclusion is limited.
Acknowledgments and disclosures
This research was financially supported by grant 100-003-021 from ZonMw, the Netherlands organization for health research and development; by funds from De Open Ankh; and by the following mental health organizations: GGZ Delfland, GGZ Drenthe, GGZ Dijk en Duin, GGZ Noord-Holland Noord, GGZ Noord- en Midden-Limburg, InGeest, Rivierduinen, and Parnassia Bavo Group.
The authors report no competing interests.