Recent research on first-episode psychosis emphasizes the importance of early interventions to initiate remissions and to prevent relapses (
1–
3). The emerging literature on first-episode psychosis highlights the high prevalence and adverse consequences of substance use, misuse, or disorder (
4–
8). Approximately one-half of first-episode clients have a history of cannabis abuse or dependence and one-third have a current cannabis use disorder (
7–
12). The proportions are similar for alcohol use disorders (
7–
9,
13,
14). Smaller but significant proportions have use disorders related to cocaine, amphetamines, barbiturates, and other drugs (
7,
8,
11,
15,
16). Overall, approximately half of all clients with first episodes of psychosis present for treatment with a current substance use disorder. Once in treatment, continued use of alcohol and other drugs is associated with increased symptoms (
6,
9,
16–
19), adjustment difficulties (
17), treatment nonadherence (
16,
19,
20), relapses (
9,
21), and hospitalizations (
7,
9,
19,
22). Thus substance use disorders constitute a major risk factor for these clients. Nevertheless, little is known about the course and treatment of co-occurring substance use disorders among clients with first-episode psychosis.
These issues are much better understood among clients with long-term psychotic disorders. For this population, substance use disorders are common (
1–
5) and are associated with multiple adverse outcomes, including treatment dropout (
23), recurrent hospitalization (
24,
25), violence (
26), homelessness (
27), incarceration (
28), relapse (
29), and victimization (
30), as well as medical problems such as HIV and hepatitis (
31). The course of substance use disorders in this population tends to be chronic and relapsing (
32,
33). Traditional parallel treatment approaches (in separate settings) are ineffective, are fragmented, and result in treatment nonadherence and dropout (
34,
35). The negative outcomes associated with traditional approaches have led to integrated treatments designed to target co-occurring mental and substance use disorders concurrently in the same setting (
36,
37). Several reviews of experimental and quasi-experimental studies support different types of integrated treatment, including group counseling, contingency management, residential treatment, and motivational interventions combined with cognitive-behavioral treatment (
38,
39).
To synthesize existing knowledge regarding substance use disorders among clients with a first episode of psychosis, we systematically reviewed research on course and treatment response. We addressed two clinical questions. First, because clinical wisdom suggests that some clients become abstinent after a first episode of psychosis without specialized substance abuse treatments, how often does this occur? Second, because some clients continue to use substances after a first episode of psychosis and clearly suffer adverse consequences, is the addition of specialized substance abuse treatment effective? The answers to these questions are critical for clinical and research programs on first-episode psychosis.
Methods
We collaboratively established search criteria with assistance from a library scientist at the first author's institution to identify articles on first-episode psychosis (keywords: schizo$, first episode psychosis, early psychosis, recent onset schizophrenia) and substance use disorders (keywords: substance$, drug, alcohol, cannabis, cocaine, marijuana, heroin, methamphetamine) (note $ is a wildcard term). Although tobacco use is prevalent in this population (
40), we specifically excluded studies in which tobacco was the only substance of abuse because treatment processes and sequelae for tobacco are substantially different from those for alcohol and other substances. We used search criteria to identify English-language articles indexed between 1990 and 2009 in MEDLINE, PsycINFO, Cochrane Controlled Trials Register, Cochrane Database of Systematic Reviews, and Sociological Abstracts databases. Among 540 abstracts, we excluded review articles, editorials, commentaries, theoretical articles, and case reports; studies that did not use objective criteria for standardized approaches to assessing substance use disorders; and studies that included fewer than ten clients in each study group. We selected longitudinal studies, including experimental, quasi-experimental, and observational designs, of people with first episodes of psychosis (or early psychosis, schizophrenia spectrum disorders, or affective psychoses) and co-occurring substance use, abuse, or dependence. Using these criteria, we retrieved 115 articles for further review. By searching the citations in articles, we identified 14 additional articles for review.
We divided treatment studies into two categories: those that provided basic interventions for psychosis, including education regarding the need to avoid psychoactive substances to prevent relapses of psychosis, and those that provided some type of specialized substance abuse treatment. Of the 129 articles retrieved for full review, we identified nine studies that described outcomes from psychiatric-only treatment for individuals with co-occurring disorders and five studies that described outcomes from integrated treatments. For each study, we extracted information on study design, substances used, description of interventions, sample size, inclusion and exclusion criteria for intervention and control or comparison group, treatment group, and outcome data. We organized studies by design (randomized controlled trial, prospective cohort, retrospective cohort, case control, and observational) outcomes. Because of the heterogeneity in designs, methods, and measures, we were unable to aggregate data statistically.
Results
First-episode treatment studies without substance abuse treatment
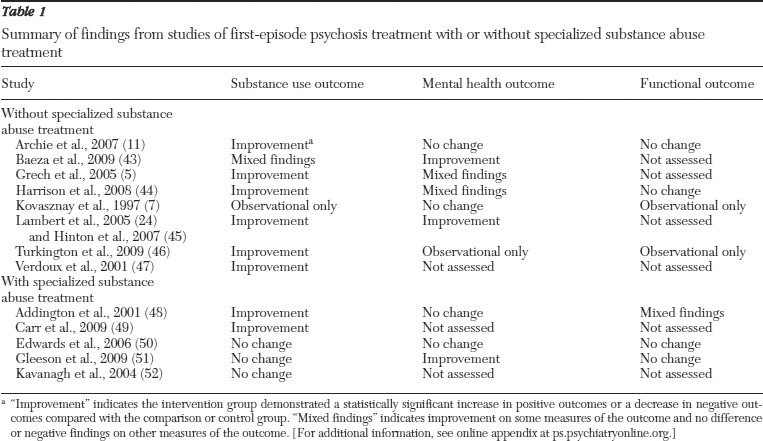
Studies of first-episode psychosis without specialized substance abuse treatment are summarized in
Table 1. [Additional information on these studies, including methodological and measurement details and substance abuse, mental health, and functional outcomes, is included in an online appendix to this article at
ps.psychiatryonline.org.] Archie and colleagues (
11), using data from four psychosis treatment centers in Canada (Toronto, London, Hamilton, and Ottawa), conducted a prospective cohort study on 200 clients with first-episode psychosis. At baseline, 32 (18%) clients met criteria for heavy drinking, 48 (26%) met criteria for hazardous drinking, and 69 (17%) met criteria for drug abuse. Heavy drinking was defined as five drinks or more in a day. A score of 8 or more on the Alcohol Use Disorders Identification Test (
41) met criteria for hazardous alcohol use, and a score of 6 or more on the Drug Abuse Screening Test (
42) met criteria for drug abuse. The treatment programs offered an array of services for early psychosis but no specialized substance abuse treatment services. At 12-month follow-up, significant reductions occurred in drug abuse (from N=64, 32%, to N=34, 17%), hazardous alcohol use (from N=42, 21%, to N=20, 10%), and concurrent drug abuse and hazardous alcohol use (from N=22, 11%, to N=4, 2%) but not in heavy drinking (from N=32, 16%, to N=26, 13%). Although significant differences in involuntary hospitalizations and arrests were found between drug abusers and nonabusers at baseline, these differences were no longer significant at follow-up. Similar trends were reported for the hazardous alcohol users as well as the concurrent drug abusers and hazardous alcohol users.
Baeza and colleagues (
43), using data from six psychiatry departments in Spain, analyzed data for 110 youth ages nine to 17 years with a first episode of psychosis at admission and at six-month follow-up. The programs offered no specific substance abuse treatment. At baseline, 32 (29%) participants were using cannabis, 24 (22%) alcohol, eight (8%) cocaine, and six (5%) other drugs. Cannabis use decreased significantly at six months (from N=32, 29%, to N=15, 14%), but alcohol and other substance use did not. Cannabis users had higher positive symptoms at initial assessment, but at six months they had lower positive, negative, general, and total symptom scores, especially those who stopped using.
Grech and colleagues (
5), in South London, England, evaluated a cohort of 119 clients with recent-onset psychosis at baseline and did a follow-up evaluation after 3.7 years. No specific substance abuse treatment was provided. Sixty-one (62%) participants reported no history of cannabis use at admission or follow-up; nine (9%) participants reported a history of cannabis use at admission but no use at follow-up; 12 (12%) participants without a history of cannabis use at admission reported cannabis use at follow-up; and 16 (16%) participants reported a history of cannabis use at baseline and follow-up. Cannabis users had more positive symptoms and greater continuous course of illness over time.
Harrison and colleagues (
44), who conducted the West London First-Episode Study, reported a naturalistic 14-month follow-up on 152 clients with first-episode schizophrenia. No specialized substance abuse treatments were offered. They obtained substance use data for 85 of the original 152 clients. At follow-up, 15 (18%) clients reported no cannabis use and 12 (15%) reported no drinking. Persistent substance users, defined as using at baseline and at follow-up, experienced more severe symptoms and greater severity of illness overall at follow-up. Clients who reported no lifetime substance use disorder at baseline had greater spatial working memory at follow-up.
Kovasznay and colleagues (
7), from the Suffolk County (New York) Mental Health Project, followed first-episode clients diagnosed as having schizophrenia or affective psychosis disorders. Six months after the baseline assessment, clients with schizophrenia or affective psychosis and a history of substance use disorders (N=84, 42%) were more likely to use cannabis (N=16, 19%) and to do so at least weekly (N=7, 8%) compared with clients without a history of substance use disorders. Clients with affective psychosis and a history of substance use disorders (N=45, 22%) were more likely to drink alcohol at least weekly (N=13, 29%). Clients with schizophrenia and a history of substance use disorders had poorer clinical functioning than clients with affective psychosis. No significant associations with having a lifetime substance use disorder were found with treatment type or medication adherence.
Lambert and colleagues (
3), at the Early Psychosis Prevention and Intervention Centre in Melbourne, Australia, reported on 643 clients with first episodes of psychosis and co-occurring substance use disorder (primarily cannabis and alcohol use disorders) who completed 18 months of treatment. The Early Psychosis Prevention and Intervention program provided comprehensive psychiatric services but did not include specialized substance use disorder interventions. At 18 months, 155 (38%) clients were abstinent, 91 (22%) had decreased use, and 163 (40%) had persistent substance use disorders. Clients whose substance use disorders persisted had more severe disorders (dependence) at baseline. Hinton and colleagues (
45), from the same study, followed 72 clients who were regular cannabis users at treatment entry and received no specialized substance abuse treatment. After nine weeks, 29 (40%) clients were abstinent, and those who continued to use had significantly reduced amounts. Alcohol use in the sample did not change, but use of other illicit substances decreased.
Turkington and colleagues (
46), in the Northern Ireland First Episode Psychosis Study, tracked 194 clients with a first episode of psychosis who received usual care (not measured) in local service systems. At baseline, 81 (43%) clients reported substance misuse (abuse or dependence), mostly alcohol and cannabis. At one-year follow-up, 43 (23%) clients reported substance misuse. Those who persisted with substance misuse had more depressive symptoms at baseline. At follow-up, persistent misusers had more depressive symptoms, more positive symptoms of psychosis, poorer functional outcomes, and more relapses.
Verdoux and colleagues (
47), in Bordeaux, France, followed 65 clients with first-episode psychosis for two years with assessments at baseline and every six months. All clients received usual care. At baseline, 20 (31%) clients had a history of alcohol use disorder, and 15 (23%) clients had a history of drug use disorder. By six months, alcohol and drug use decreased to five of 64 (8%) clients and four of 64 (6%) clients, respectively. The lower proportions remained stable for two years.
First-episode treatment studies with substance abuse treatment
A small number of first-episode programs have developed and studied the outcomes of specific substance abuse treatments that were integrated with the psychosis treatments. These included three randomized controlled trials and two cohort studies, summarized in
Table 1. [Additional information on these studies is available in an online appendix to this article at
ps.psychiatryonline.org.]
Addington and Addington (
6), at the Calgary Early Psychosis Program in Alberta, Canada, described substance use outcomes over a three-year period for 203 of 300 clients with a first episode of psychosis who completed both baseline and year 1 follow-up assessments. Substance use was treated with education and relapse prevention in all aspects of the program, and a specialized treatment group was added for clients who did not become abstinent within one year (
48). At baseline, 105 (52%) clients had one or more substance use disorders (mostly alcohol and cannabis). The proportions with active misuse generally declined in the first year and stayed low: for alcohol misuse, the baseline and year 1, 2, and 3 figures, respectively, were N=37 (35%), N=21 (20%), N=19 (18%), and N=19 (18%); for cannabis misuse, N=35 (33%), N=17 (16%), N=7 (7%), and N=7 (7%); and for other drug misuse, N=11 (10%), N=2 (2%), N=2 (2%), and N=2 (2%). At one-year follow-up, cannabis users had more positive symptoms and greater levels of depression compared with nonusers.
Carr and colleagues (
49), at the Prevention and Early Intervention Program for Psychoses in London, Ontario, examined substance misuse among 243 individuals receiving treatment for first-episode psychosis in a prospective cohort study. Clients received education and health instruction regarding substance use in a group setting and in a workshop for families. Approximately 85 (35%) clients were diagnosed as having co-occurring substance use disorders (primarily cannabis and alcohol). Alcohol misuse decreased between baseline and three months for clients with an alcohol use disorder but increased by six and 18 months. Drug misuse (primarily cannabis) decreased at three, six, and 18 months. No specific numbers were reported.
Edwards and colleagues (
50), at the Early Psychosis Prevention and Intervention Centre in Melbourne, Victoria, Australia, conducted a single-blind randomized controlled trial of a cognitive-behavioral intervention targeting cannabis use and psychosis among 47 young adults with first-episode psychosis and cannabis use (only half had a diagnosis of cannabis use disorder). Participants were randomly assigned to weekly sessions for three months of cannabis and psychosis therapy (N=23) or to ten individual education presentations (N=24). At the end of treatment and at six months posttreatment, the groups did not differ on cannabis use, but significant proportions in both groups were abstinent (N=10, 43% posttreatment and N=8, 35% at six months for the experimental group versus N=13, 56%, and N=12, 50%, for the control group).
Gleeson and colleagues (
51), also at the Early Psychosis Prevention and Intervention Centre in Melbourne, conducted a randomized controlled trial comparing relapse prevention therapy, a multimodal individual and family cognitive-behavioral therapy for relapse prevention, with standard case management among 82 clients with first-episode psychosis. A majority of the clients had substance use disorders. The substances used primarily included cannabis (N=42, 52%), alcohol (N=20, 25%), amphetamine (N=15, 19%), or hallucinogens (N=12, 15%). Relapse prevention therapy included individual cognitive-behavioral and family educational sessions over seven months and emphasized alcohol and drug abstinence. Clients were reassessed at the end of treatment. Despite an experimental effect on relapse prevention, the groups did not differ on any substance use measures. Overall reductions were not reported.
Kavanagh and colleagues (
52) compared a substance use disorder intervention for inpatients diagnosed as having early psychosis and substance misuse (primarily alcohol and cannabis) in Brisbane, Queensland, Australia. Clients were randomly assigned to the experimental “start over and survive” group (N=13) or to the standard care group (N=12). Start over and survive included three hours of individual substance abuse treatment over six to nine sessions emphasizing motivational interviewing, coping strategies, and problem solving. Standard care included no specific substance abuse treatment. The duration of treatment was seven to ten days because of brief inpatient stays. A majority of clients in both groups became abstinent or reduced all substance use by six weeks and at nearly all follow-ups to 12 months. There were no significant group differences on substance use, but the sample size was small and only eight of 13 clients engaged in start over and survive.
Discussion
Several cohort studies of clients with first-episode psychosis documented significant reductions in alcohol and drug use in the absence of specialized substance abuse treatments. Approximately half of the clients in these studies became abstinent or significantly reduced their use of substances (primarily cannabis and alcohol in all studies). The reductions in use tended to occur rapidly (by six-week follow-up in one study) and to be stable (in most but not all studies). These programs typically provided education and advice to avoid alcohol and drugs to prevent relapses. Some studies found that clients diagnosed as having substance dependence or greater depression at baseline were more vulnerable to persistent substance use disorders, but only a few studies compared those who quit and those who persisted. Another consistent finding was that clients who adopted abstinence reduced their rates of relapse and hospitalization, whereas those with persistent substance use disorders experienced increased rates of relapse and hospitalization.
The few existing studies of specialized substance abuse treatments did not demonstrate substantially better rates of reduction or abstinence. Two cohort studies with specialized treatment for substance use disorders (
48,
49) found reductions in use similar to the nine studies without specialized substance use disorder interventions. Three randomized controlled trials showed no experimental effects of specialized treatment on substance use, but two of the three reported reductions in use that were comparable with the findings of the cohort studies without specialized substance abuse treatments. That is, the finding of early decrease in use occurred in the control as well as the experimental conditions. One explanation of these findings is that a significant proportion of clients who were using or abusing alcohol and other drugs (primarily cannabis) reduced their substance use or became abstinent when they experienced a first episode of psychosis as a result of the traumatic experience of psychosis and the education they received about preventing relapses (
53). It could also be that studies were underpowered to detect differences or that there was a bias toward positive findings in published studies. Finally, it could also be that treatment for psychosis resulted in some reduction in substance abuse through the effectiveness of elements both treatments had in common: assertive outreach, comprehensiveness, long-term perspective, shared decision making, stagewise treatment, and pharmacotherapy (
54). Thus far, the limited research on specialized substance abuse treatments did not show further decreases in substance use.
Treatment should probably proceed in stages (
48). We suggest that specialized interventions be introduced after three or six months of treatment for psychosis for those who continue to use substances and for patients who are dependent on drugs, who experience significant legal or other problems specifically due to substance use, or for whom there is a significant family history of substance abuse.
These findings also highlighted the heterogeneity of studies' diagnostic systems, assessment methods, follow-up period (22 weeks to four years), sample size (from 25 to 643), and recruitment, assessment, and treatment strategies, all of which can influence outcomes. Most of the existing studies had small study groups, recruited participants prior to the natural reductions in use, and did not test interventions in pilot studies prior to conducting randomized controlled trials. The use of different assessment methods and a reliance on self-report suggest that these studies would benefit from more consistent and standardized methodology. Despite this heterogeneity, however, the findings across studies were remarkably consistent.
Because we are still beginning to develop interventions for those who persist in using substances, research should include the standard strategies for developing new interventions: qualitative research, phenomenological studies, attention to the fit of existing interventions, and staged trials (
55). Because studies of specialized substance use disorder interventions for this population are in their infancy, future studies should examine the effects of psychiatric treatment with and without specialized substance abuse treatment on other outcomes in addition to substance use, such as positive and negative symptoms, hospitalization, treatment adherence, social functioning, cognition, and employment. We suggest that researchers include the following elements in their reports: recruitment and participant selection; methods of assessment and their validity; specific substances of abuse (including tobacco) and standardized
DSM-IV or
ICD-10 diagnoses based on structured clinical interview; details on treatments provided, including duration and dose of pharmaceutical treatment and fidelity to psychosocial treatment; description of study dropout and how this was accounted for in the analyses; multiple outcomes, including mental health, substance use, and functional outcomes; and sufficient follow-up periods. Including these elements will facilitate the synthesis of multiple studies into knowledge that can improve outcomes.
Acknowledgments and disclosures
Dr. Wisdom was funded by grant DA020487 from the National Institute on Drug Abuse. The authors thank Mary Brunette, M.D., and Michele Pollock, L.M.S.W., for their assistance.
The authors report no competing interests.