Nonwhite populations have a greater disability burden from depression and anxiety because they are less likely than whites to receive high-quality mental health care (
1–
3). Although racial and ethnic disparities in depression and anxiety care and outcomes may be influenced by patient-level factors, they may also result from lower-quality care being delivered by providers or facilities patronized by nonwhites. We are aware of only one study that examined whether disparities in depression care could be attributed in part to less care being provided by practices that treat mostly nonwhites. Lagomasino and colleagues (
4) found that although Hispanics had lower rates of depression care than whites, these rates did not vary significantly according to whether clinics had low, moderate, or high proportions of Hispanic patients. Analyses were limited, however, to managed primary care clinics in five urban areas and compared only Hispanics and whites. No studies have examined whether disparities in depression care for nonwhites can be explained by the characteristics of practices treating primarily nonwhite patients, such as lack of resources, reimbursement issues, or provider factors.
In other literature on general health, providers and medical facilities have been shown to have an impact on other health disparities. Studies have shown that blacks are more likely than whites to receive cardiac surgery and carotid endarterectomies by less experienced surgeons and in hospitals with higher mortality rates or fewer of such procedures performed (
5–
7); blacks are also more likely than whites to receive treatment in hospitals with worse performance ratings for acute myocardial infarction and pneumonia (
8,
9). Blacks are more likely than whites to be enrolled in health maintenance organizations (HMOs) with low-quality ratings (
5) and to be admitted to low-quality nursing homes (
10). A study on Medicare found that 80% of office visits by blacks were concentrated in 20% of practices and that physicians in these practices were less likely to be board certified and more likely to report difficulties in delivering good-quality care and obtaining necessary tests (
11). On the other hand, a study using data from the National Ambulatory Medical Care Survey (NAMCS) found that although 80% of visits by blacks were clustered in 24% of all practices, physicians delivered the same level of primary care services, regardless of whether they saw a larger or smaller percentage of black patients; however, those who saw a larger percentage of black patients were less likely than those who saw a smaller percentage to refer their patients to specialists (
12).
Policies and interventions aimed at reducing provider- and system-level barriers to providing high-quality care within settings with a high proportion of nonwhite patients could have a substantial impact on reducing disparities (
13,
14). This study examined whether disparities in care for depression and anxiety for both blacks and Hispanics are attributable to providers who see high proportions of nonwhite patients. It also explored whether resource issues (measured as payer mix) account for these disparities. We used NAMCS data that allowed us to examine this relationship in a large sample of primary care and psychiatric providers in nationally representative settings. Our analytical strategy was informed by the Institute of Medicine's definition of disparity (
15) and did not adjust for socioeconomic status, which is a potential mediator of health care disparities. Because providers serving mostly nonwhite clientele may be more likely to encounter cultural patient-provider differences, have numerous competing patient demands, and practice in resource-poor practices, we hypothesized that they will provide less care for depression and anxiety than providers serving mostly white patients. In addition, we expected to find that practices receiving a large proportion of their revenue from public sources (which typically have lower reimbursement rates) will provide less care for depression and anxiety.
Methods
Data source
We used NAMCS data from 2003 to 2007. NAMCS, designed and conducted by the National Center for Health Statistics (NCHS), is a nationally representative sample of office-based physician visits that uses three-stage probability sampling. NAMCS design and execution are described in detail elsewhere (
16). All analyses were performed using the design variables and weights provided by NCHS. Our analyses of treatment outcomes were not limited to visits with a depression or anxiety diagnosis, because a diagnosis may not be documented even if the condition is present and treatment indicated. The UCLA institutional review board approved analyses of deidentified secondary data.
Measures
Outcomes.
Outcomes included received counseling or referral for counseling, antidepressant prescription, and any care for depression or anxiety (antidepressant prescription, counseling or referral for counseling, or both).
The counseling or referral for counseling indicator included counseling provided by the physician or an order for psychotherapy or for mental health or stress management. The antidepressant indicator included any prescription for selective serotonin reuptake inhibitors (SSRIs) (for example, fluoxetine, sertraline, and paroxetine), newer non-SSRI antidepressants (for example, venlafaxine, bupropion, and mirtazapine), tricyclics (for example, amitriptyline, desipramine, and imipramine), other heterocyclics (for example, amoxapine and maprotiline), and monoamine oxidase inhibitors (for example, phenelzine and tranylcypromine). We omitted trazodone because it is used most commonly as a sedative-hypnotic. An indicator for receiving any depression or anxiety care was constructed from the counseling and antidepressant indicators.
Patient visit characteristics.
Race (white, black or African American, Asian, Native Hawaiian or Other Pacific Islander, and American Indian or Alaska Native) and ethnicity (Hispanic or non-Hispanic) were recorded as separate items in the NAMCS data. We derived a race-ethnicity variable with the following categories: white (non-Hispanic), black (non-Hispanic), and Hispanic. Gender was dichotomously coded, and age was measured continuously (with individuals younger than 18 years excluded). A dichotomous variable for presenting complaint of depression or anxiety was derived from the following codes recording reason for visit: anxiety or nervousness (1100.0), fears or phobias (1105.0), depression (1110.0), or obsessions or compulsions (1130.5). A dichotomous variable for a diagnosis of depression or anxiety was similarly constructed, including any ICD-9 codes for depressive disorders (296.2–296.36, 309.1, and 311), anxiety states (300.0, 300.01, 300.02, and 300.09), hysteria (300.10), phobic disorders (300.2–300.23 and 300.29), neurasthenia (300.5), other neurotic disorders (300.8), neurotic depression (300.4), and unspecified neurotic disorders (300.9).
Physician characteristics.
Primary care physicians included doctors of osteopathy and those specializing in internal medicine, general and family practice, and obstetrics and gynecology; the psychiatric specialty included only psychiatrists. Other physician characteristics derived from the data included indicators for solo practitioner (versus other office settings), practice ownership (physician versus HMO, medical or academic, or other hospital or other health care corporation), and high proportion (more than 25%) of practice revenue obtained from Medicare, Medicaid, private insurance, and managed care contracts (one indicator for each of these sources).
Percentage of nonwhite patients.
The percentage of nonwhite patients was estimated from the NAMCS visit data in a manner similar to that used in previous research examining practice composition (
11,
12). First, a dichotomous indicator was created that was coded as 1 for white patients and as 0 for nonwhite patients, and then the mean of this variable was calculated by physician identification code. This number was then subtracted from 1 to obtain the proportion of nonwhite patients, multiplied by 100 to obtain a percentage, and collapsed into quartiles for cross-tabulations: 0%–3.70%, first quartile; 3.71%–11.11%, second quartile; 11.12%–24.24%, third quartile; and 24.25% or more, fourth quartile. Because initial findings noted that physicians in the fourth quartile provided the majority of care for nonwhites, we derived an indicator for “high percentage of nonwhite patients” for visits to physicians in this quartile. This indicator was used instead of the four quartiles because the lower quartiles in psychiatry did not have enough visits by blacks and Hispanics to produce reliable estimates, based on what is recommended by NCHS (at least 30 visits per important category) (
17).
Analyses
We produced cross-tabulations, with Wald statistics and F tests, of characteristics of physician and patient visit characteristics by physician specialty and by whether the physicians saw a high or low percentage of nonwhite patients. We estimated multivariate logistic regressions for our outcomes using SAS software with SUDAAN for the Statistical Analysis of Correlated Data (
18). Logistic regression analyses included survey year and visit characteristics, such as the patient's age, gender, urbanicity of practice (urban versus nonurban), race-ethnicity, and presenting complaint of depression or anxiety. In addition, we included separate indicator variables for whether the visit occurred with a physician who saw a high percentage of nonwhite patients and had a high proportion of practice revenue from Medicare, Medicaid, private insurance, and managed care contracts. We report predicted marginal probabilities to examine differences in treatment patterns according to whether physicians saw a high or low percentage of nonwhite patients, while the analyses controlled for these other visit characteristics. To determine whether whites and nonwhites received similar care from physicians seeing a high percentage of nonwhite patients, we tested interaction terms for race-ethnicity by the indicator for high percentage of nonwhite patients. We found no significant interactions between the visit characteristic of race-ethnicity and practice composition and thus present only the main-effects models below.
Results
Our results revealed that racial-ethnic disparities in depression care persist, especially in primary care, even after the analyses controlled for provider-level characteristics.
Among primary care physicians, 79% of visits by black patients, 83% of visits by Hispanic patients, and 27% of visits by white patients were to providers seeing a high percentage of nonwhite patients; among psychiatrists, 62% of visits by black patients, 69% of visits by Hispanic patients, and 15% of visits by white patients were to providers seeing a high percentage of nonwhites.
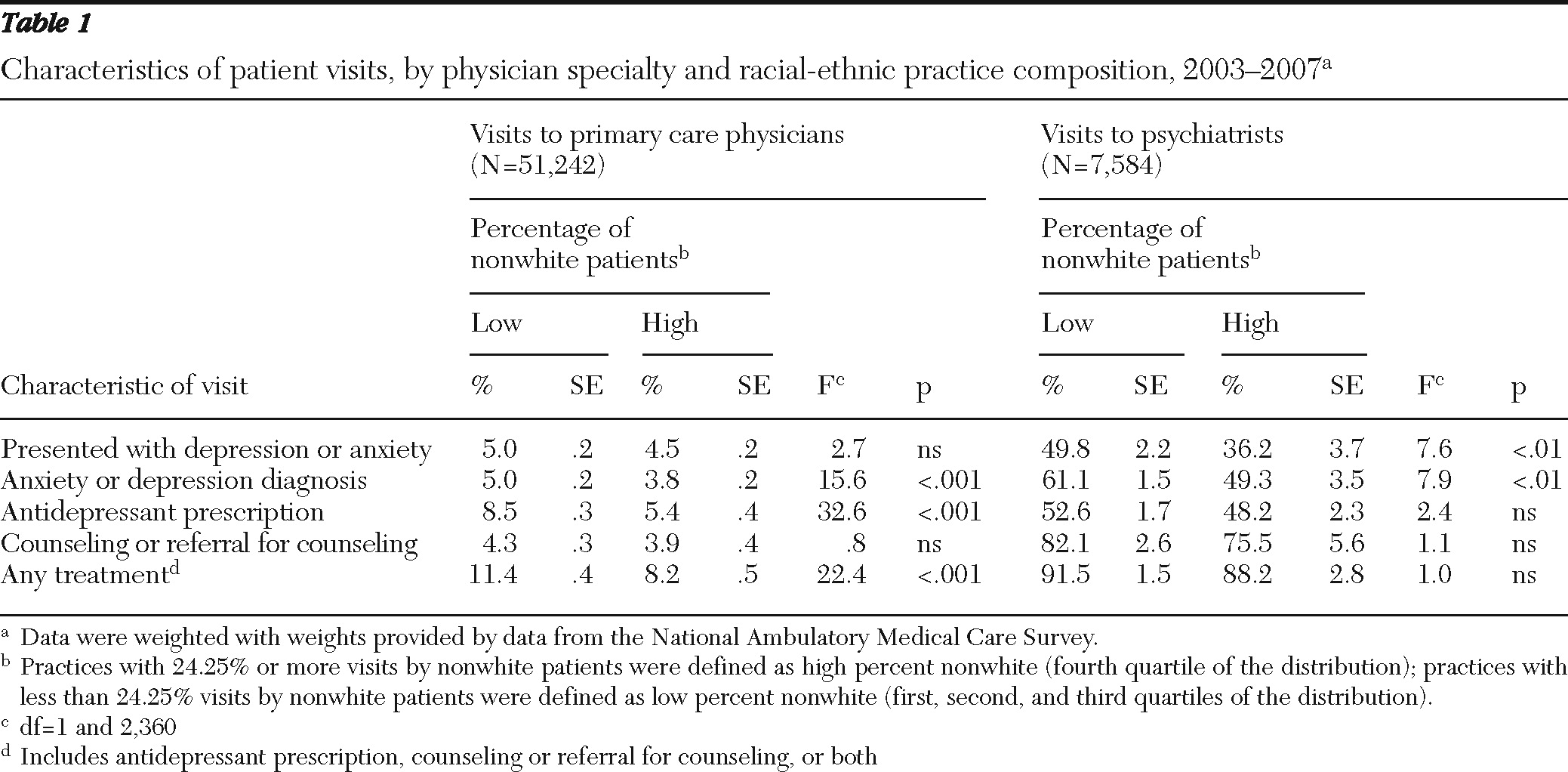
Table 1 presents visit characteristics by physician specialty in settings with a high and low percentage of nonwhite patients. Among primary care physicians, although visits where patients presented with depression or anxiety were similar across settings (high versus low percentage of nonwhite patients), a higher percentage of visits in settings with a low percentage of nonwhite patients resulted in a diagnosis of anxiety or depression, antidepressant prescription, or any care for depression or anxiety. Among psychiatrists, visits in settings with a low percentage of nonwhite patients were more likely to have patients who presented with and were diagnosed as having depression or anxiety.
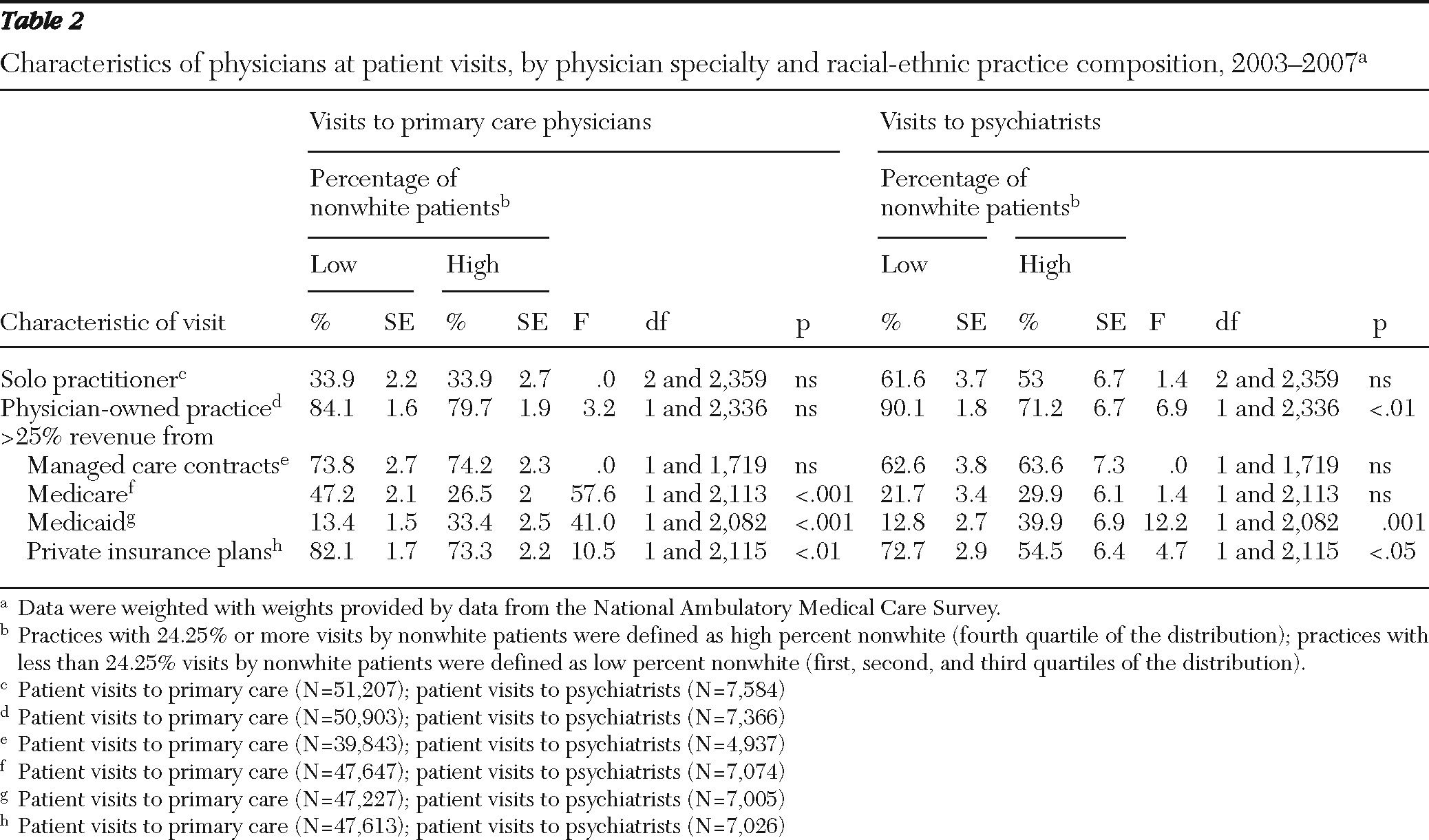
Table 2 shows physician visit characteristics by physician specialty and racial-ethnic practice composition. In primary care, compared with providers seeing a low percentage of nonwhite patients, those seeing a high percentage of nonwhite patients were less likely to have a high proportion of revenue from Medicare and private insurance plans and more likely to have a high proportion of revenue from Medicaid. Among psychiatrists, those seeing a high percentage of nonwhite patients were less likely to have a physician-owned practice and less likely to have a high proportion of revenue from private insurance plans; they were more likely to have a high proportion of revenue from Medicaid.
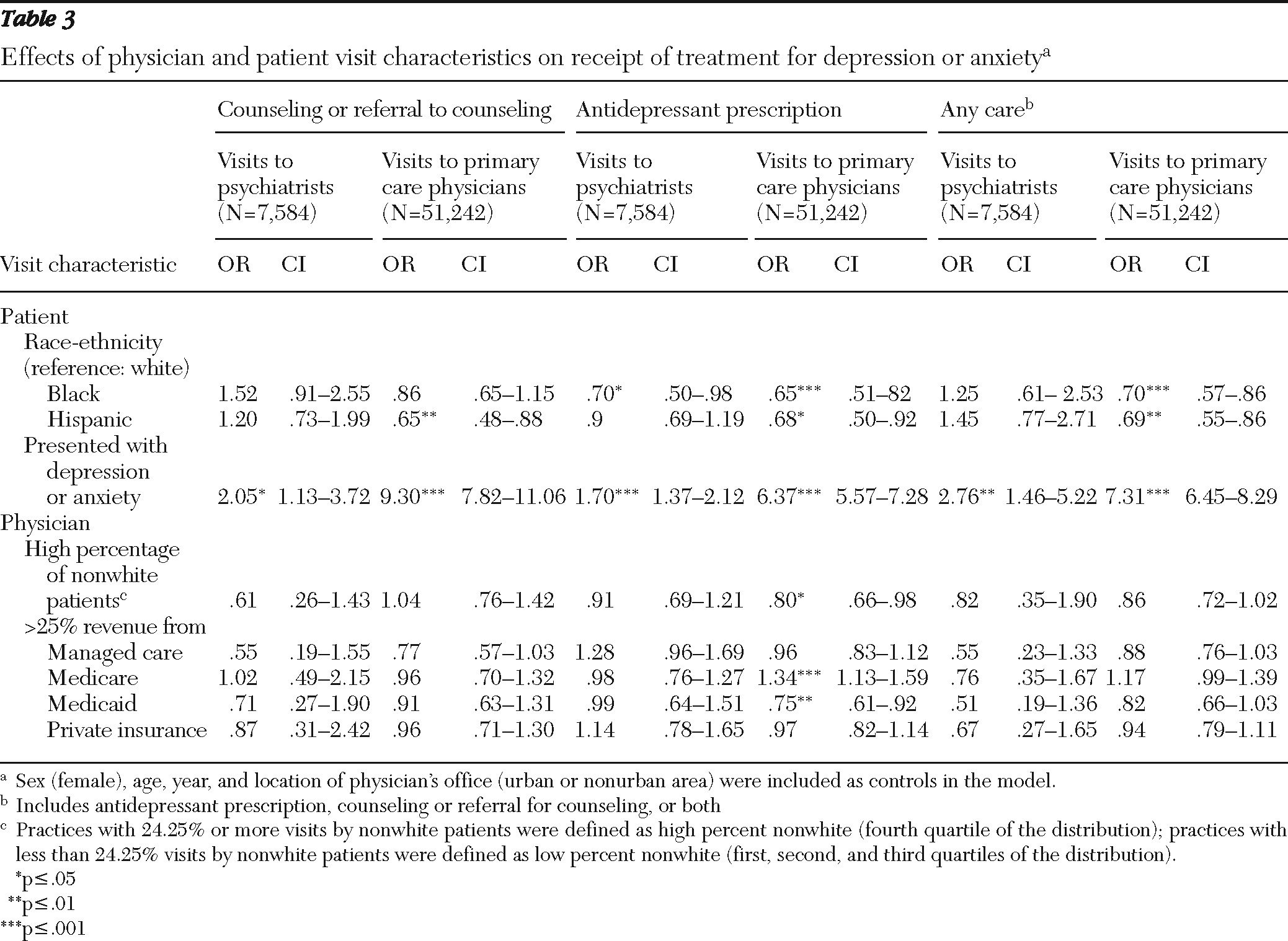
As shown in
Table 3, multivariate logistic regression models revealed persistent racial-ethnic disparities among primary care physicians after controlling for provider and practice characteristics. Compared with visits by white patients, visits by black patients were found to be less likely to result in receipt of antidepressants in either primary care or psychiatric settings and to result in receipt of any care in primary care settings. Primary care visits by Hispanic patients were less likely than those by white patients to result in receipt of counseling, antidepressants, or any care. The overall group effect for the visit characteristic of race-ethnicity was statistically significant only for any care in primary care (
χ2=9.31, df=2, p<.001). Having depression or anxiety as the presenting complaint significantly increased the odds of getting counseling, antidepressants, or any care in both psychiatric and primary care settings.
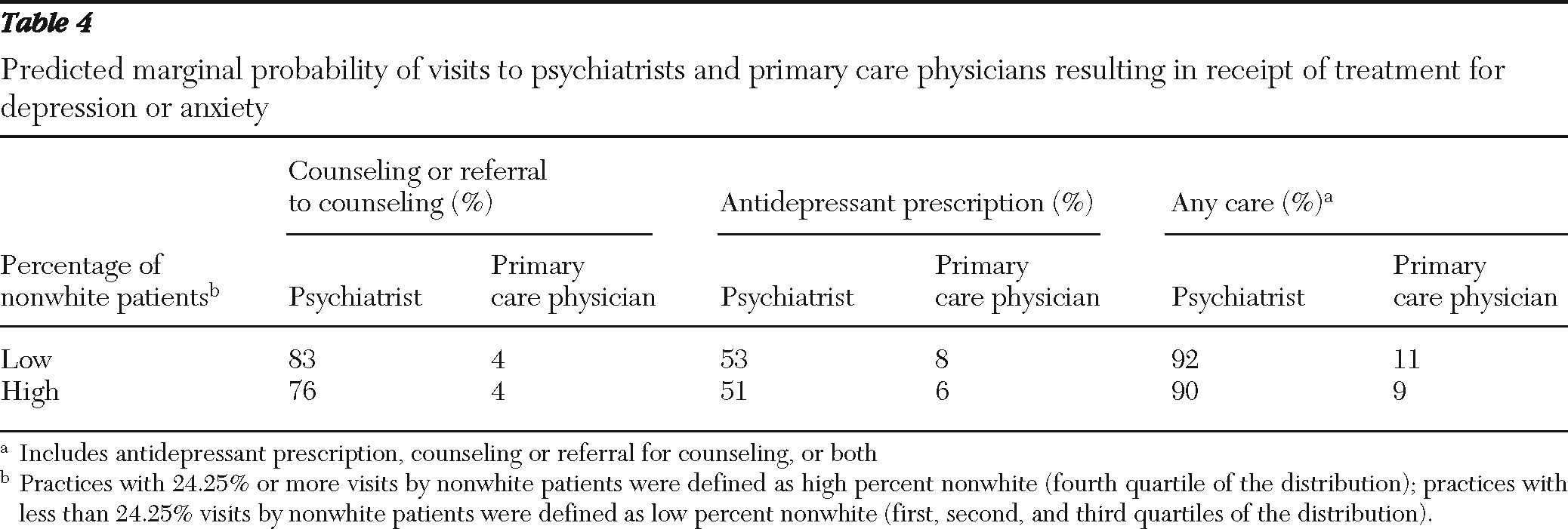
Logistic regression models examined whether these disparities in care might be accounted for by persons from racial and ethnic minority groups frequenting clinics with a high percentage of nonwhite patients. This variable was significant only in predicting lower rates of antidepressant prescriptions in primary care settings. The marginal predicted probability of receiving antidepressant prescriptions during visits to primary care settings with a high percentage of nonwhite patients was 6%, compared with 8% during visits to primary care settings with a low percentage of nonwhite patients (
Table 4). Visits to providers seeing a high percentage of nonwhite patients and with a high proportion of revenue from Medicaid were less likely than those to providers seeing a low percentage of nonwhite patients and those with a low proportion of revenue from Medicaid to result in receipt of antidepressants, whereas visits to providers with a high proportion of revenue from Medicare were more likely than those to providers with a low proportion of revenue from Medicare to result in receipt of antidepressants. Notably, disparities in antidepressant prescriptions remained even after the analyses adjusted for all of these variables.
Sensitivity analyses.
We conducted a series of sensitivity analyses to determine whether the disparities we found could be explained by such factors as use of anxiolytic medications other than antidepressants. Although antidepressants are recommended first-line treatments for anxiety, other anxiolytics (including benzodiazepines and buspirone) may be prescribed. However, alternative models for outcomes that included anxiolytic prescriptions were not substantively different.
We also examined whether insurance status accounted for the differences we found, and we examined whether treatment disparities exist because physicians who see a high percentage of nonwhite patients might see more patients with more medical problems and thus have competing demands for time. We created two proxy variables for competing demands by summing number of reasons for visit and number of medications prescribed at the visit. Although insurance and competing medical demands were statistically significant predictors of receipt of depression care, the findings by race-ethnicity and by whether physicians saw a high percentage of nonwhite patients did not change substantively when these variables were included.
Finally, because black and Hispanic patients are particularly underrepresented in psychiatric settings, one explanation for differences in depression care could be that the few nonwhite patients presenting to psychiatric settings are being treated for more severe affective or psychotic disorders. We included an indicator for psychotic symptoms as the recorded presenting complaint in the models for depression and anxiety treatment in psychiatry. We found no substantive differences in results by race-ethnicity or percentage of visits by nonwhite patients with this indicator in the model.
Discussion
These results offer further understanding of disparities in depression and anxiety care. Over the study period, disparities in depression care continued to exist primarily in primary care settings. In these settings, compared with visits by whites, visits by black and Hispanic patients were less likely to result in receipt of antidepressants or any care, and visits by Hispanics were less likely to result in receipt of counseling. In psychiatric settings, visits by black patients were less likely than those by white patients to result in receipt of antidepressants. Black and Hispanic patients were mostly served by providers who see a high proportion of nonwhite patients. However, the racial-ethnic composition of practices and resources (insurance composition) were significant factors only in predicting less antidepressant prescriptions in primary care and did not fully account for the treatment differences observed. This is fairly consistent with the earlier study in this area that found that disparities in care could not be accounted for by site of care (
4).
These results suggest that physician bias and resources issues may play a somewhat limited role in whether depression is diagnosed and treated. Especially with regard to antidepressant treatments, primary care clinics serving primarily nonwhites may have provider-, organizational-, or system-level barriers to providing high-quality care. For example, they may have fewer resources for more patients; their funding may be public; their jobs may be less desirable; their physicians may be less well trained, more transient, or trainees; and their physicians may be more likely to be international medical school graduates and may not have either English or Spanish as their first language. However, racial-ethnic disparities remained after analyses controlled for practice characteristics, suggesting that physician bias, patient preferences, or both could also play a role in lower rates of treatment. Patients from racial or ethnic minority groups may be less likely than whites to accept antidepressant medication treatment. Prior work has shown that both blacks and Hispanics prefer to receive counseling to medication (
19) and that blacks and Hispanics are less likely than whites to receive antidepressant treatment, even though primary care providers recommended antidepressant treatments equally to whites and nonwhites (
20). Our study found that Hispanics were also less likely than whites to receive counseling or referral for counseling.
Our findings have important implications for reducing disparities for black and Hispanic patients, particularly in primary care settings, where these patients are most likely to seek mental health care. Efforts to improve care in these settings may require ensuring adequate resources and prescription insurance coverage for patients from racial or ethnic minority groups, reducing physician bias in decision making concerning depression care, and providing patients with education regarding effective treatments. The American Psychiatric Association's workgroup on disparities has put into operation some of the broad recommendations in the Surgeon General's report on mental health for racial and ethnic minority groups (
1), but more is needed to institute accountability mechanisms at a system level. Policy interventions by professional and regulatory bodies and federal agencies are needed to adequately address disparities (
13). In addition to changes in medical education and training, reducing physician bias may also require changes in the conditions under which decision making occurs—that is, fatigue, overload, and time pressure, all of which are more prevalent in practices with high proportions of nonwhite patients (
14).
Although NAMCS data were particularly effective for examining whether patients or physicians might contribute to racial or ethnic disparities in mental health care, a few limitations should be mentioned. First, the data are based on physician or physician office staff reports, which may affect causal validity. For example, reports of the presenting complaint may be influenced by the treatment prescribed for the patient; thus the causal direction of the relationship between these two variables may be the opposite of what our model represents. Because our primary focus in these analyses was the effect of racial-ethnic practice composition, it is unlikely that reverse causation between presenting complaint and treatment outcome would affect our conclusions about patient race-ethnicity or practice composition. Second, nonwhites with depression or anxiety could be more likely than whites with these disorders to seek care for them from a primary care provider rather than from a psychiatrist. We found higher rates of treatment for visits to these settings; however, we do not believe selection effects can explain our results.
Furthermore, we had no information on severity of depression or anxiety or the dosage or duration of medications or counseling. We were also unable to examine the affect of patient socioeconomic status or language preference, because NAMCS does not collect this information. NAMCS data do not allow us to examine separately whether physicians were equally likely to refer white and nonwhite patients to counseling; the data allowed us to determine only whether patients received counseling or referral for counseling at the visit. Thus we were unable to rule out patient preferences (and other important patient-level factors) as a factor in disparities in antidepressant treatment. Additionally, the method of determining patient race and ethnicity could vary across doctors' offices, which may affect reliability of this variable; however, no studies that we are aware of have examined the reliability of the NAMCS race and ethnicity variables. Finally, these analyses are representative of only nonfederal office-based visits to primary care and psychiatric settings.
Conclusions
More research is necessary to determine the specific mechanisms by which patient race-ethnicity and racial-ethnic composition of practices contribute to lower rates of treatment for depression and anxiety. In addition to physician bias and practice resource issues, patient preferences could play a role in disparities in treatment for depression and anxiety. Barriers to care at the patient, physician, and system levels need further exploration. These barriers may be as diverse as increased concerns about stigma on the part of nonwhite patients, physicians' discomfort in interacting with nonwhite patients, clinical uncertainty associated with differential interpretation of symptoms, the physician-patient interaction, limited practice resources and many competing demands in public-sector settings, and the accumulated effects of a lifetime of structural inequality (
21–
25).
Acknowledgments and disclosures
This research was supported by grants from the John D. and Catherine T. MacArthur Foundation, grant 3P03-AG-021684-06 from the National Institute on Aging, grant NIH/2P20-MD-000182-06 from the National Center for Minority Health and Health Disparities, and grant P30-MH-082760-01 from the National Institute for Mental Health. The authors thank Lingqi Tang, Ph.D., and Lily Zhang, M.A., for their excellent help with programming statistical analyses.
The authors report no competing interests.