Posttraumatic stress disorder (PTSD) co-occurs with a wide variety of psychiatric disorders. The most common of these disorders are substance abuse, anxiety, and depression
(1, 2). However, there has been increasing attention to the concomitant physical symptoms that may accompany trauma
(3–5; unpublished data of J.C. Beckham et al). In one study
(4), firefighters with PTSD were more likely to report cardiovascular, respiratory, musculoskeletal, and neurological problems than firefighters who did not develop PTSD and who were exposed to the same trauma. In a comparison of PTSD patients who did and did not report physical symptoms, PTSD patients with physical complaints reported higher overall PTSD symptoms and a greater frequency of major depression
(4). In the DSM-IV field trials, a high level of association among trauma, affective dysregulation, dissociation, and somatization was detected
(5). However, since all of these studies used self-report measures of health, it is unknown whether observed differences in physical symptoms are solely the result of self-report bias.
Vietnam veterans with combat-related PTSD report more current and chronic health problems than combat veterans without PTSD
(3). PTSD severity is associated with greater cardiovascular morbidity
(3), and greater severity of PTSD has been associated with more health complaints regardless of comorbid psychiatric symptoms (J.C. Beckham et al., unpublished data). Rated discharge summaries of Vietnam veteran inpatients treated for PTSD report a high rate of medical problems
(6). However, the reliability of the ratings and rates of medical disorders in a comparison group were not evaluated. In the two studies of veterans with and without PTSD, which employed medical examination, no differences in physical health status were detected between Vietnam and non-Vietnam veterans
(7) or Israeli veterans and matched comparison subjects
(8).
Several hypotheses have been generated to account for the discrepancy between medical health data and veteran self-reported health. These include the following: veterans may exaggerate their symptoms
(9), precursors of poorer health outcomes associated with PTSD have not been measured
(3), and greater somatization is part of the sequelae of chronic, complex PTSD
(5).
Several decades of research experience conducting the National Health Interview Surveys and the Health Interview Evaluation Surveys in the general population suggest that use of general disease categories based on self-report may result in slightly overreported medical conditions. However, this was not true for specific medical conditions. Recent Health Interview Evaluation Survey research indicates that conditions requiring a physician’s diagnosis and those requiring ongoing care had the highest level of agreement between the interview and medical record
(10). These findings underscore the importance of collecting both self-reported and physician-rated data in the assessment of health status and the unique contribution of physician ratings of health conditions.
The primary purpose of the current study was to evaluate physician-rated as well as self-reported health problems in veterans with and without PTSD. The secondary purpose was to assess factors that are associated with severity of health problems in PTSD patients. We formulated two a priori hypotheses: 1) Vietnam combat veterans with PTSD will have poorer health status according to both self-report and physician ratings, and 2) somatization and PTSD symptom severity will be related to health problems in Vietnam combat veterans with PTSD.
METHOD
Subjects
The study groups were 276 help-seeking male combat veterans from a Veterans Affairs (VA) Medical Center PTSD Clinical Team diagnosed with PTSD and 51 who were diagnosed as not having PTSD. All patients completed all information as part of their clinic evaluation. Those diagnosed with combat-related PTSD scored higher than 0 on the Combat Exposure Scale
(11) and were rated by clinicians as having PTSD on the basis of the Clinician-Administered PTSD Scale
(12) (kappa coefficient=0.98). To qualify as a combat veteran without PTSD, the veteran had to have a score higher than 0 on the Combat Exposure Scale and be rated by a clinician as not meeting PTSD criteria. Socioeconomic status was rated with the Hollingshead scale
(13). Patients were also administered the Mississippi Scale for Combat-Related Posttraumatic Stress Disorder
(14).
Measures
Self-reported health measure
In the self-report measure used in the National Vietnam Veterans Readjustment Study
(2), patients are presented with two dichotomous rating checklists (0=no, 1=yes). The first is a 22-item symptom list (e.g., diarrhea, muscle aches). The second contains 37 chronic health problems, and the veteran rates these conditions both for lifetime and past year occurrence. Three scores result: total health complaints, lifetime physical conditions, and current physical conditions. Physical conditions in the past year were coded on the basis of categories (e.g., cardiovascular) in The Merck Manual of Diagnosis and Therapy
(15) in order to compare patient report to physician rating. Pack-year history was calculated on the basis of average number of cigarettes a day times the years smoked divided by 20
(10). Alcohol problems were measured by the CAGE questionnaire (16) and the MacAndrew alcoholism supplementary scale of the MMPI-2
(17). CAGE scores range from 0 to 4; scores of 2 or higher are used to indicate a likely alcohol disorder
(16). The CAGE was used to rate alcohol problems both in the past month and over the subject’s lifetime. MacAndrew alcoholism scale scores range from 0 to 51. We used the most stringent recommended cutoff score, 28 or higher, to indicate the presence of an alcohol disorder
(17). Studies suggest that the MacAndrew alcoholism scale is a more general measure of substance abuse, which includes alcohol as well as other drugs
(17).
Medical chart review
VA medical charts were reviewed for the number and type of physician-diagnosed disorders. Each disorder was categorized through use of the Merck manual (e.g., cardiovascular, gastrointestinal, hematology, genitourinary, pulmonary, musculoskeletal, immunology, metabolic, dermatological, and other). Ratings were completed by a PTSD clinic physician who was not involved in the patients’ medical or psychiatric care and who was blind to PTSD diagnostic status. The ratings resulted in two scores: total number of categories and total number of illnesses. Reliability was calculated with 50 randomly selected charts rated by a second rater, resulting in a kappa coefficient of 0.85.
Davidson Trauma Scale
The Davidson Trauma Scale is a 17-item, 5-point self-rated scale that assesses frequency and severity of each DSM-IV PTSD symptom
(18). The scale was developed with rape, combat, natural disaster, and other trauma populations and has high reliability and validity
(18).
Somatization
The MMPI-2 hypochondriasis scale, which was used as a measure of somatization, includes items designed to assess a general overconcern with bodily function. The scale does not distinguish actual from imagined physical difficulties
(17).
Beck Depression Inventory
The Beck inventory, a 21-item, forced-choice scale, is a reliable and valid measure of general depression symptoms
(19). The cutoff scores for the presence of a depressive disorder are well validated against clinician interviews
(19).
RESULTS
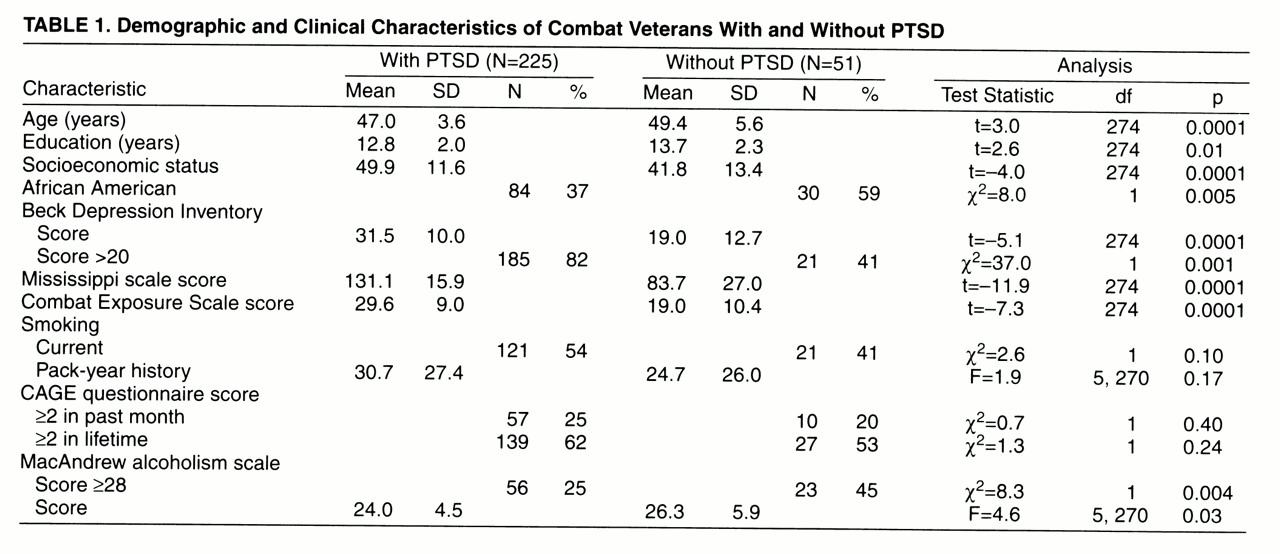
Descriptive data for the two study groups are presented in
table 1. Mean age and years of education were significantly lower in veterans with PTSD than in those without PTSD. Veterans with and without PTSD were of similar pack-year history, current smoking status, and CAGE scores. PTSD veterans were of lower mean socioeconomic status (lower middle class) than those without PTSD (middle class) and were less likely to be of African American ethnicity. Veterans with PTSD had higher mean combat exposure scores (moderate to heavy) than combat veterans without PTSD (moderate) and higher Mississippi scale scores. Mean Mississippi scale scores were above the recommended cutoff for PTSD (higher than 107) in the PTSD group and below the cutoff (lower than 90) in the group without PTSD
(14). PTSD patients had higher Beck inventory scores than patients without PTSD. An analysis of covariance (ANCOVA), which controlled for age, socioeconomic status, minority status, and combat exposure, indicated no significant difference between groups for pack-year history and a significant difference on MacAndrew alcoholism scale scores. Non-PTSD patients had significantly higher MacAndrew alcoholism scale scores. Of the non-PTSD group, 42% scored in the clinically depressed range on the Beck inventory, and nearly half scored above the cutoff on the MacAndrew alcoholism scale, indicating the presence of an alcohol disorder.
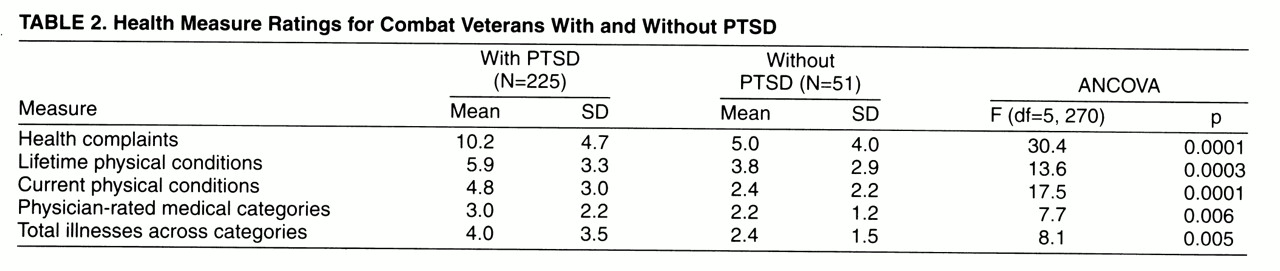
Hypothesis 1: Combat Veterans With PTSD Will Have Poorer Health Status Than Combat Veterans Without PTSD
Ninety-four percent of the non-PTSD patients and 90% of the PTSD patients were rated as having at least one health problem, and 75% of each group were rated as having multiple medical problems. Health measure ratings are shown in
table 2. Age, socioeconomic status, minority status, combat exposure, pack-year history, and MacAndrew alcoholism scale scores were used as covariates in ANCOVAs. Separate ANCOVAs were conducted to compare self-reported and physician-rated health status in combat veterans with and without PTSD. Compared to veterans without PTSD, veterans with PTSD had higher ratings on all health status measures. Pack-year history was significant for total health complaints, lifetime physical conditions, and current physical conditions. MacAndrew alcoholism scale scores were significant for lifetime health complaints. No other covariates were significant in the models.
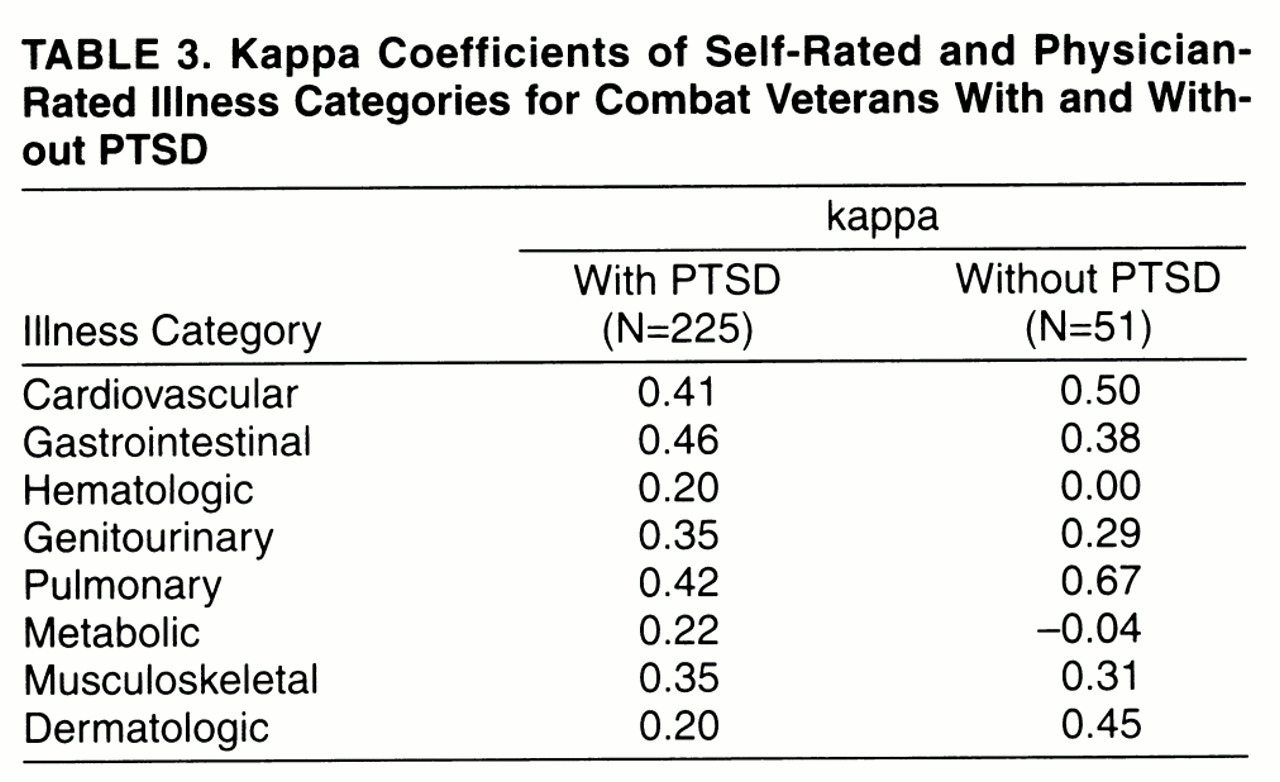
In order to evaluate the rate of agreement between patient and physician reports, kappa coefficients were calculated for each category by group
(20). These are presented in
table 3. The range for the coefficients was very low to moderate, and no significant differences across groups in kappa coefficients were detected.
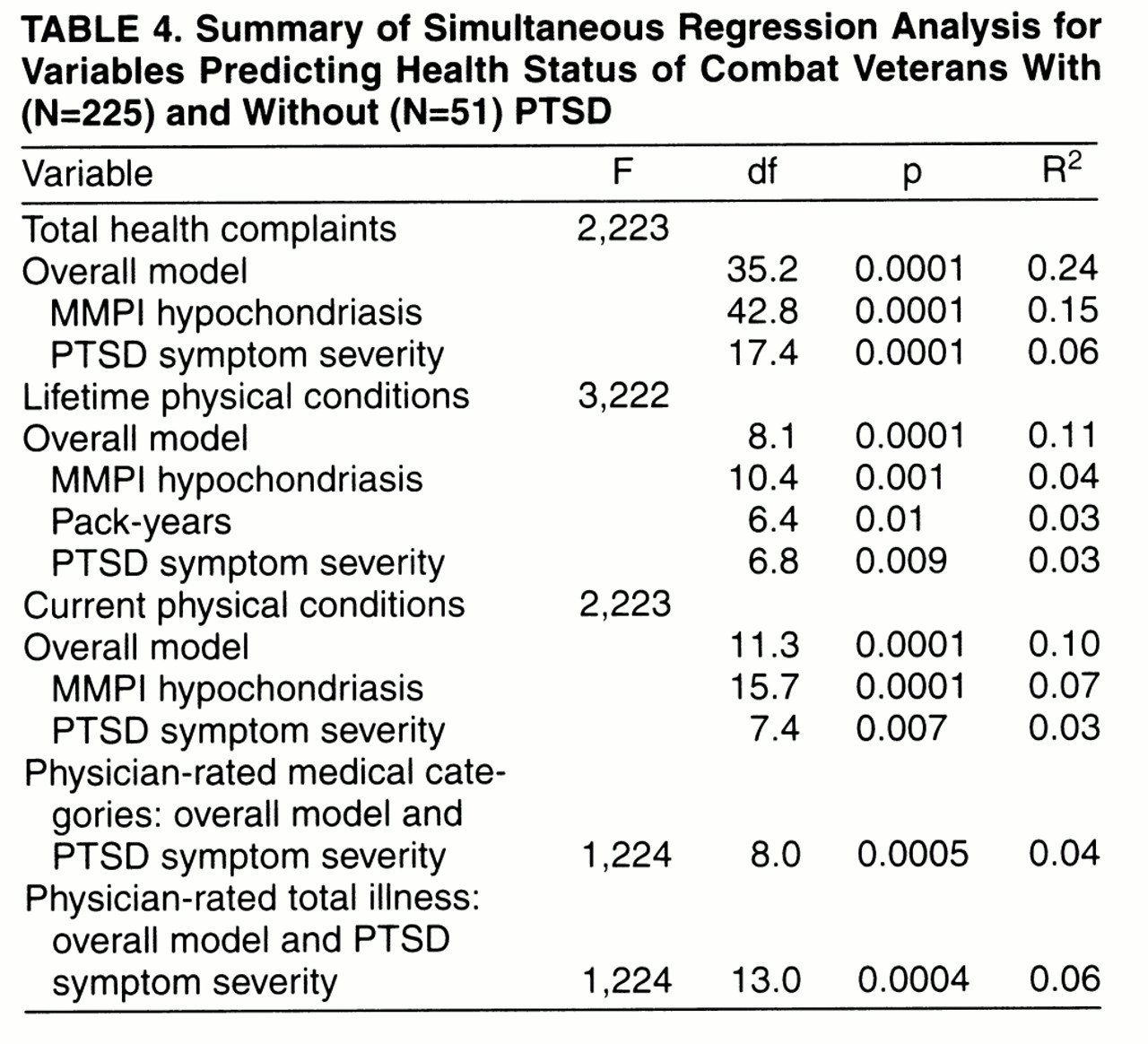
Hypothesis 2: Health Status Will Be Related to Somatization and PTSD Symptom Severity in Combat Veterans With PTSD
In part 2 of the study, multiple regression analyses (21) were used to examine the relationship between the dependent variables (health status measures) and the independent variables (age, combat exposure, socioeconomic status, pack-year history, MacAndrew alcoholism scale scores, depression, hypochondriasis, and PTSD symptom severity). Separate regression models were conducted for each health status measure, and the independent variables were entered in a simultaneous model. Results are presented in
table 4. Hypochondriasis was significant for self-reported health measures. Total PTSD severity was significant for both self-reported and physician-rated health variables. Pack-year history was significant for self-reported lifetime physical conditions. No other variables were significant in the models.
DISCUSSION
The results of this study indicated that when age, socioeconomic status, minority status, combat exposure, and pack-year history were controlled, combat veterans with PTSD reported and were rated as having a greater number of health problems than combat veterans without PTSD. Pack-year history was related to patient report of a greater number of health complaints and current and lifetime physical conditions. MacAndrew alcoholism scale scores were related to lifetime health complaints. Although almost all patients across groups were rated as having at least one chronic medical condition, PTSD patients (compared to non-PTSD patients) were rated as having a greater number of total illnesses across a wider number of medical categories. The rate of agreement between patient and physician for the presence of physical conditions across groups ranged from low to moderate; neither patient group was very accurate. When the physician rating of medical charts was used as the standard, patients were relatively more accurate at reporting cardiovascular and pulmonary conditions. In examining variables related to health measures in PTSD patients, we found that hypochondriasis was most strongly related to self-reported health measures. PTSD symptom severity was significantly related to both self-reported and physician ratings of health.
Rate of self-reported current physical health problems was higher than rates reported in the National Vietnam Veterans Readjustment Study
(2) for combat veterans with PTSD (4.8 versus 2.4) and without PTSD (2.4 versus 1.1), and rate of physical health problems in PTSD patients (94%) was higher than that in a previous report
(6) of PTSD patients being treated for PTSD (60%). These higher rates could be due to differences in age at the time of sampling, measurement method, or help-seeking status. PTSD symptom severity was related to both self-reported and physician-rated health, indicating that those with more severe PTSD symptoms also had more health problems.
Both veteran groups had a smoking rate that was nearly two times that of a temporally comparable male population estimate of 25%, derived from national survey data
(22). Pack-year history was similar across groups and was a significant predictor of self-reported health in both patient groups. Score on a general measure of substance abuse (MacAndrew alcoholism scale) was significant for lifetime health complaints.
Somatization was significant for all measures of self-reported health in the PTSD patients. It has been hypothesized that as part of their PTSD, PTSD patients have difficulty determining the salience of information and that this deficit in information processing may contribute to a patient’s focus on and misinterpretation of somatic sensations
(4, 5, 23).
The lack of significance in depression level for health measures in PTSD patients is inconsistent with a previous finding that the presence of a major depression diagnosis was more frequent in PTSD patients who reported physical symptoms
(4). In examining the rate of depression in the current PTSD study group, we found that 83% of the patients had Beck inventory scores greater than or equal to those of patients who are clinically depressed (i.e., scores of 21 or higher). This high rate of depressive symptoms is consistent with previous research (J.C. Beckham et al., unpublished data), but because of a high level of depressive symptoms, there simply may have been too little variability for depression to be a discriminating variable.
There are limitations to the results of this study. The study design is correlational and therefore cannot indicate that PTSD causes greater health problems. The results of this study may be confounded by the presence of comorbid disorders. Exposure to trauma other than combat was unassessed. Results of the study can be generalized only to help-seeking combat veterans with and without chronic PTSD.
Nonetheless, regardless of etiology, comorbidity, or phenomenology, the results of the current study add veracity to previous studies that found an association between PTSD and health by using physician ratings of health status. The results of the current study extend previous findings by documenting that severity of PTSD was associated with poorer health status. Addressing the physical health effects of PTSD awaits further study.