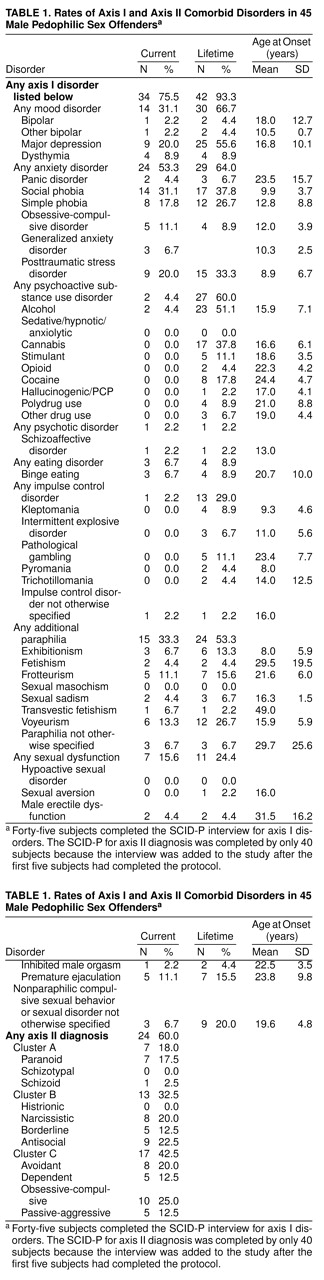
The most remarkable finding in this study is that 93% (N=42) of the subjects met the criteria for some axis I diagnosis in addition to pedophilia over the course of their lifetime. Only three subjects had pedophilia as their only psychiatric diagnosis. These data support the view that attention to the diagnosis and treatment of comorbid psychiatric disorders is essential to the treatment of this population. Diagnosis on all five of the DSM-IV axes should be assessed during the evaluation and treatment of pedophilic sex offenders.
Mood and anxiety disorders were the most common disorders in our population. The presence of these disorders could make it difficult for patients to respond effectively to the rigors of sex offender treatment, which often uses confrontational group therapy and cognitive behavioral therapy approaches. The same could be said for the personality disorders that were common in these subjects (i.e., obsessive-compulsive, antisocial, avoidant, narcissistic, and paranoid personality disorders). Personality disorders, particularly antisocial personality disorder, have been offered as an explanation for pedophilic behavior, even though the literature has not supported this position
(2). It is important to note that in our group, 77.5% of the subjects (N=31) did not meet the criteria for antisocial personality disorder, and 80% (N=32) did not meet the criteria for narcissistic personality disorder. Previous authors have reported higher-than-expected rates of alcoholism and alcohol abuse in child molesters (reviewed in reference
4). In our population of pedophiles, 51% (N=23) met the criteria for a lifetime history of alcohol use disorder, and 44% (N=20) met the criteria for a substance use disorder other than alcohol. Thirty-three percent of this group of pedophiles (N=15) met the criteria for at least one other paraphilic diagnosis. With regard to exhibitionism, frotteurism, and voyeurism, we made these diagnoses even if the focus of these behaviors was directed primarily at children. We used a liberal interpretation of this statement in DSM-IV: “if the individual’s sexual preferences meet criteria for more than one paraphilia, all can be diagnosed” (p. 525). Future studies could focus more on the details of the differential diagnosis of these disorders. Lack of progress in treatment is often attributed to poor motivation, inattentiveness, resistance, and denial. In light of the findings presented here, it seems likely that unrecognized psychiatric conditions contribute to the difficulties that individuals face when they try to engage in the process of therapy and in completing therapeutic tasks. These findings call for taking comorbid disorders into consideration when individualizing treatment within sex offender treatment programs and for the appropriate use of pharmacotherapy in addition to psychotherapy. It seems reasonable to assume that sex offenders would benefit from the treatment of comorbid psychiatric disorders and the appropriate use of pharmacotherapy.