In DSM-IV, rapid cycling is defined as the occurrence of at least four major depressive, manic, hypomanic, or mixed episodes during the previous year, demarcated either by a remission of at least 2 months’ duration or by a switch to an episode of opposite polarity. Duration criteria for affective episodes are not waived: each major depressive episode must last at least 2 weeks, each manic or mixed episode at least 1 week, and each hypomanic episode at least 4 days.
This definition, although consistent with the one originally proposed by Dunner and Fieve
(1), is different from those adopted in most empirical studies on rapid cycling carried out to date. In fact, both Koukopoulos and Reginaldi
(2) and Wehr et al.
(3) waived duration criteria for affective episodes and required a circular course (i.e., a direct transition from mania or hypomania to depression or vice versa) at some time in the history of illness. Coryell et al.
(4) waived duration criteria for affective episodes and required at least four episodes during 1 year of prospective follow-up, demarcated by at least 2 weeks (instead of 2 months) of remission or by a switch to the opposite polarity. Bauer et al.
(5) required at least four affective episodes during any 1-year period in the past, demarcated by “a period of euthymia lasting at least as long as the proximate episodes” or by a switch to the opposite polarity. Maj et al.
(6) adopted a definition based on the Research Diagnostic Criteria, which was consistent with the one in DSM-IV except for the minimum duration of hypomanic episodes (1 week rather than 4 days).
An analysis of the results of the above-mentioned studies shows that the different definitions of rapid cycling have important clinical implications. In particular, the two studies in which circularity of course was a prerequisite
(2,
3) found rapid cycling to be a relatively stable pattern on follow-up, whereas the other three studies
(4–
6) found it to be very unstable over time. The difference is particularly striking if one compares the studies by Wehr et al.
(3) and Coryell et al.
(4), which are those with the longest follow-up. In the former study, 41% of patients retained the rapid-cycling pattern throughout a follow-up that averaged 5 years, whereas in the latter, only 2.6% of patients retained the pattern throughout a 4-year follow-up. On the other hand, a significantly higher proportion of bipolar II disorder among rapid-cycling patients than among nonrapid-cycling patients was reported by both Koukopoulos and Reginaldi
(2) and Coryell et al.
(4), who waived duration criteria for affective episodes, whereas this was not found by Bauer et al.
(5) and Maj et al.
(6), who did not waive those criteria. Thus, the DSM-IV definition may identify a group of patients who are meaningfully different from those enrolled in most available empirical studies on rapid cycling, and it may exclude those patients in whom the rapid-cycling pattern is most stable, who are likely to be the least responsive to currently available therapies.
The definition of rapid cycling finally adopted in DSM-IV was not the only one considered by the DSM-IV Mood Disorders Work Group. Actually, in an early report
(7), that group recommended the inclusion of “truncated episodes” (i.e., those meeting severity criteria but not duration criteria for an episode of mania, hypomania, or major depression) in the definition of rapid cycling, whereas in a more recent report
(8), the group noted that the inclusion of subjects with truncated episodes did not alter the validators (i.e., predominance of female patients and bipolar II pattern) and concluded that the decision whether to include these subjects had to be based on “issues of practicality.” In a related article
(9), consideration was given to the possibility of including truncated episodes but requiring that patients be fully symptomatic for at least 8 weeks during the reference year, in order to avoid the risk of including subjects who had been ill for just a few days. This option, however, has never been assessed systematically.
The present study aimed to address the issue of the reliability and validity of four alternative definitions of rapid cycling in a large group of patients with bipolar disorder. We tested definitions that 1) counted only full affective episodes, 2) simply waived duration criteria, 3) waived duration criteria and required a switch in polarity, and 4) waived duration criteria and required that patients be fully symptomatic for at least 8 weeks during the reference year.
METHOD
The study was carried out with 210 consecutive patients (101 male and 109 female; mean age=39.1 years, SD=8.9, range=17–71) who were attending the Center for Affective Disorders at the First Faculty of Medicine of the University of Naples. The patients met the Research Diagnostic Criteria (RDC)
(10) for bipolar disorder as ascertained by the Schedule for Affective Disorders and Schizophrenia (SADS)
(11), independently administered to each patient by two trained psychiatrists (M.M. and R.P.). The study included only patients for whom a consensus on the diagnosis of bipolar disorder could be reached by the two psychiatrists. Written informed consent was obtained from all subjects after the study procedure had been fully explained.
On the basis of the information collected by the structured interview, integrated with some additional questions concerning affective morbidity during the past year, the two assessors independently checked whether each patient met the following alternative definitions of rapid cycling: 1) at least four major depressive, manic, or hypomanic episodes, as defined by the RDC, during the previous year, demarcated by a euthymic period of at least 8 weeks or by a switch to an episode of opposite polarity (a euthymic period was defined by the absence of the mood disturbance required by RDC criterion A for major depression, mania, or hypomania and by the presence of no more than two of the symptoms required by RDC criterion B for major depression); 2) the same as definition 1, but including all major depressive, manic, or hypomanic episodes meeting RDC severity criteria and lasting at least 1 day; 3) the same as definition 2, but with the requirement of at least one direct transition from mania or hypomania to major depression or vice versa during the previous year; and 4) the same as definition 2, but with the requirement of a total duration of at least 8 weeks of fully symptomatic affective illness during the previous year. The interrater reliability for the application of each definition was assessed by Cohen’s kappa statistic.
Patients for whom there was agreement between the two psychiatrists about their meeting one of the above-mentioned definitions constituted four partially overlapping groups of rapid-cycling subjects. These groups were compared to the group of patients who, according to both psychiatrists, did not meet any of the four criteria sets (nonrapid-cycling group) on the following variables: sex, age, time since first psychiatric contact, bipolar II pattern, history of suicide attempts, and history of major depression or mania in first-degree relatives (as assessed by the Family History Research Diagnostic Criteria
[12]). All of the patient groups were then followed up prospectively for 1 year and assessed every 2 months with the version of the SADS that measures change (SADS-C). Treatment was decided by the physician in charge of each patient. The stability of each rapid-cycling pattern was explored, as well as the rate of conversion of nonrapid-cycling patients to each of those patterns. Within each group of rapid-cycling patients, those who completed 1 year of lithium prophylaxis (according to the protocol described in reference
13) were compared to the nonrapid-cycling patients who received the same treatment on the outcome of prophylaxis (a favorable outcome was defined as a reduction of at least 50% in the time spent in the hospital during the year of lithium treatment compared to the 1-year period preceding the index episode). Comparisons were made with the chi-square statistic (with Yates’s correction as required) for categorical data and Student’s t test for ordinal data.
RESULTS
The kappa values for interrater reliability were 0.93 for definition 1 of rapid cycling (only full affective episodes included), 0.73 for definition 2 (simply waiving duration criteria), 0.75 for definition 3 (waiving duration criteria and requiring a switch in polarity), and 0.80 for definition 4 (waiving duration criteria and requiring at least 8 weeks of fully symptomatic affective illness during the previous year).
The number of patients consistently identified as rapid-cycling by both psychiatrists was 31 (14.8% of the entire study group) when definition 1 was used, 57 (27.1%) when definition 2 was used, 33 (15.7%) when definition 3 was used, and 40 (19.0%) when definition 4 was used. Ninety-seven patients (46.2% of the entire study group) were consistently rated as not meeting any of the four definitions of rapid cycling and were classified as the nonrapid-cycling group.
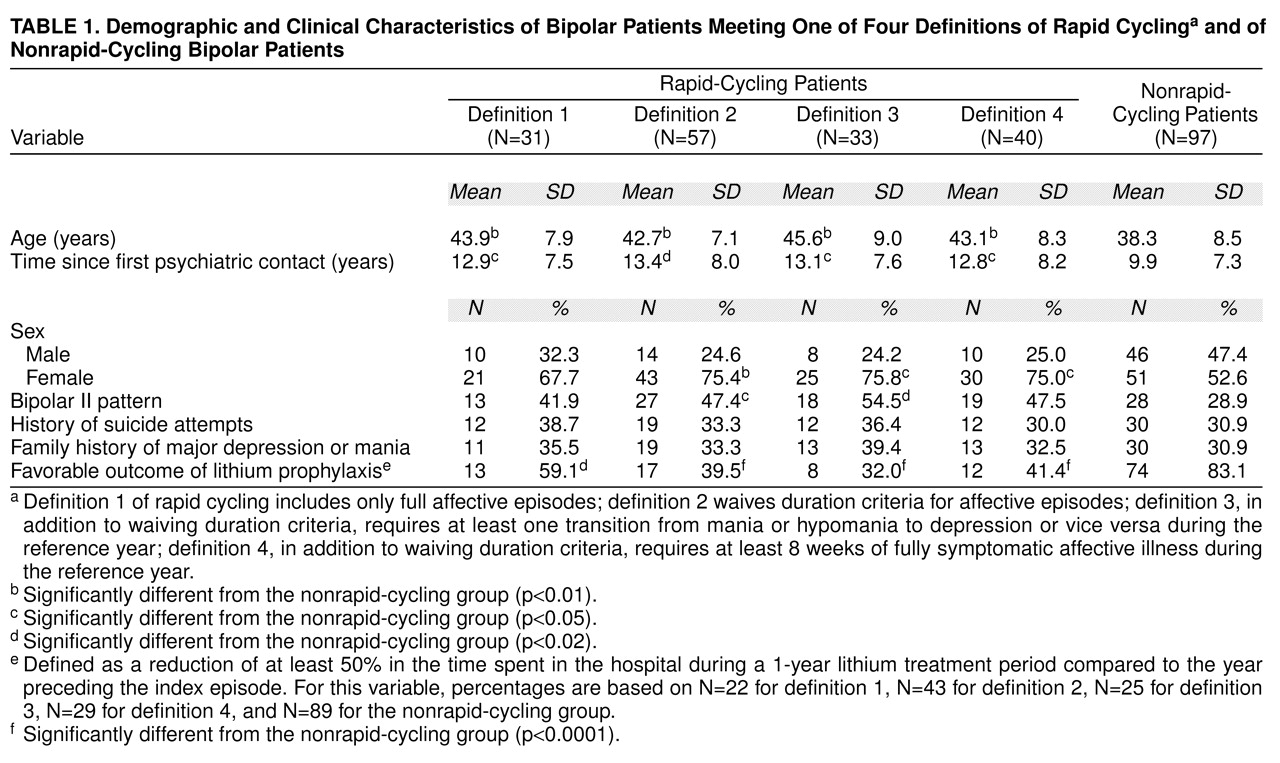
As shown in
table 1, each rapid-cycling group was significantly older and had a longer duration of illness than the nonrapid-cycling group. As compared to the nonrapid-cycling group, the groups meeting definitions 2, 3, and 4 for rapid cycling had a significantly higher proportion of female patients, and the groups meeting definitions 2 and 3 had a significantly higher frequency of the bipolar II pattern. Each rapid-cycling group had a significantly lower proportion of patients with a favorable outcome of lithium prophylaxis than the nonrapid-cycling group (p<0.02 for the group meeting definition 1, and p<0.0001 for the other three groups). The four rapid-cycling groups, compared among themselves, did not differ significantly with respect to the proportion of female patients (χ
2=0.76, df=3, p<0.85), bipolar II patients (χ
2=1.03, df=3, p<0.80), and patients with a favorable outcome of lithium prophylaxis (χ
2=3.78, df=3, p<0.30).
During the follow-up period, stability of the rapid-cycling pattern was observed in 58.1% (N=18) of the patients meeting definition 1, and in 63.1% (N=36), 75.7% (N=25), and 45.0% (N=18), respectively, of those meeting definitions 2, 3, and 4 (χ2=7.75, df=3, p<0.06). The proportion of patients initially classified as nonrapid-cycling who converted to rapid cycling was 9.3% when definition 1 was used and 13.4%, 3.1%, and 10.3%, respectively, when definitions 2, 3, and 4 were used (χ2=2.67, df=3, p<0.60).
DISCUSSION
The results of this study do not allow us to draw definite conclusions concerning the most appropriate way to define rapid cycling. The expression “rapid cycling” seems to encompass a spectrum of conditions, ranging from cases of typical bipolar disorder, in which the number of episodes per year is occasionally high, to states of extreme mood instability, with several transitions from one polarity to the other in a very short time. The DSM-IV definition, although quite reliable, covers only part of this spectrum, and the conditions that are excluded seem to be typical in terms of external validators and relatively stable over time. In fact, our data are in line with previous research evidence showing the highest proportion of female patients (up to 92% according to Wehr et al.
[3]) and of bipolar II patients (up to 82.5% according to Koukopoulos and Reginaldi
[2]), as well as the highest stability of the rapid-cycling pattern (up to 41% of cases in a 5-year follow-up according to Wehr et al.
[3]), in groups of rapid-cycling subjects recruited on the basis of definitions that suspended duration criteria for affective episodes and included switching of polarity as a prerequisite. Waiving duration criteria for affective episodes and requiring circularity of course also seem to decrease the likelihood of a favorable outcome of lithium prophylaxis, which is in line with the clinical impression
(14) that “patients with very short episodes of high frequency” are the least treatment-responsive within the rapid-cycling spectrum.
The suspension of the duration criteria for affective episodes, however, seems to produce a decrease in the interrater reliability of the definition of rapid cycling. This result is not comparable to that reported by Bauer et al.
(5), who found high interrater reliability in the identification of truncated rapid cycling but made their assessments using case vignettes rather than independently interviewed real patients. In our setting, the assessors found it difficult to differentiate retrospectively both between short affective episodes and subclinical mood fluctuations and between multiple short affective episodes and a single mixed episode. This may reflect in part the limitations of currently available diagnostic interviews, but a partial overlap between rapid cycling with short episodes and mixed states is probably factual. Requiring at least 8 weeks of fully symptomatic affective illness during the previous year, in addition to waiving duration criteria for affective episodes, improves the reliability of the definition but reduces the stability of the pattern on follow-up.
In conclusion, our data are not sufficient to argue that any of the proposed alternative definitions of rapid cycling shows a substantial advantage over the DSM-IV definition. However, they suggest that the definition that waives duration criteria for affective episodes and requires circularity of course is associated with the highest percentage of female patients, bipolar II patients, and nonresponders to lithium and is the most stable on follow-up. A currently missing element is whether this definition is also associated with the most favorable response to mood stabilizers other than lithium.