Obsessive-compulsive disorder (OCD) affects 1%–3% of the world’s population and imposes high individual and socioeconomic burdens
(1 –
3) . The heredity of the illness has been under investigation since 1930
(4) . However, the use of different diagnostic criteria for OCD and different methodological approaches limited the comparability of early studies.
Using a family study design with matched control subjects and applying operational criteria for the assessment of OCD, McKeon and Murray
(5) found no increased familial risk of OCD, but they did observe a greater rate of mental illness in the first-degree relatives of OCD probands. Bellodi et al.
(6), using no comparison group, found a low prevalence of OCD (3.4%) among first-degree relatives. In cases with an early onset (before age 14), prevalence reached 8.8%, which seems to indicate a biological vulnerability. Black et al.
(4) described an elevated rate of anxiety disorders and subclinical OCD in OCD families but observed no familial aggregation of OCD in first-degree relatives.
Pauls et al.
(7) were the first to find a significantly higher rate of OCD (10.3% versus 1.9%) and subclinical OCD (7.9% versus 2.0%) among first-degree relatives of individuals with clinically ascertained OCD than among relatives of control subjects. The results of the Pauls et al. study were replicated by the Johns Hopkins OCD Family Study
(8), which used multiple recruitment sites (treatment facilities) to reduce the potential for selection bias and used carefully selected community comparison subjects. In two earlier twin studies of OCD, concordance rates of monozygotic versus dizygotic twins were 80% versus 20%
(9) and 87% versus 47%
(10) . However, these studies used small numbers of twin pairs and diagnostic procedures that would not meet today’s standards.
To our knowledge, all family studies of OCD have used patients from treatment facilities, a population that has been shown to have higher rates of comorbid disorders than persons with OCD in the general population
(11) . For many patients with OCD, the distress caused by comorbid anxiety disorders or depressive episodes is the ultimate reason for seeking treatment. As is well known, many persons with OCD avoid seeking professional help (OCD has been referred to as “the hidden disease”)
(12) despite the disabling severity of their symptoms. Thus, results from available family studies may be biased by yet unknown factors that are responsible for differences in help seeking and thus accessibility for research purposes. Moreover, it remains unclear to what extent comorbid disorders that also affect first-degree relatives of persons with OCD influence the familial transmission of OCD itself
(13 –
16) . Thus, only a family study that includes people with untreated OCD from the general population would be able to overcome the methodological limitations of previous studies with clinically ascertained OCD probands.
This investigation is part of the German Epidemiologic Network for OCD Studies (GENOS), a large family study of OCD carried out at four different sites. GENOS includes not only a sample of patients with OCD drawn from treatment facilities but also a sample of individuals with OCD identified in a general population study. GENOS was established to study the familial aggregation of OCD, to identify psychological, neuropsychological, and genetic factors that are related to the familiality of OCD, and to characterize subtypes of OCD.
In the present study, three hypotheses were investigated:
First-degree relatives of all OCD probands from treatment facilities and from the community combined have significantly higher rates of OCD and subclinical OCD than relatives of comparison subjects.
First-degree relatives of OCD probands from treatment facilities and from the community each have significantly higher rates of OCD and subclinical OCD than relatives of comparison subjects.
Given the high severity of symptoms in OCD probands from treatment facilities, the first-degree relatives of these probands have higher rates of OCD and subclinical OCD than do first-degree relatives of OCD probands from the general population.
Method
The study was approved by the local ethics committees at the four study sites. All participants gave written informed consent before they were enrolled in the study.
Community Sample
The Study of Health in Pomerania (SHIP) is a cross-sectional study of the population in Western Pomerania, the northeastern coastal region of Germany
(17) . A random sample was drawn from the total population of 212,157 people living in the study area. Data were collected between October 1997 and May 2001. The SHIP population comprised 4,310 participants (68.8% of eligible subjects) aged 20–79 years. Five screening questions for OCD symptoms (checking, washing, need for symmetry, obsessions, and aggressive impulses) were included in the self-rating section of SHIP. Responses to all five screening questions were available for 4,067 participants. Subjects whose scores on these questions were above the 95% percentile (N=204) were contacted by letter and by telephone. Those who could not be contacted (N=11), declined to participate (N=29), did not have at least two living first-degree relatives (N=43), or did not give permission for researchers to contact their relatives (N=15) were excluded from further diagnostic procedures. Of the remaining 106 subjects, 15 were identified by direct interview as having definite OCD (N=15). From these 15 community probands, 58 first-degree relatives were included in the study (on average, 3.9 relatives per proband).
From the GENOS database, as many OCD probands from treatment sites, comparison subjects, and first-degree relatives for both groups as possible were matched to the 15 community probands and their first-degree relatives on age of the OCD proband (±10 years) and the type of interview (direct or indirect) given to their first-degree relatives. This was done to minimize the putative effects of the family structure (such as whether the first-degree relatives were parents or offspring) and the type of interview on the familial rate of OCD among the three samples. This matching procedure resulted in the inclusion of 90 OCD probands from treatment sites and 70 comparison subjects and their first-degree relatives.
Clinic Sample
Ninety adult OCD probands at least 18 years of age and their first-degree relatives were selected from our outpatient clinic sample (N=156) from four psychiatric university hospitals in Germany (Bonn, Homburg, Cologne, Stralsund). From these probands, diagnostic information was obtained on 285 first-degree relatives (on average, 3.2 relatives per proband) through direct and indirect interviews.
Comparison Sample
From a pool of 117 subjects who did not have definite or subclinical OCD, 70 comparison subjects and their first-degree relatives were selected for the study. Of these 70 subjects, 33 were randomly recruited from SHIP (plus 126 relatives), 26 from community registers in Bonn (plus 86 relatives), and seven from community registers in Cologne (plus 21 relatives), and four (plus 14 relatives) were volunteers who were recruited by public announcement in Homburg.
All OCD case probands met full DSM-IV criteria for lifetime OCD during their worst episode. Probands and comparison subjects diagnosed as having schizophrenia, mental retardation, or dementia were excluded.
All included probands, comparison subjects, and their relatives were Caucasian.
Diagnostic Procedures
Altogether, 384 face-to-face interviews and 109 telephone interviews were conducted. All OCD probands and comparison subjects were directly interviewed, either face-to-face or by telephone. For 131 (38%) of the relatives of OCD probands and 95 (38%) of the relatives of comparison subjects, informant interviews were conducted with one to three relatives who were familiar with the subject because the subject was deceased or refused to participate or the proband refused to allow contact with relatives. All interviews were conducted between October 2001 and December 2003.
Diagnostic instruments included the German-language version of the Schedule for Affective Disorders and Schizophrenia—Lifetime Version, Modified for the Study of Anxiety Disorders, Updated for DSM-IV (SADS-LA-IV)
(18,
19) and the Family Informant Schedule and Criteria (FISC)
(20) . Sections were added for a detailed assessment of OCD (the Yale-Brown Obsessive Compulsive Scale and the Yale-Brown Obsessive Compulsive Scale Symptom Checklist [
21,
22 ]), tics, Tourette’s syndrome, eating disorders, body dysmorphic disorder, and impulse control disorders according to DSM-IV criteria.
Subjects were interviewed by psychiatrists, clinical psychologists, and doctoral-level clinical researchers. All interviewers had undergone intensive and continuous training in the diagnostic procedures. At each study center, one senior psychiatrist supervised all interviews. Every third month, interviewers from all centers were trained together with videotaped interviews. Interviewers were blind to whether subjects were comparison subjects, OCD probands from SHIP, relatives of comparison subjects, or relatives of OCD probands, although in some cases of OCD patients receiving treatment at a hospital, interviewer blindness was limited.
All diagnoses were made according to DSM-IV criteria. Diagnoses were made on the basis of available diagnostic materials (the SADS-LA-IV and FISC interviews) by the expert psychiatrist at each center. In some cases, additional information was obtained from medical records or through an additional interview conducted by the expert psychiatrist. Consensus diagnoses were made by all expert psychiatrists from all centers (H.J.G., A.H., S.R., and P.F.) in cases with difficult differential diagnoses.
Interrater reliability was assessed in 15 randomly selected patients with OCD (10% of the face-to-face interviews) and 11 randomly selected comparison subjects (9.5% of the face-to-face interviews). Kappa values for diagnostic agreement were 1.0 for OCD, 0.92 for major depressive disorder, 1.0 for panic disorder, 0.87 for social phobia, 0.76 for simple phobia, 1.0 for general anxiety disorder, 1.0 for somatoform disorder, 0.84 for posttraumatic stress disorder, 1.0 for substance use disorders, 1.0 for eating disorders, 0.47 for tic disorders, and 0.77 for OCD spectrum disorders.
The diagnosis of OCD was considered definite if all required DSM-IV criteria were met. A diagnosis of subclinical OCD was given if characteristic OCD symptoms were present but the criterion of significant distress or impairment or of duration (>1 hour per day) was not met.
Data Analysis
To compare demographic characteristics in case and comparison probands, chi-square tests were used for categorical data and t tests for continuous data. The rate of OCD in case versus comparison relatives was assessed with chi-square tests, and odds ratios were calculated for risk estimation. In a more complex model, the relatives’ age-related risk of being affected by OCD was estimated by a Cox proportional hazards analysis
(23) . With Cox regression it is possible to calculate the hazard ratio and survival time for cases under the influence of certain covariates for all cases in the model, even if only a small proportion are affected by the illness. Cases in which the “event”—in this model, relatives being affected by OCD—did not take place during their lifetime up to the time of the interview were censored. This model specifically estimates the risk of relatives’ developing OCD given their present age. A significant Wald chi-square statistic indicates that the variable is useful for the Cox regression model. To adjust for differences between the tested samples, the following covariates were included in all Cox regression models: sex of the proband or comparison subject, type of interview (direct or informant), education (college or high school graduates versus others) of the proband or comparison subject, number of relatives per family (≤2 or >2), and type of relative included (parent, sibling, or offspring [yes or no for each]). The contribution of the type of relative to the risk for definite and subclinical OCD in relatives was also computed by including each of the three values for type of relative separately into the Cox regression.
For the relatives of OCD probands from both treatment facilities and the community, the following variables were each entered separately into the Cox regression models: comorbid lifetime diagnosis of anxiety disorders, major depression, or anxiety disorder without comorbid depression in the probands, and age at onset of OCD (≤18 years or >18 years) in the probands. This procedure allowed us to investigate in an exploratory fashion whether these variables interacted with the risk of relatives’ being affected by definite or subclinical OCD. The Cox regression models were also adjusted for the covariates as indicated above.
Results
Basic Demographic and Clinical Characteristics
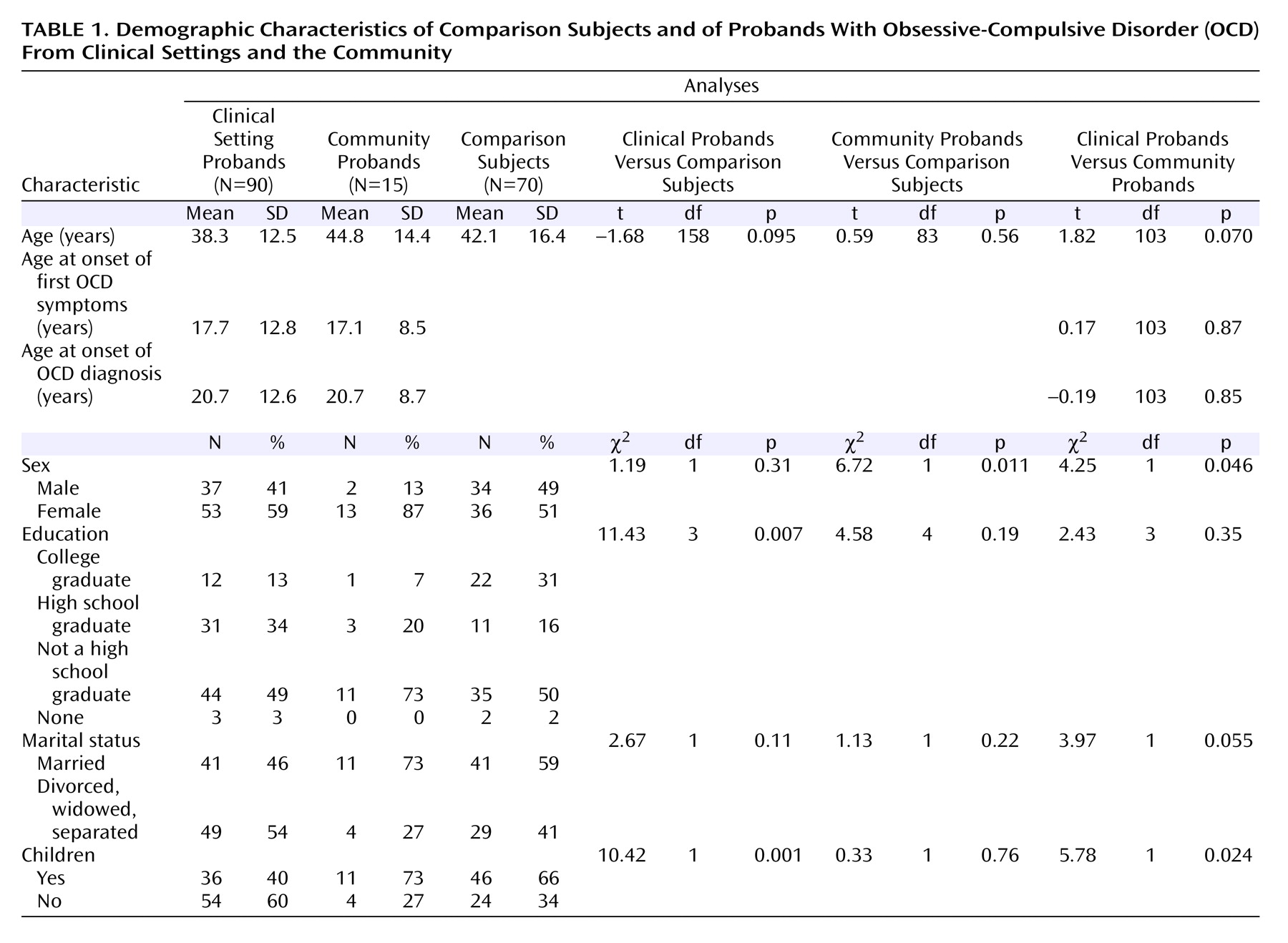
Basic demographic and clinical characteristics of probands and comparison subjects are listed in
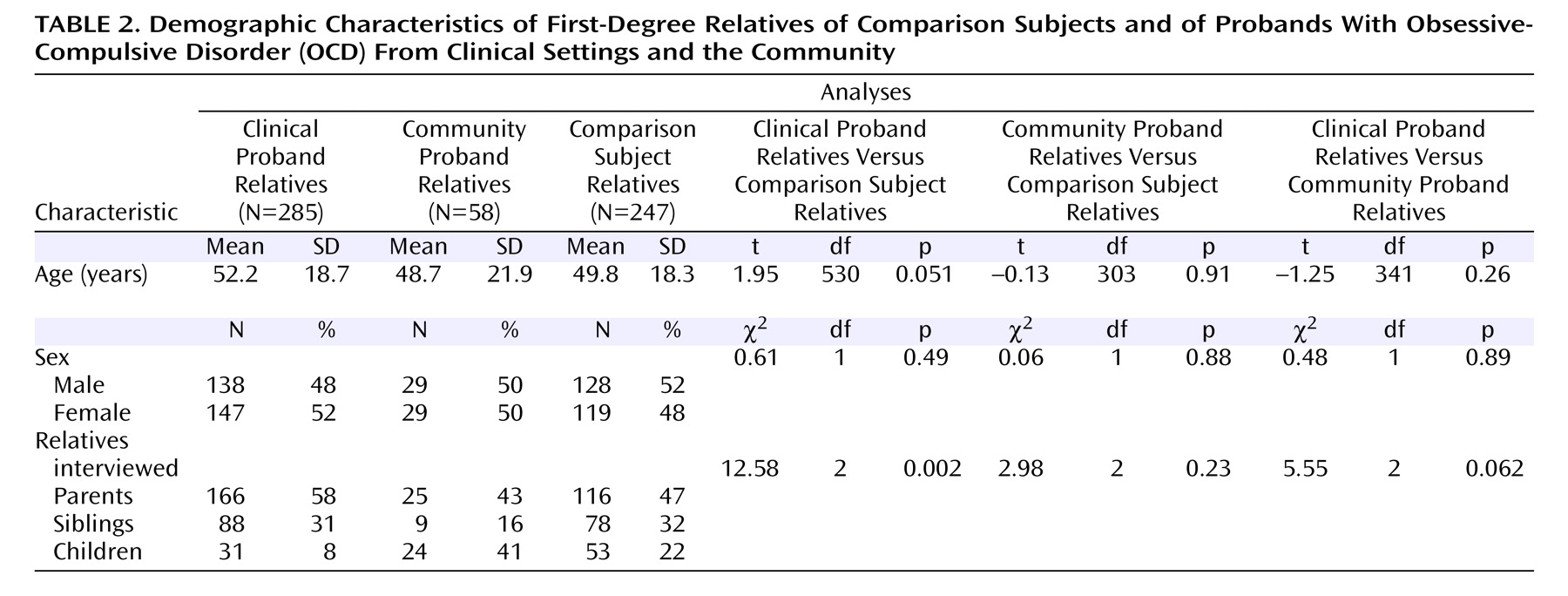
Table 1, and basic demographic characteristics of first-degree relatives are listed in
Table 2 . No difference in the age at onset of OCD was noted between probands from the treatment facilities and those from the community.
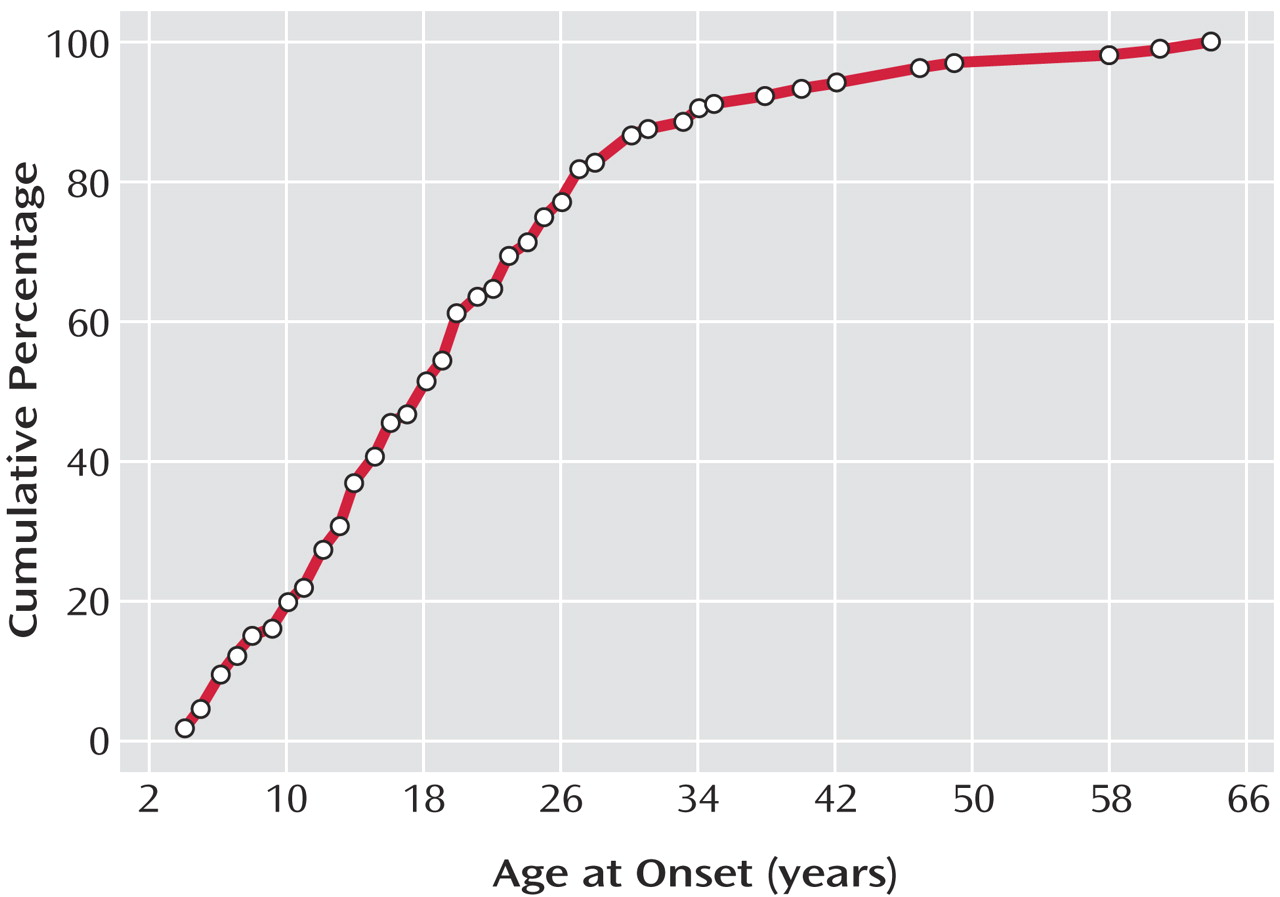
Figure 1 depicts the cumulative percentage of ages at onset of OCD in the 105 probands selected.
As expected, the lifetime comorbidity for any depressive disorder was higher among the OCD probands from treatment facilities (70%) than among those from the community (40%) (χ 2 =5.13, df=1, p=0.037). In contrast, the lifetime comorbidity of other anxiety disorders was lower among the OCD probands from treatment facilities (48%) than among those from the community (67%) (χ 2 =4.95, df=1, p=0.047).
Prevalence of OCD and Subclinical OCD in Relatives
At least one relative had definite OCD in 33% of the families of OCD subjects from the community, in 16% of the families of OCD patients from treatment facilities, and in 4% of the families of comparison subjects (χ 2 =10.7, df=2, p=0.004). At least one relative had subclinical OCD in 60% of the families of OCD subjects from the community, in 15% of the families of OCD patients from treatment facilities, and in 10% of the families of comparison subjects (χ 2 =16.3, df=2, p≤0.001).
The prevalence of definite OCD in relatives of clinical and community probands combined was 6.4%, compared with 1.2% for comparison relatives (odds ratio=5.3; 95% confidence interval [CI]=1.6–17.4, χ 2 =9.6, df=1, p=0.002), and the prevalence of subclinical OCD was 5.9%, compared with 2.9% for comparison relatives (odds ratio=2.1; 95% CI=0.9–4.8, χ 2 =2.9, df=1, p=0.09). Cox proportional hazards analyses revealed a 6.2-fold higher risk for definite OCD for relatives of all OCD probands compared with relatives of comparison subjects (95% CI=1.8–21.3, Wald χ 2 =8.4, df=1, p=0.004) and a 2.2-fold risk higher for subclinical OCD compared with relatives of comparison subjects (95% CI=0.9–5.3, Wald χ 2 =2.9, df=1, p=0.09).
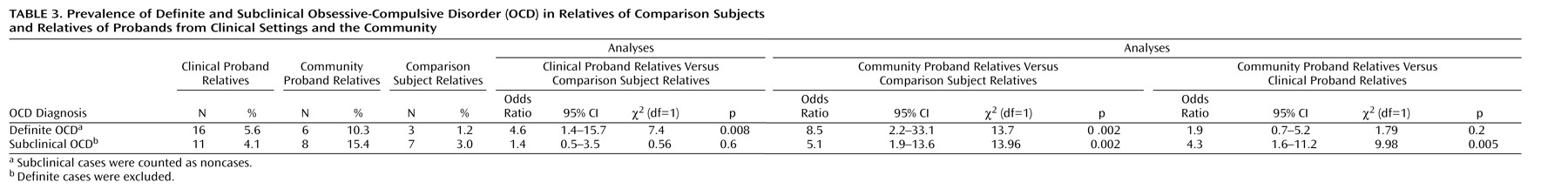
As
Table 3 shows, the prevalence of definite OCD in relatives of probands from treatment facilities (5.6%) was significantly higher than in comparison relatives (1.2%), but the prevalence of subclinical OCD was nonsignificantly different between both groups of relatives. Relatives of probands from treatment facilities (5.6%) did not have a higher prevalence of definite OCD than relatives of community probands (10.3%). Moreover, relatives of community probands had a significantly higher rate of subclinical OCD (15.4%) than relatives of probands from treatment facilities (4.1%).
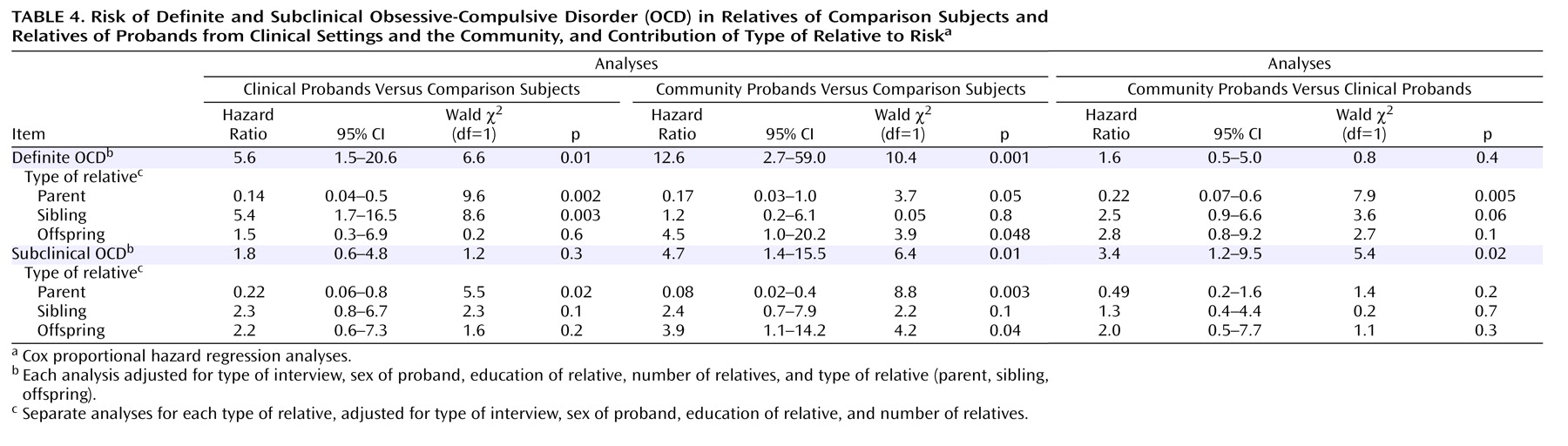
Cox regression models were used to analyze the risk of relatives’ being affected by OCD in age-dependent fashion while adjusting for potential confounders (the sex and educational level of the OCD proband, the interview type, the number of relatives included per family, and type of relative [parent, sibling, offspring]). It was confirmed that relatives of community probands had a significantly higher risk of subclinical OCD (hazard ratio=3.4) and a nonsignificantly higher risk of definite OCD (hazard ratio=1.6) compared with relatives of probands from treatment facilities (
Table 4 ).
Among the relatives of all OCD probands (from clinical and community settings combined), the comorbid lifetime diagnosis of an anxiety disorder (hazard ratio=1.0; 95% CI=0.4-2.5, Wald χ 2 >0.001, df=1, p=0.9), major depression (hazard ratio=0.5; 95% CI=0.2-1.3; Wald χ 2 =2.1, df=1, p=0.15), or an anxiety disorder without comorbid depression (hazard ratio=2.3; 95% CI=0.7-7.3; Wald χ 2 =1.9, df=1, p=0.17) and the proband"s age at onset of OCD (hazard ratio=1.2; 95% CI=0.5-2.9; Wald χ 2 =0.1, df=1, p=0.75) did not interact significantly with the risk of relatives" being affected by definite OCD.
Discussion
Our first hypothesis was confirmed by the data: Relatives of all OCD probands (from clinical and community settings combined) had a significant 6.2-fold higher risk of definite OCD compared with relatives of comparison subjects. This rate corresponds to results from prior studies that found a higher prevalence of OCD among first-degree relatives in the United States
(7,
8) . However, the overall risk of subclinical OCD in relatives of OCD probands (hazard ratio=2.2) was lower than rates previously reported
(7,
8) .
The second hypothesis was partly confirmed by the data: Relatives of OCD cases from treatment facilities had a significant 5.6-fold higher risk of definite OCD, but not an elevated risk of subclinical OCD, compared with relatives of comparison subjects. Relatives of probands from the community had an elevated risk of both definite and subclinical OCD.
Our third hypothesis was not confirmed: 10.3% of relatives of community probands met criteria for a lifetime diagnosis of definite OCD, compared with 5.6% of relatives of probands from treatment facilities. For subclinical OCD, relatives of community probands had a significant 3.4-fold higher risk than relatives of probands from treatment facilities.
The results of this study confirm the familial transmission of OCD, which has previously been described in only two controlled family studies in the United States
(7,
8) . The finding that the familial transmission of definite and subclinical OCD was also detected in a nonclinical sample from an epidemiological study is of special interest because of the absence of selection bias that might occur as a result of treatment seeking behavior for OCD or comorbid disorders that could have triggered treatment seeking. Our results thus clearly support and validate the findings on familiality of OCD in treatment samples.
An early age at onset of OCD has been related to a higher familial aggregation rate, suggesting the existence of an OCD subtype with a higher genetic loading
(7,
8,
13,
24) . However, in Cox regression analyses, the probands’ age at onset was not associated with an increase in the risk that OCD relatives would be affected by definite or subclinical OCD.
The analysis of comorbid disorders in our sample revealed a lower rate of depressive disorders and a higher rate of comorbid anxiety disorders in the community probands compared with those from treatment facilities. This finding would be consistent with a lower genetic liability of OCD associated with depressive disorders and a higher liability associated with anxiety disorders
(15,
25) . This hypothesis found some support in our nonsignificant findings in Cox regression analyses that the familial risk of OCD was lower among subjects with comorbid depression and higher among subjects with a comorbid anxiety disorder without comorbid lifetime depression. These nonsignificant results will require replication in the complete GENOS sample, however.
A selection bias because of the sampling procedure of the community probands seems unlikely. At the initial step of the recruitment procedure, the probands were not told that they would be participating in a study of mental illness or of OCD in particular. From the 106 probands who were screened by direct interview for the diagnosis of OCD, all later agreed to participate. First-degree relatives of all 15 OCD probands identified were included in the study.
Evidence is accumulating that OCD is a familial condition that may have a genetic etiology. This study adds to previous knowledge by ruling out the proposition that familial aggregation only occurs among probands who have more severe symptoms and seek treatment, and in fact our study suggests that probands from the community may be characterized by a higher genetic load. It will be important to further identify psychological and neuropsychological risk factors for familial transmission in order to determine etiologically homogeneous subgroups of OCD that will facilitate the search for genetic risk factors. Clinicians and general practitioners should be aware that first-degree relatives have an elevated risk of being affected by OCD and offer the necessary diagnostic procedures and therapeutic interventions when indicated.