Mortality associated with mental disorder has increased in Europe during the last decades
(1) . Eating disorders and substance abuse are the psychiatric diagnoses with the highest risks of premature death
(2) . Among the eating disorders, anorexia nervosa has the worst prognosis. The mortality rate for women with anorexia nervosa is substantially greater than for female psychiatric inpatients as a group
(3) . However, there is considerable controversy about the magnitude of the mortality rate in anorexia nervosa, from 16% reported in a 21-year follow-up study
(4) to no increased mortality 30 years after diagnosis relative to the general population
(5) . Differences in age at onset, gender, duration of illness, and other inclusion procedures explain some of the differences. A previous study has suggested that anorexia nervosa mortality may be lower than formerly supposed
(6) . We hypothesize that decreased mortality is a result of increased awareness of medical complications and improved medical care
(7) and to the commonly applied broad perspective approach of long-term treatment. Follow-up studies of national cohorts with similar inclusion criteria are one way to test this hypothesis. In this study, we used the Swedish National Registers to examine any changes concerning survival occurring over the last decades in female hospitalized patients with anorexia nervosa.
Method
This study was based on data from the Swedish Patient Discharge Register and the National Cause of Death Register, which contain information about hospital discharges and deaths for the entire Swedish population. The Cause of Death Register covers—with certainty—all deaths. The underlying medical reports—missing in about 0.5% of all cases—constitute the major limitation of accuracy
(8) . The correctness of diagnoses are investigated usually every second year by independent studies of random samples, demonstrating coding errors between 1.2 (SD=0.3) regarding ICD chapter and 6.3 (SD=0.7) regarding ICD complete code
(8) .
The first study population consisted of all female patients born between 1958 and 1967 who were hospitalized with a main diagnosis of appetite disorder (306.50 in ICD-8) between 1977 and 1981 (N=564). The second cohort consisted of all female patients born between 1968 and 1977 who were hospitalized with a main diagnosis of anorexia nervosa (307B in ICD-9) between 1987 and 1991 (N=554). Mean age at first hospital admission was 16.4 years (SD=2.75) in the 1977–1981 cohort and 15.9 years (SD=2.59) in the 1987–1991 cohort. The cohorts were followed from the first hospital admission until 1992 and 2002, respectively, in the National Cause of Death Register. With the intention of illuminating the whole panorama of anorexia nervosa mortality of these age groups, anorexia nervosa-related deaths among female patients born during the two study decades—but with no hospital care due to anorexia nervosa during the index periods—were also registered until 1992 and 2002, respectively.
Results
Twenty-five deaths (4.4%) from the 1977–1981 hospital cohort were recorded, with the cause of death for 19 having a probable association with anorexia nervosa (anorexia nervosa: N=6, suicide: N=10, myocardial disease: N=1, drug overdose: N=1, constipation: N=1) and six with no obvious such link (cerebral palsy, traffic accident, diabetes, homicide, and two patients with cancer). In the 1987–1991 hospital cohort, seven patients (1.3%) died, four with an anorexia-related cause of death (anorexia nervosa: N=1, suicide: N=2, drug overdose: N=1) and three with no obvious link (cancer and two who died in traffic accidents).
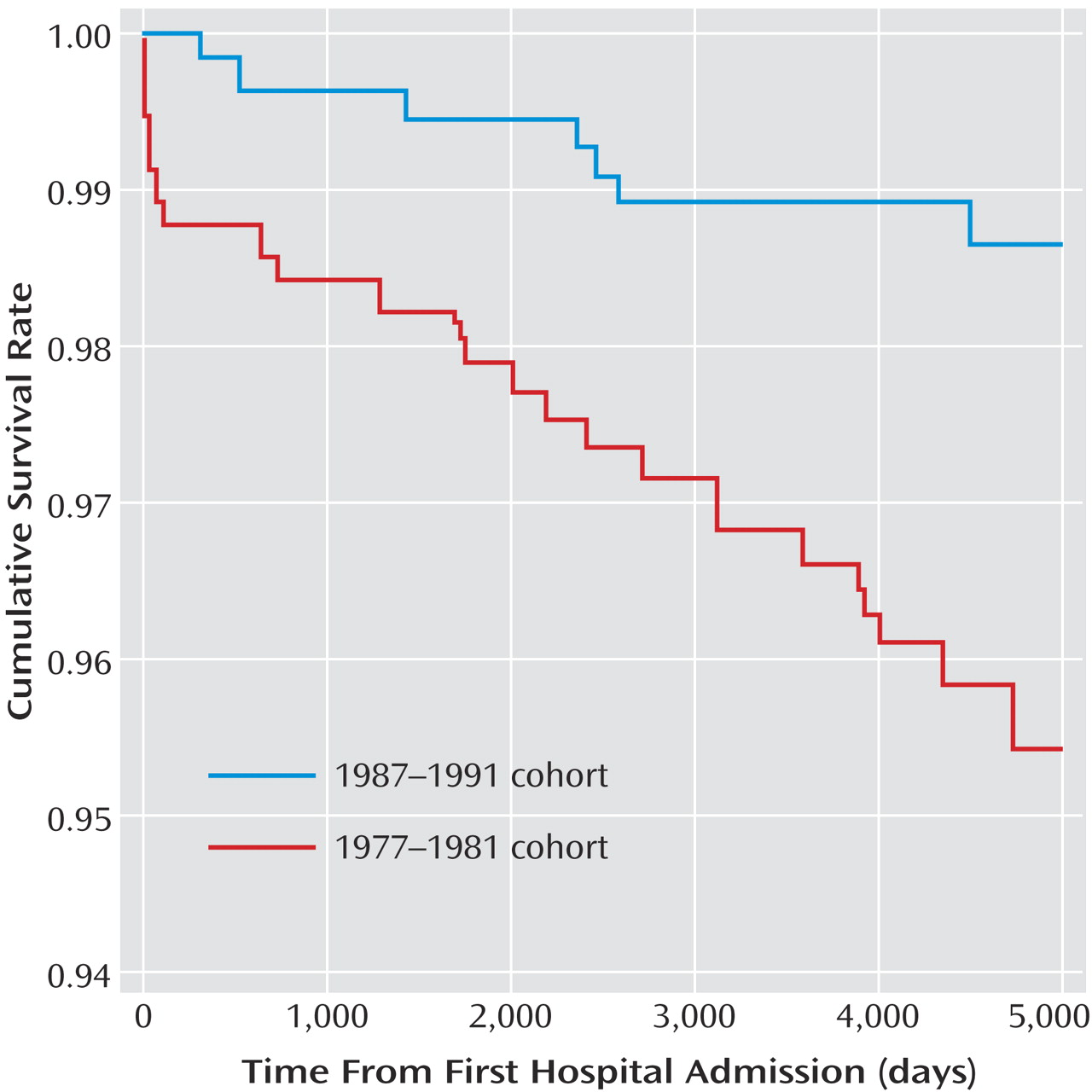
Figure 1 demonstrates improved survival during the first months of hospital care as well as improved long-term survival 5–10 years after hospital care. The hazard ratio of death—related and unrelated to anorexia nervosa—during the follow-up period was 3.7 (95% confidence interval=1.6–8.5) for the 1977–1981 cohort relative to the 1987–1991 cohort. The standardized mortality ratios were 7.7 (1977–1981 cohort) and 2.9 (1987–1991 cohort).
Among women born between 1958 and 1967 with no hospitalizations for anorexia nervosa during the period 1977–1981, three anorexia nervosa-related deaths were registered by 1992 (two had been hospitalized outside the index period, the third had no registered hospitalizations). Among women born between 1968 and 1977 with no hospitalizations for anorexia nervosa during the period 1987–1991, two anorexia nervosa-related deaths were registered by 2002 (both had been hospitalized outside the index period).
Discussion
As hypothesized, mortality decreased from 4.4% to 1.2% over one decade, probably mirroring the improved care for anorexia nervosa patients. We believe that improved medical care, including treatment of nutritional emergency states, is primarily reflected in the decreased risk of death during the first months of hospital care and that improved long-term care is reflected in the decreased risk 5–11 years after first hospitalization. The establishing of specialized units during the second period—rather than new knowledge about treatment strategies—probably constitutes the core of such presumed improvement. The more successful prevention of suicide during the second period seems to be one factor of importance. It could be a sign of improved alertness to suicidal behavior or a general effect of improved care—or both. An alternative/complementary explanation of the decreased mortality is improved detection of anorexia nervosa as a result of increased awareness of the illness, resulting in hospitalization at a time when the illness was less advanced. This would be consistent with the slightly younger age of the 1987–1991 cohort.
An estimation from a commonly cited lifetime prevalence of 0.5% demonstrates that the number of patients included in our cohorts would represent about 20% of such imagined anorexia nervosa populations. This seems to be consistent with our selection of patients, representing only the cases having necessitated hospitalization (also taking the number of cases developing anorexia nervosa after the study period into consideration).
This report followed adolescent patients of anorexia nervosa to 25–34 years of age. Further studies with a longer follow-up time are needed to describe the mortality of chronic anorexia nervosa in middle age. It is quite possible that mortality due to complications of the prolonged starvation emergency will be more evident in this older age group.
It is interesting that the overall mortality associated with mental disorder was rather stable in Sweden during the 1980s and the 1990s
(1) . This speaks against the hypothesis that the changes in anorexia nervosa mortality could be explained by more general changes in psychiatric care—or other societal changes affecting psychiatric patients.
Differences between ICD-8 and ICD-9—and how these classifications were applied—may have influenced our findings but hardly the magnitude of the change in mortality. The individuals in focus—being hospitalized due to severity of anorexia nervosa—have probably more easily been recognized and correctly diagnosed by the medical profession than outpatients. The fact that the identified groups were similar in size adds some support to this presumption. There was only one case of anorexia nervosa-related death with no hospital care due to anorexia nervosa registered from the same age cohorts, which speaks against the hypothesis that inclusion of outpatient cases would have yielded contrary results. A strength of our approach is the use of two complete age cohorts.
We suggest that our results may be generalized to other Western countries where anorexia nervosa care has developed along the same lines during the 1990s. With the aim of further decreasing the mortality rate in anorexia nervosa, an important research line for the future would be to investigate a cohort of cases with fatal outcome, trying to analyze why the general improved care was not successful in these cases.