The perspective of developmental psychopathology encourages a life-course approach for research regarding the role of childhood conditions and processes in the etiology and course of psychiatric disturbances
(1 –
4) . Posttraumatic stress disorder (PTSD) has not been included in prior longitudinal studies that have followed children into adulthood. PTSD as defined in DSM-IV requires exposure to a qualifying traumatic event and a clinical syndrome (consisting of reexperiencing, avoidance and numbing, and increased arousal) connected to the traumatic event in content and temporal order. The disturbance must last at least 1 month and cause clinically significant distress or impairment. Epidemiological surveys in the United States have documented that the majority of community residents have been exposed to one or more PTSD-level traumatic events, as defined in DSM-IV. However, the conditional probability of developing PTSD following traumatic exposure is less than 10%
(5 –
8) . A sex-related pattern has been documented. Men are more likely to experience traumatic events, in particular, events that involve assaultive violence, serious accidents, and witnessing violence; women are more likely than men to develop PTSD once trauma exposure occurs
(7 –
14) .
Previous research has identified an array of suspected causal determinants of PTSD among community residents exposed to traumatic events. These include family history of psychiatric disorders, preexisting disorders (including conduct problems in childhood), and early childhood adversity
(9,
15 –19) . The role of cognitive abilities as a modifier of the susceptibility for PTSD was reported in studies of Vietnam combat veterans
(20) and was observed among inner-city children exposed to trauma
(21) . The list of suspected causal determinants for exposure to traumatic events overlaps, in part, with the list of PTSD determinants. Prior studies on suspected childhood determinants of traumatic events and PTSD have relied on cross-sectional designs and retrospective data. Consequently, recall bias threatens the validity of inferences drawn from these studies
(17) . In the world literature on PTSD, we have been unable to locate prospective studies that began in early childhood and followed cohorts to adulthood.
In this community-based prospective study, children (age 6–7 years old) were assessed as they entered the first grade of primary school. They were then followed to young adulthood, which created an opportunity to study prospectively childhood antecedents of traumatic event exposure and risk of PTSD after trauma. We previously reported descriptive information on exposure to traumatic events and PTSD collected at the follow-up assessment of the cohort in adulthood
(6) . The vast majority of the cohort (82.5%) had experienced one or more traumatic events up to the time of interview; exposure was higher in male subjects than female subjects. The conditional probability of PTSD given exposure to trauma was 8.8%, a figure similar to estimates in recent community-based surveys
(7,
8) . As in these other surveys, the conditional probability of PTSD was higher in female subjects than male subjects.
In this report, we examine data from assessments conducted at the start of schooling to evaluate the extent to which potentially malleable individual level factors (cognitive ability, behavioral problems, and emotional problems) measured in childhood might account for the risk of 1) exposure to traumatic events and 2) developing PTSD following exposure to traumatic events.
Method
Data are from a prospective study conducted within the context of a group randomized prevention trial
(22 –
24) . During two successive school years (1985 and 1986), a total of 2,311 youths entered first grade in 19 primary schools within a single public school system of a mid-Atlantic city in the United States. Fifteen years later, nearly 75% of the surviving subjects were interviewed face-to-face to assess lifetime traumatic experiences and PTSD
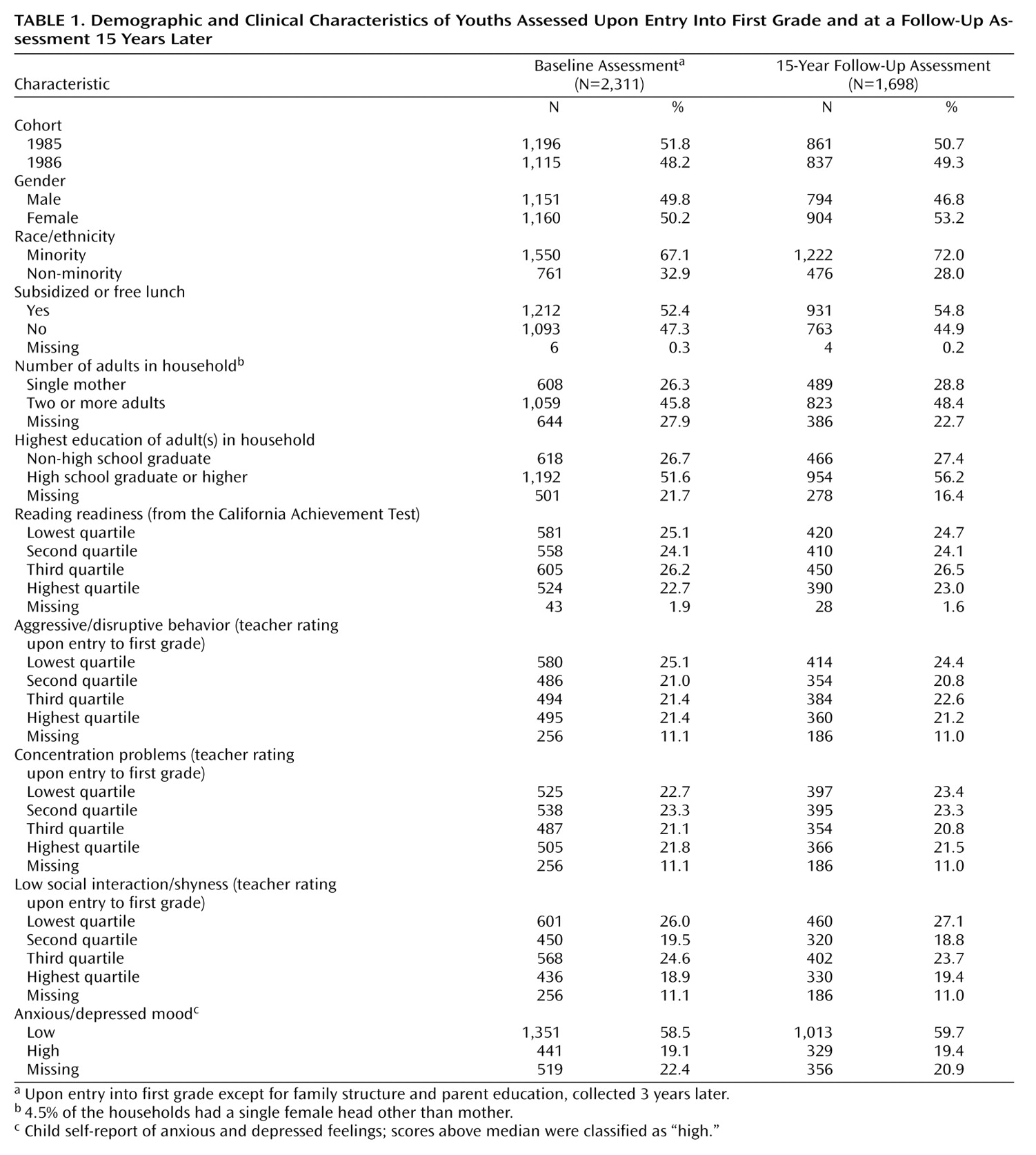
(6) . The total sample of 2,311 youths who had entered first grade and the 1,698 interviewed as young adults were similar with respect to family and child characteristics (
Table 1 ). However, attrition was slightly greater among male and non-minority subjects. Study protocols were approved by institutional review boards of Johns Hopkins University; Michigan State University’s institutional review board also approved the data analysis activities. Parental signed consent and child assent were obtained for the childhood assessments, followed by signed consent from each participant after age 18.
Data and Measurement of Key Variables
In early adulthood, when participants were 20–23 years of age (mean age=21), exposure to traumatic events and PTSD were assessed as part of a 90-minute standardized interview administered by experienced lay interviewers without special clinical training or credentials
(8) . The PTSD module of the interview began by eliciting a history of lifetime exposure to DSM-IV qualifying traumatic events, using a list of 18 traumatic event types. Respondents were asked to identify the most upsetting traumatic event (the worst event) they had experienced from the complete list of traumatic events they reported. PTSD was evaluated in connection with the worst event, using the PTSD section of the World Health Organization Composite International Diagnostic Interview (CIDI), Version 2.1, which is modeled after the NIMH Diagnostic Interview Schedule (DIS). A validation study found good agreement between the standardized interview and independent clinical reinterviews
(25) .
The 18 traumatic events were grouped into two broad categories: six events that involved assaultive violence (rape, sexual assault other than rape, being badly beaten up, being held captive/tortured/kidnapped, being shot/stabbed, and being mugged/threatened with a weapon) and 12 that did not (serious car accident; other serious accident; natural disaster; life-threatening illness; child’s life-threatening illness; witnessing of a killing/serious injury; discovering a dead body; learning of close friend/relative who was attacked, raped, sexually assaulted, or suffered a serious car accident or some other serious accident; and learning of sudden unexpected death of a close friend/relative).
Childhood Assessments in Primary School
Central computerized school data sources provided standardized reading readiness scores assessed at the beginning of primary school, based on the California Achievement Test, forms E and F
(26) . Family characteristics (e.g., single mother, educational status of adults in household) were assessed by parental report.
As described by Werthamer-Larsson et al.
(27), classroom teachers used the Teacher Observation of Classroom Adaptation–Revised to rate the children on three domains of behavior problems soon after the pupils entered first grade. A trained assessor guided the teacher through a structured interview of 36 items pertaining to a child’s adaptation to classroom task demands over the preceding 3-week period. The domains of behavior included 1) aggressive/disruptive behaviors (starts fights, acts stubborn, breaks rules, breaks things, yells at others, takes others’ property, lies, harms others and property, and teases classmate); 2) concentration problems (completes assignments, concentrates, works well alone, works hard, pays attention, learns up to ability, eager to learn, stays on task, mind wanders, easily distracted, and poor effort); and 3) low social interaction/shyness (plays with classmates, initiates interaction, interacts with classmates and teacher, friendly, avoids classmates and teacher, rejected by classmates). Items were rated on a six-point Likert scale; higher scores reflect more problems. Over a 4-month interval and across different interviewers, the test-retest correlations of subscales were above 0.6 for each subscale. Internal consistency reliabilities (Cronbach alpha) exceeded 0.8. In this analysis, each scale score was sorted into quartiles.
Depression and anxiety were assessed by self-report items that mapped onto DSM-III-R criteria for major depression, overanxious disorder, and separation anxiety disorder. Items were drawn from existing child self-report measures, including the Children’s Depression Inventory (M. Kovacs, unpublished manuscript, 1983) and the Revised Children’s Manifest Anxiety Scale
(28) . Children reported the frequency of problems over the preceding 2 weeks. To address minor assessment refinements introduced between cohorts, scores for depression and anxiety problems were computed by summing and then dividing the sum by the number of items separately for each cohort (Cronbach alpha for each cohort’s scale exceeded 0.8). Children scoring above the median on
both of the scales were categorized as high on anxious or depressive mood; all others were categorized as low. We probed for cohort differences and found none. Missing self-reports on this measure occurred for children whose parents refused participation or for children who were absent from school on the scheduled assessment dates.
Statistical Analysis
To evaluate associations between childhood antecedents and exposure to traumatic events, we used contingency tables and logistic regressions. We then used multinomial logistic regressions to evaluate associations of childhood antecedents with exposure to two types of traumatic events, assaultive violence and other (i.e., traumas that do not involve assaultive violence). In these models, the outcome variable was coded as a categorical response with four categories: 1) never experiencing a traumatic event up to young adulthood (N=297); 2) having experienced assaultive violence only (N=75); 3) having experienced only traumatic events that did not involve assaultive violence (N=599); and 4) having experienced events of both types (N=727). To estimate the associations between childhood antecedents and PTSD associated with the worst traumatic event, we used logistic regression. Analysis of antecedents of PTSD was conducted on the subset that reported exposure to one or more traumatic events. We tested additional models that included covariates to adjust for gender, cohort, race, family disadvantage (single mother, low education of adult in household), as well as all the childhood antecedents under study. For each childhood antecedent we included a category that contained participants with missing data in order to stabilize the number of participants contributing information to the multiple regression analyses, as shown in
Table 1 . To accommodate the initial sample design (clustering of students within schools), a variant of the Huber-White sandwich estimator of variance was used to obtain robust SE estimates (STATA statistical software, release 8.0SE, 2000).
Results
Cumulatively, to young adulthood, the estimated occurrence of exposure to one or more DSM-IV qualifying traumatic events in this cohort of young adults was 82.5%. Within the total cohort, 47.2% experienced one or more traumatic events that involved assaultive violence; 91% of the participants who experienced assaultive violence also experienced other event types that did not involve assaultive violence (e.g., learning about the sudden unexpected death of a loved one). We found that the occurrence of traumatic events up to age 6–7 was less than 1%, and that age-specific occurrence rose markedly after age 15, with the highest rate observed between 16 and 18 years of age
(6) . These age-specific rates confirm the temporal sequence from childhood antecedents measured in first grade to later traumatic events and PTSD.
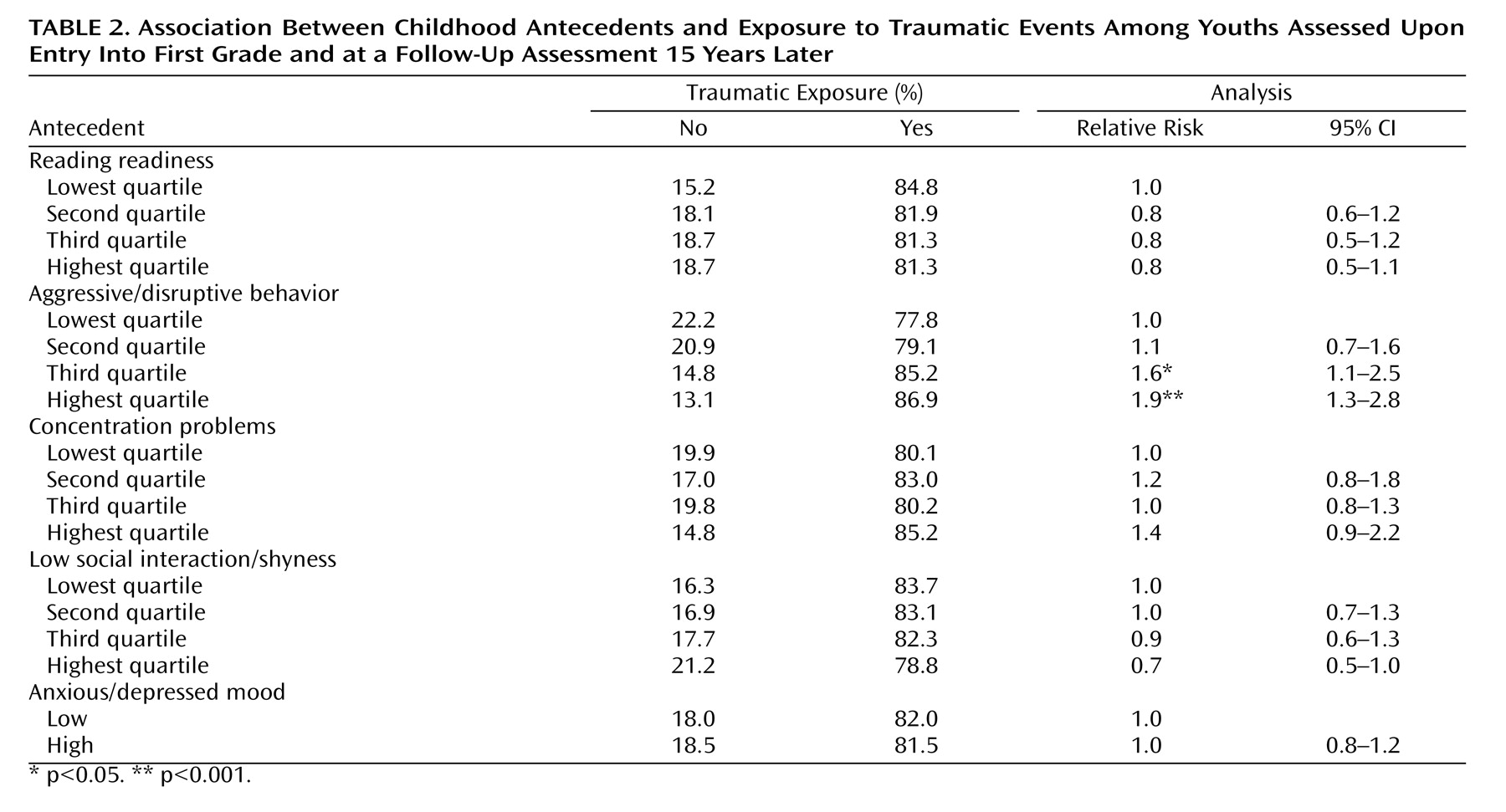
Table 2 presents percentages and relative risk estimates of exposure to any traumatic event across subgroups of the cohort defined by childhood variables. Children with teacher ratings of aggressive/disruptive behavior in the third and fourth quartiles were more likely to experience traumatic events by early adulthood. However, as can be seen in
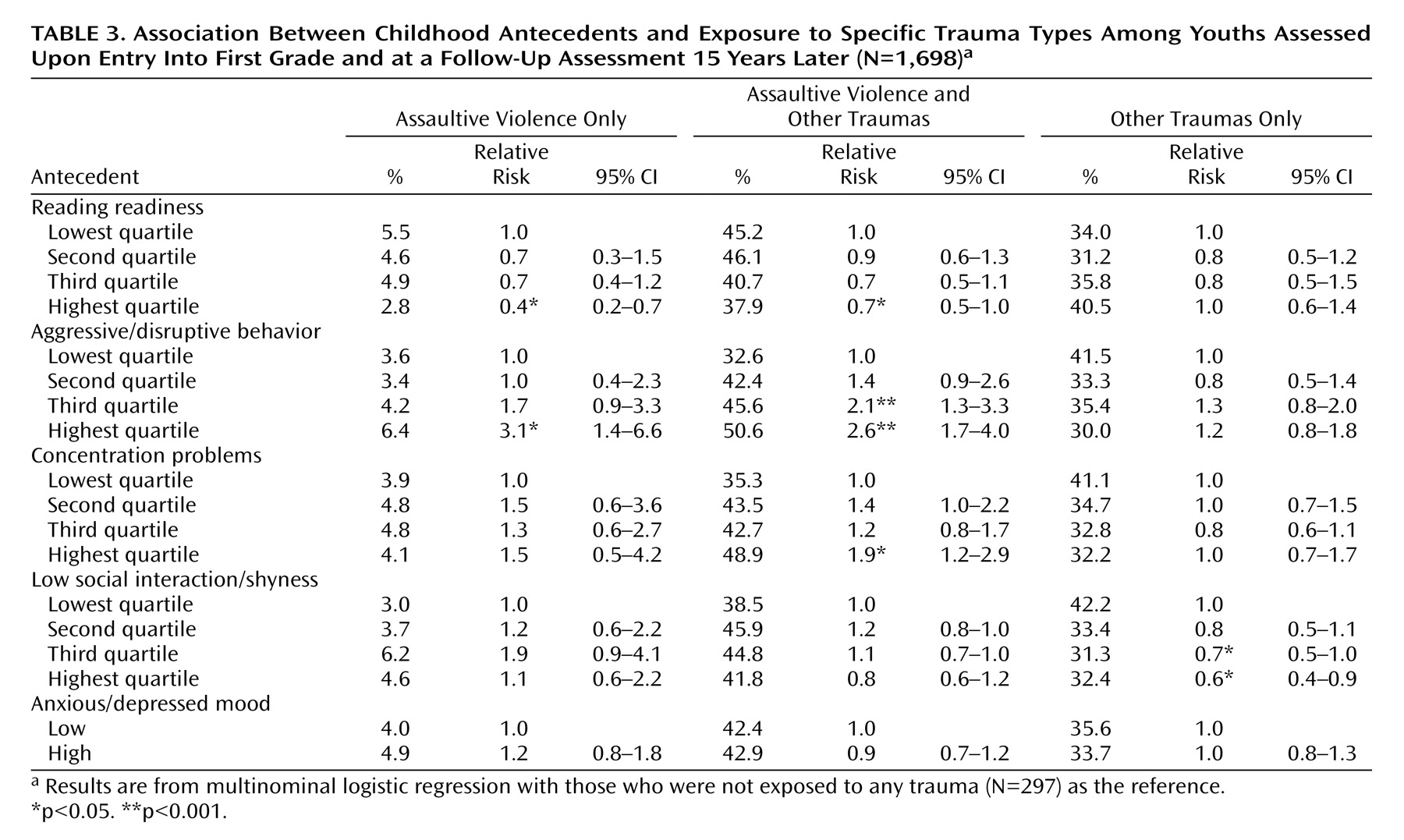
Table 3, the relationship of childhood factors with subsequent exposure varied between the two categories of traumatic events. High levels of aggressive/disruptive behavior in first grade were associated with increased risk for exposure to assaultive violence (alone or together with other traumas) but not with exposure to other event types in the absence of exposure to assaultive violence. Teacher ratings of a high level of aggressive/disruptive behavior (third and fourth quartiles) signaled approximately a doubling of risk for being exposed to an assaultive violence traumatic event.
In addition, reading readiness and concentration problems in first grade predicted exposure to assaultive violence but not to other types of traumatic events. Specifically, children who scored in the highest quartile of reading readiness were less likely to experience assaultive violence than children scoring in the lowest quartile. Children whose ratings on concentration problems placed them in the highest quartile were at increased risk for exposure to assaultive violence. We also found that low social interaction/shyness (teachers’ ratings in the fourth quartile) was associated with a lower risk for exposure to nonassaultive events only. Multivariable regression models, which included all variables in the Table plus indicators of family disadvantage (single mother, low education of adult in household), yielded similar results, although the confidence intervals for the estimates were larger.
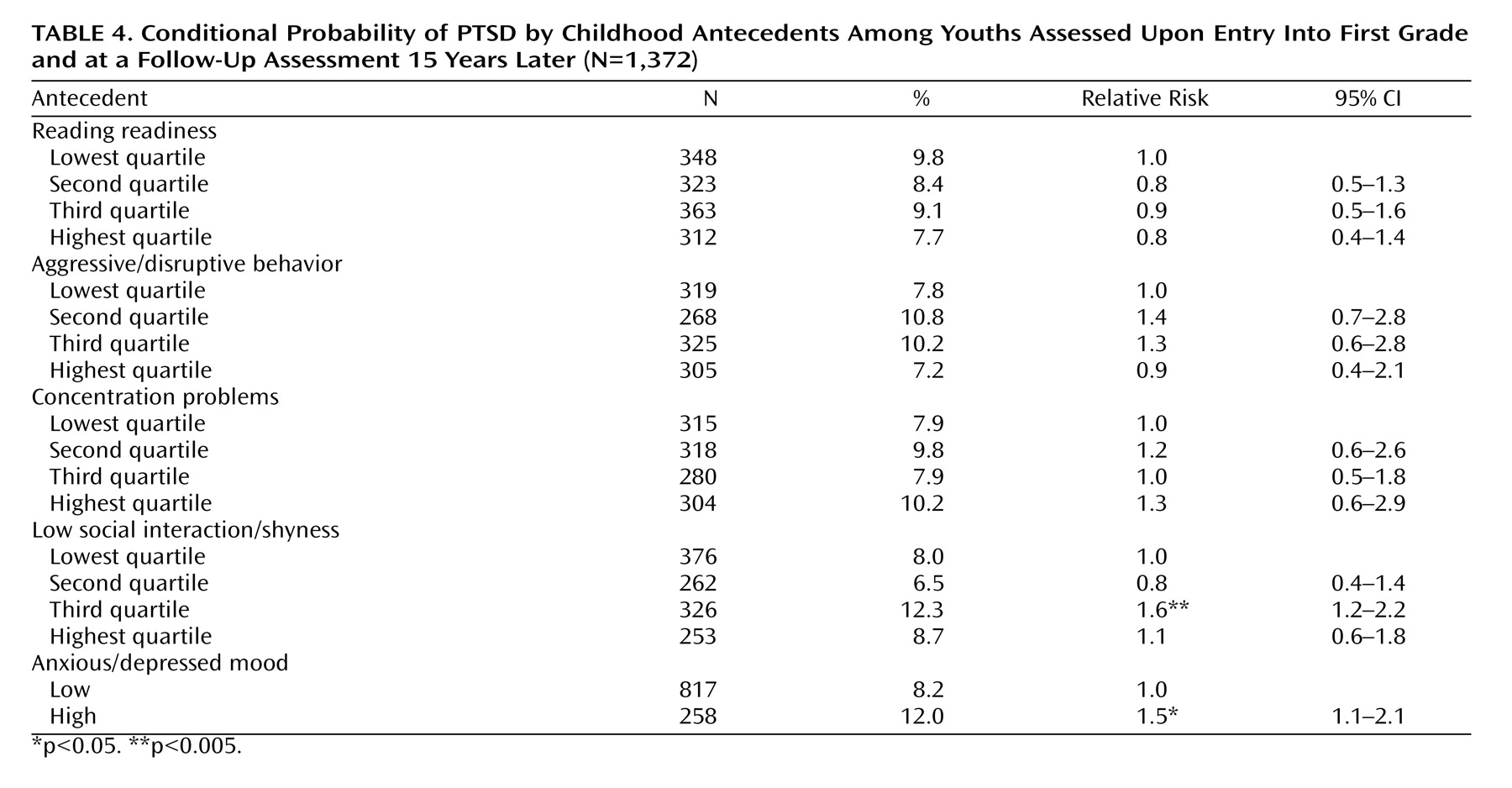
Of those who experienced any traumatic event, the estimated occurrence of PTSD was 8.8% (SE=0.8). In analyses of the conditional probability of PTSD given exposure to one or more qualifying events, there were 121 cases of PTSD, which diminished statistical precision and power, compared with analysis of exposure to trauma. Reading readiness and behavioral problems were not associated with the risk of PTSD given exposure (
Table 4 ). High levels of anxious or depressive mood in the first grade were associated with a 1.5-fold greater risk of PTSD among those exposed to traumatic events. After statistical adjustment for covariates—cohort, gender, race, family disadvantage, trauma type, and other childhood antecedents—the resulting estimate was slightly attenuated and less precise (relative risk=1.4, 95% CI=0.9–2.3; p<0.14).
Discussion
There were three key findings of this prospective analysis. 1) Young adults with high teacher ratings of aggressive/disruptive problems soon after entry to primary school were more likely to experience traumatic events that involved assaultive violence, but not other event types, and not PTSD following exposure to a traumatic event. 2) In contrast, young adults with high levels of depressed and anxious feelings in first grade were 1.5 times more likely to experience PTSD in response to a traumatic event but were not more likely to experience traumatic events by young adulthood. 3) Young adults whose reading scores in the first grade were in the highest quartile were at lower risk for exposure to assaultive violence.
The evidence on the prospective relationship between childhood conduct problems and the risk for exposure to assaultive violence provides firm support for previous results from retrospective data on Vietnam veterans and civilian samples of adults
(9,
18) . In a previous study, we found that exposure to traumatic events that involve assaultive violence is highest in late adolescence and is more prevalent among residents of urban areas versus residents of suburban areas
(8) . It is noteworthy that in this cohort of young adults who have grown up in an urban environment, classroom misconduct rated by teachers at the start of schooling was linked to the risk of exposure to assaultive violence.
In contrast with exposure to assaultive violence, exposure to other traumatic events (in persons who have experienced no assaultive violence events) was unrelated to childhood behavior problems or cognitive abilities. Previous epidemiological studies that reported on conduct problems and low intelligence as risk factors for exposure to traumatic events did not distinguish between types of traumatic events
(20,
21) .
With respect to susceptibility to the PTSD effects of exposure, the results extend previous findings on preexisting major depression and anxiety disorders, in that high levels of depressive and anxious problems (as opposed to disorders) at the start of first grade were shown to predict an increased risk of PTSD following exposure to traumatic events. A previous report on this cohort showed that depressive and anxious problems at the time of entry into primary school constituted early signs of major depression and anxiety disorders
(29) . Thus, the results of this analysis show that early childhood depressive and anxious problems identify children at risk not only for major depression and anxiety disorders but also for PTSD in response to traumatic experiences.
The interpretation of the results should take into account several limitations. First, participation at follow-up in young adulthood, although high for prospective studies from childhood to adulthood, was incomplete (75%). Second, the assessment of PTSD was conducted by nonclinicians, who used a structured interview without access to supplementary information that might be elicited by clinicians. However, the structured interview and the assessment procedure had been evaluated against blind clinical assessments, yielding high estimates of concordance
(25) . Third, we used standardized tests of reading readiness at school entry, which do not capture cognitive abilities as well as standardized intelligence tests do. Other studies have found robust associations, not only with exposure but also with PTSD, using standardized intelligence tests
(20,
21) . Construct and criterion validity have been established for the components of the Teacher Observation of Classroom Adaptation–Revised
(27) . The aggressive/disruptive behavior items from this instrument were very similar to those used in the teacher version of the Child Behavior Checklist developed by Achenbach
(30) . Previous reports on the Teacher Observation of Classroom Adaptation–Revised documented that ratings of aggressive/disruptive problems at baseline increased the risk for conduct disorder, antisocial personality disorder, or a juvenile or adult arrest
(31 –
33) .
Several strengths deserve mention. Most important are the community-based cohort and the longitudinal study design, which followed children from age 6 to young adulthood. Although there are a handful of studies that have examined risk factors for exposure or PTSD prospectively, they covered periods in adulthood
(15,
34) . There is a clear methodological advantage for assessing suspected causal determinants of PTSD and exposure to traumatic events in childhood, before their measurement reflects the influence of experiences that might be shaped, in part, by stressful experiences. Assessment of conduct problems at the start of schooling represents more faithfully early predispositions, compared with the assessment of conduct problems in adolescence, when they are increasingly influenced by the environmental responses they have elicited, as proposed in a model of conduct disorder in relation to early neurodevelopmental deficits
(35) .
The results suggest potential risk factors for PTSD that can be identified early in life and might be amenable to interventions. The generalizability of the results, which highlight the suspected causal role of childhood conduct problems in exposure to assaultive violence and the role of early depressive/anxious problems in PTSD, deserve testing in longitudinal studies of other populations. Our findings suggest that children reporting emotional problems in the first grade of school might be vulnerable to PTSD, although the extent of the elevated risk is modest. Future analyses of data from this study will attempt to elucidate further who is at risk by tracing the developmental trajectories of cognitive abilities, conduct problems, and emotional problems throughout the elementary school years.