Syphilis is an infection caused by the bacterium Treponema pallidum that has shown decreased prevalence because of the advent of penicillin (
1). If the disease remains untreated, syphilis progresses through three stages. Primary syphilis involves development of a chancre about 2 to 3 weeks after exposure, and secondary syphilis is characterized by lymphadenopathy, fever, CNS involvement, and rash on the palms and soles that appears weeks to months after infection. Tertiary syphilis is an inflammatory process that can cause granulomatous tissues to form in the cardiovascular or central nervous system 1 to 30 years after exposure. The illness may remain latent for years in between stages (
1). Neurosyphilis itself can be further broken down into an early stage involving meningeal and vascular structures and a late stage affecting the parenchyma of the brain and spinal cord (
1,
2).
Some of the psychiatric symptoms that have been described in untreated neurosyphilis patients include personality changes, aggressive behaviors, mania, auditory and visual hallucinations, illusions, frank paranoia, progressive cognitive impairment often leading to loss of employment, delirium, and persecutory delusions (
1–
7). Because of early treatment, only about 10% to 15% of primary syphilis cases progress to tertiary syphilis, and of these cases, less than 20% present with primary psychiatric symptoms (
3). For these reasons, the diagnosis of neurosyphilis is often overlooked.
Few journal articles and case reports in the current literature describe psychosis as the first manifestation of syphilis. In fact, many patients over age 45 who present as psychotic are diagnosed with late-onset schizophrenia. Late-onset schizophrenia accounts for 15% to 20% of all diagnoses of schizophrenia and is typically associated with better premorbid functioning, fewer negative symptoms, and less severe neurocognitive impairment, compared with schizophrenia that presents at an earlier age (
8). Late-onset schizophrenia usually responds to lower doses of antipsychotics, compared with higher doses.
Case Report
Ms. A was a 67-year-old female with a medical history significant for hypertension, controlled diabetes, chronic obstructive pulmonary disease, and misdiagnosed late-onset schizophrenia who presented to inpatient psychiatry under a temporary detention order because she was displaying bizarre behavior and responding to internal stimuli. She also appeared to be quite paranoid, carrying knives around with her for protection. Her symptoms were first noticed 8 years before, and she had been admitted to an outside psychiatric facility seven times over the past 2 years with a similar presentation. Ms. A was misdiagnosed with late-onset schizophrenia and had been treated with risperidone, haloperidol, and paliperidone. Her symptoms only minimally improved with antipsychotic treatment each time, and she had a history of noncompliance with medication in the outpatient setting, because she did not believe she had a psychiatric illness. Over 8 years, Ms. A's symptoms continued to worsen to the point where she could no longer maintain employment. She retired at age 62 and moved in with family members.
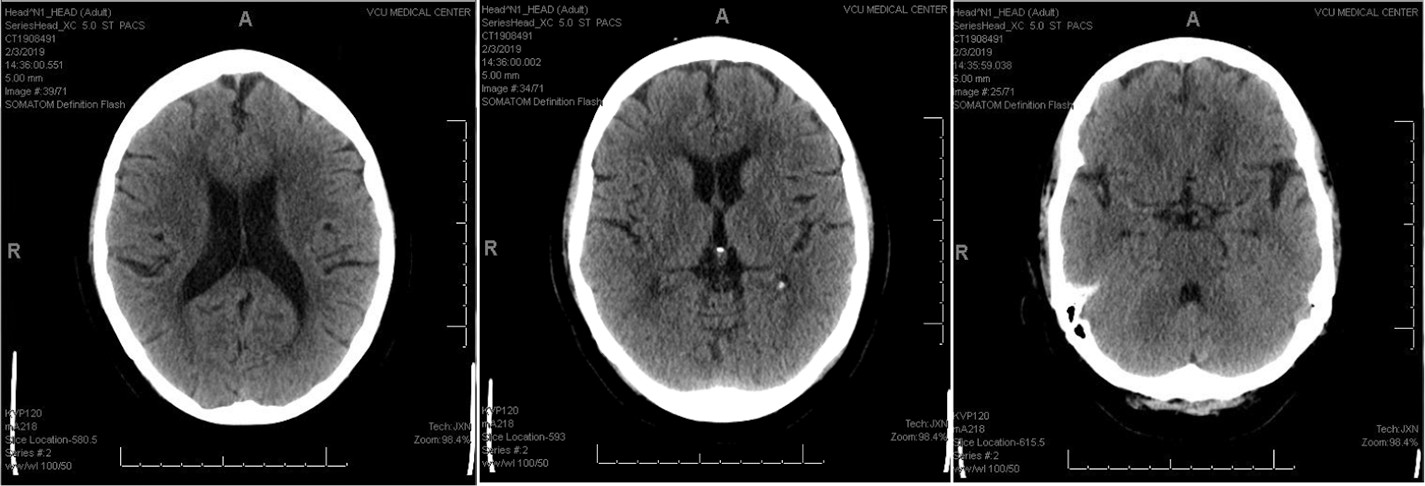
The differential diagnosis for the case was initially broad and included late-onset schizophrenia, schizoaffective disorder, unspecified psychosis, substance-induced psychosis, HIV-associated psychosis, hepatic encephalopathy, neurosyphilis, and other venereal diseases. Basic psychiatry screening labs, including complete blood count, basic metabolic panel, thyroid-stimulating hormone, lipid panel, liver function tests, hemoglobin A1c, urinalysis, and drug screen, were ordered when the patient was admitted. Given that Ms. A's symptoms did not manifest until age 60, further testing was ordered, including syphilis immunoglobulin G, HIV, hepatitis C, gonorrhea, chlamydia, trichomonas, and computerized tomography (CT) imaging of the head. Syphilis testing was found to be reactive, with rapid plasma reagin titer of >1:256. A noncontrast head CT showed nonspecific subcortical and periventricular white matter hypodensities (
Figure 1). The basic psychiatry labs noted above and HIV, hepatitis, and other sexually transmitted disease testing were all negative.
Ms. A's psychotic symptoms were addressed pharmacologically by starting paliperidone and titrating to 6 mg daily. She was overall calm and cooperative while interacting with staff members on the psychiatric unit. However, she was frequently observed responding to internal stimuli and smiling inappropriately when she thought she was alone. The patient was quite guarded and generally a poor historian. When she was told about her diagnosis of syphilis, Ms. A stated she thought she had syphilis a few years ago, but she could not recall for sure. Her family was unable to confirm or deny a prior diagnosis of syphilis.
To solidify a diagnosis of neurosyphilis, a lumbar puncture was performed by the neurology consult team. On venereal disease research laboratory testing, cerebrospinal fluid (CSF) was found to be reactive, with a titer of 1:4. The patient was then transferred to a medical specialty unit where she was started on 4 million units of intravenous penicillin every 4 hours for the treatment of neurosyphilis. A peripherally inserted central catheter line was placed for ease of treatment, and she completed a 12-day course of antibiotics. At the time of discharge from the medical unit, Ms. A was no longer displaying any paranoid behaviors nor was she speaking about any overt delusions. She was discharged home with family after completion of penicillin treatment and after being reevaluated by psychiatry. Oral paliperidone 6 mg daily was prescribed at discharge. Ms. A was advised to follow up with both her local outpatient psychiatrist and her primary care provider for further syphilis-related management.
Discussion
It is important to consider a wide differential in the case of an elderly patient who presents with psychosis as a primary symptom, including organic diseases such as neurosyphilis. Some aspects of Ms. A's case did fit with a diagnosis of late-onset schizophrenia, particularly her psychotic symptoms starting after age 45, female gender, few negative symptoms, and good premorbid functioning (
8). There was the possibility that she developed both late-onset schizophrenia and neurosyphilis. However, the positive serum and CSF testing, as well as Ms. A's minimal improvement with antipsychotic treatment, suggested that her symptoms were more likely the manifestation of neurosyphilis.
Because tertiary syphilis is quite indolent and can remain dormant for years, the patient may have been originally exposed to the disease up to 30 years earlier. Neither Ms. A nor her family could confirm whether she had previously been diagnosed with syphilis. Her symptoms likely worsened over 8 years because the infection went untreated. In contrast to Ms. A's poor response to antipsychotics, her symptoms appeared to have responded well to neurosyphilis treatment, which typically includes 18 to 24 million units per day of aqueous crystalline penicillin for 10 to 14 days through intravenous administration (
4,
9). After 12 days of intravenous penicillin, she was no longer responding to internal stimuli or smiling inappropriately.
Although a positive response was seen with intravenous penicillin treatment, it was important to ensure that the patient follow up with primary care and neurology as well as psychiatry. The overall prognosis for patients with neurosyphilis is poor. Only some patients experience resolution of psychotic symptoms after intravenous penicillin treatment; the cure rate is estimated to be about 60% (
5,
8). Patients may require serial laboratory monitoring (or lumbar punctures) every 6 months for a span of 2 years (
10). If CSF white blood cell count or serum venereal disease research laboratory levels do not decrease fourfold or normalize by the end of 2 years, then a proper treatment response has not occurred and retreatment is considered (
7,
9). Additionally, some case reports have found that neurosyphilis patients who present as psychotic do not have a good prognosis for symptom resolution (
1,
2,
5). In these cases, continuation of antipsychotic treatment may be necessary. However, if a patient continues to do well and no longer displays psychosis, antipsychotic treatment should be discontinued, given potential adverse effects from psychotropics.
The case of Ms. A helps to demonstrate that we must consider medical causes when evaluating new-onset psychosis in an older patient, especially when symptoms do not improve with antipsychotic treatment. The diagnosis of neurosyphilis is rare, but about 60% of patients respond well with intravenous penicillin treatment if providers correctly diagnose the etiology. If additional testing had not been ordered for organic causes of psychosis, Ms. A likely would have continued the pattern of psychiatric admission, medication noncompliance, and worsening of symptoms. Neurosyphilis is not an infection to be missed.
Key Points/Clinical Pearls
Acknowledgments
Dr. Nutile thanks Tushar Thakre, M.D., and Katie Adams, Pharm.D., who assisted by providing editing suggestions.