The Surgeon General’s recent report on mental health
(1) emphasized the high rates of mental disorders in the United States and pointed out that many who suffer from these disorders do not receive mental health treatments that have been shown to be efficacious. It has been well established that persons with common mental disorders such as depression or anxiety are frequent users of general medical services
(2,
3), but little is known about their use of alternative medical services. If a substantial unmet need for mental health care exists, then persons with mental illness might be expected to turn for help to alternative providers or therapies outside the formal health care system. The study reported here examined the use of complementary and alternative medicine among survey respondents who met criteria for a number of common mental disorders. The study used data from a large national survey of 9,585 adults.
Typical problems for which persons see alternative providers include back problems, anxiety, headaches, insomnia, depression, arthritis, and allergies
(4,
5). Several recent studies have suggested high rates of depression or anxiety among users of alternative medicine
(4,
6–
10). Eisenberg et al.
(7) found that 40.9% of the adults who reported severe depression and 42.7% of those who reported anxiety attacks had used alternative therapies in the past 12 months, compared with 28.2% of adults in the overall sample. Druss et al.
(11) found that major depression was a significant predictor of use of both antidepressants and nonprescription dietary supplements. Burstein et al.
(12) examined use of alternative medicine among women with early-stage breast cancer and found relatively high rates of depression among women who were new users of alternative medicine. Davidson et al.
(13) administered structured diagnostic interviews (Structured Clinical Interview for DSM-III-R) to 83 users of complementary and alternative medicine services in the United States and the United Kingdom. The majority (69%) met lifetime criteria for an axis I disorder, and 40% met criteria for a current axis I disorder, most frequently an anxiety or depressive disorder. The authors concluded that individuals with depression or anxiety disorders may be particularly interested in pursuing alternative medicine services and called for greater awareness of the possibility of psychiatric illness in persons who seek help from the complementary medicine sector.
Most studies of the relationship between mental disorders and use of alternative medicine have used small and nonrepresentative samples or have used simple self-reports of the presence or absence of mental disorders, rather than more standardized interviews. In the study reported here, we used a household sample and included standardized screening measures for specific psychiatric disorders to examine the association between mental disorders and the use of alternative medicine, while controlling for potentially confounding demographic and health status factors. We hypothesized that respondents with common mental disorders such as depression or anxiety would have higher rates of complementary and alternative medicine use.
Results
Of the total of 9,585 respondents who agreed to participate in the telephone survey for this study, 19 answered “don’t know” or refused to answer the question about use of complementary and alternative medicine. Of the remaining 9,566 respondents, 1,576 reported use of alternative medicine in the past 12 months, resulting in an unweighted proportion of 16.5%. After weighting, we estimated the prevalence of the use of alternative medicine to be 14.5%. From this point on, we present only weighted proportions.
Among those who reported using alternative medicine, 15.0% reported that they had used it to treat mental or emotional problems, 45.4% reported at least one visit to an alternative medicine practitioner, and 54.6% either self-administered alternative treatments or received treatments from a traditional health care provider (we do not have data to distinguish these two possibilities).
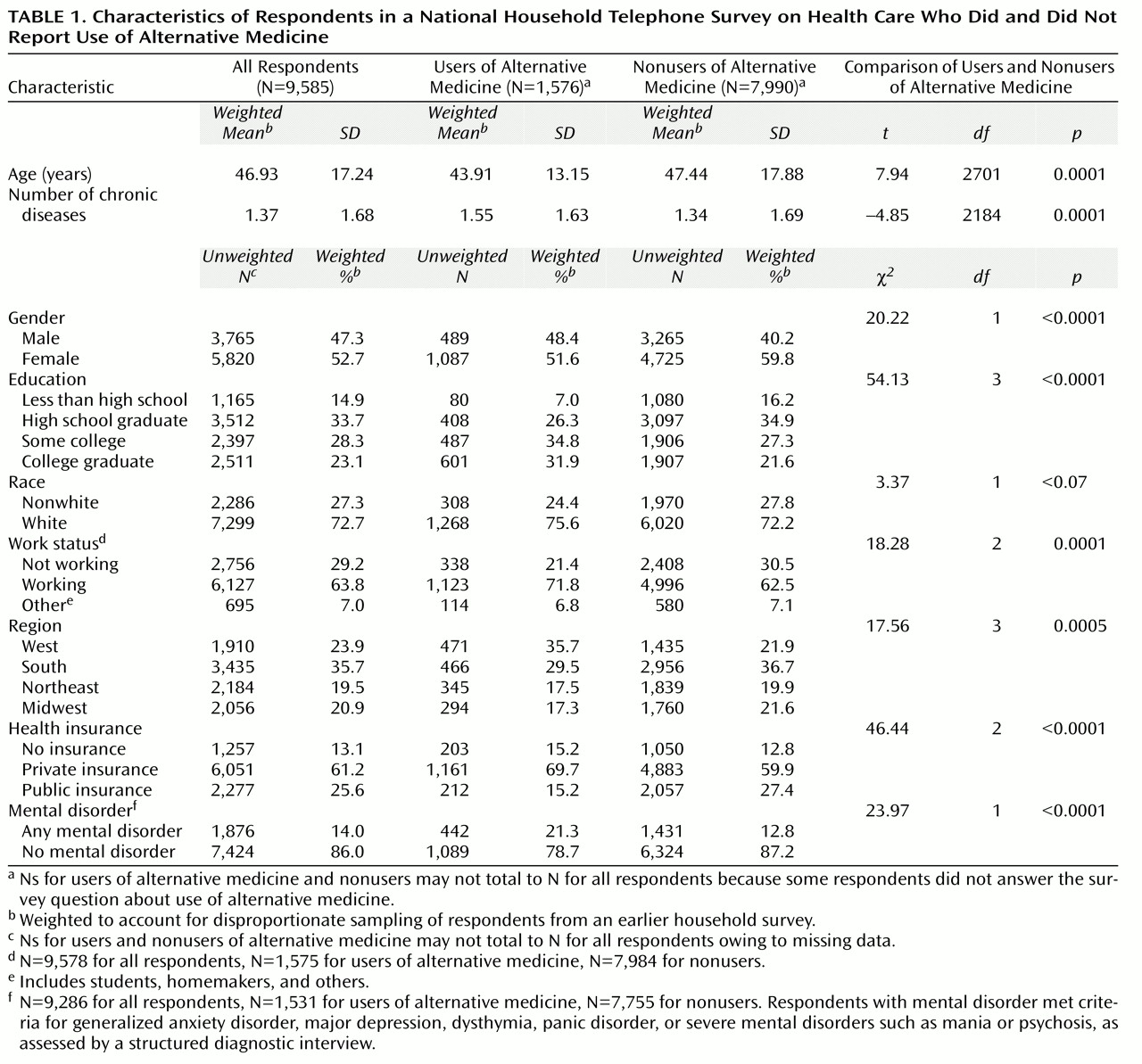
Table 1 shows the characteristics of the study participants and the differences between study participants who did and did not report use of alternative medicine in the 12 months before the study. Individuals who reported use of alternative medicine were significantly more likely to meet diagnostic criteria for at least one of the mental disorders we assessed.
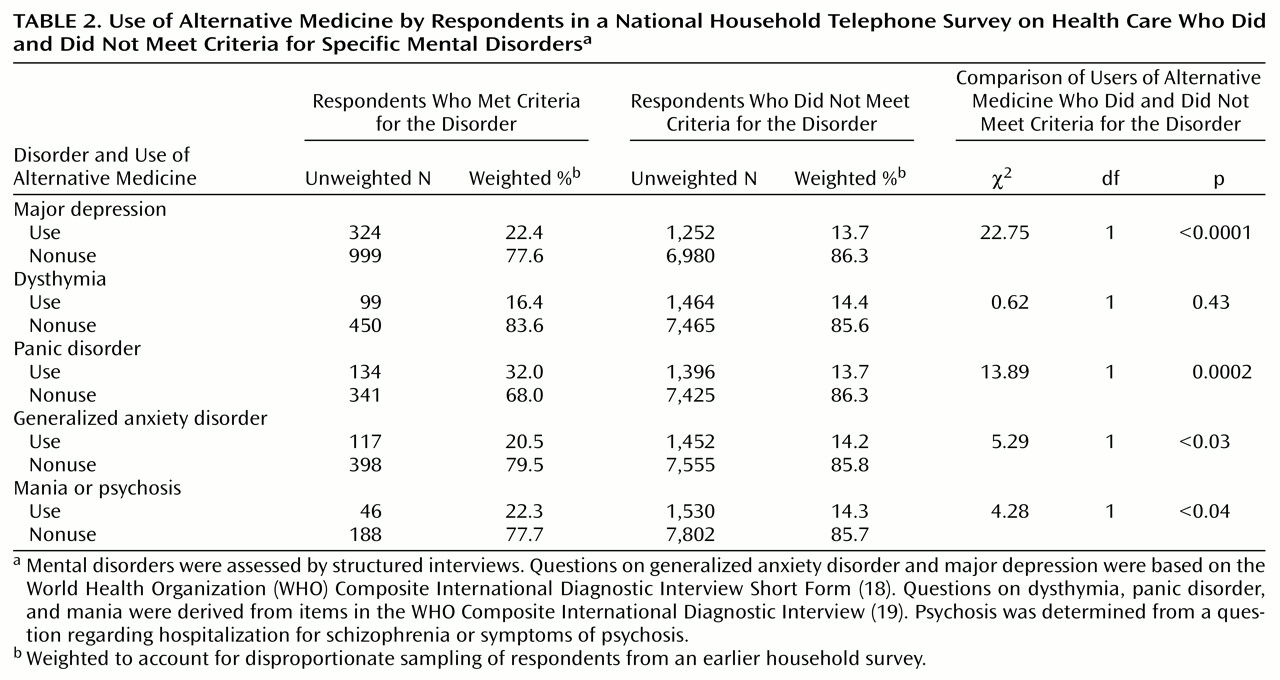
Table 2> shows the association between use of alternative medicine and each of the mental disorders we assessed. Use of alternative medicine was significantly more likely among respondents who met criteria for any of the disorders except for dysthymia. Respondents who met criteria for major depression and panic disorder were particularly likely to report the use of alternative medicine.
Respondents with more than one mental disorder were not significantly more likely to use alternative medicine than those who met criteria for just one disorder (22.4% versus 21.5%) (χ2=0.10, df=1, p=0.76). Use of alternative medicine was significantly higher among respondents who reported that they needed help with emotional or substance abuse problems in the past 12 months than among those who did not report needing such help (30.1% versus 12.7%) (χ2=86.31, df=1, p<0.001).
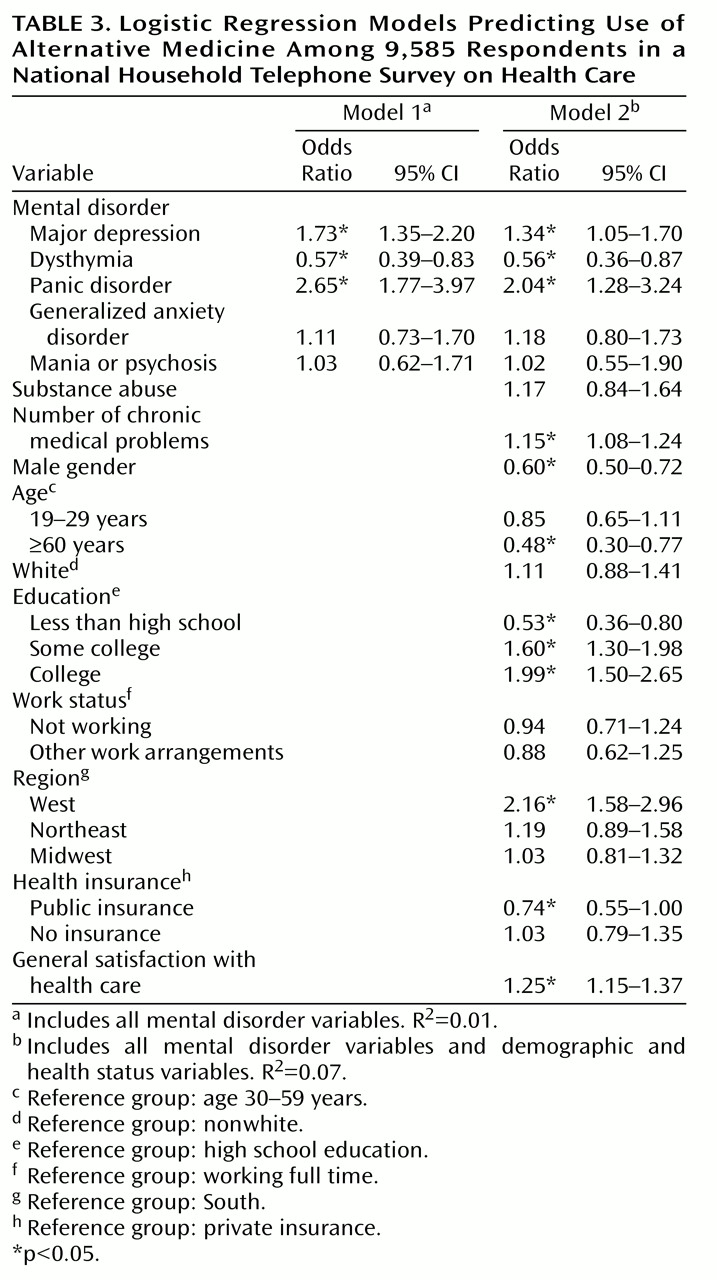
After controlling for all mental disorders in our logistic regression model (
Table 3, model 1), we found that major depression and panic disorder remained significantly associated with the use of alternative medicine. In addition, in the model that controlled for the other disorders, a significant association between dysthymia and use of alternative medicine emerged. In the full model that included all mental disorder diagnoses and demographic and clinical covariates (
Table 3, model 2), major depression, dysthymia, panic disorder, gender, age, level of education, geographic area, severity of chronic medical illness, type of insurance, and general satisfaction with health care were significantly associated with use of alternative medicine. When all other factors were controlled, participants with generalized anxiety disorder and with severe mental disorders (probable bipolar disorder or schizophrenia) did not have significantly higher rates of alternative medicine use than those without those disorders. Participants who met criteria for dysthymia were significantly less likely to report use of alternative medicine than those who did not meet those criteria.
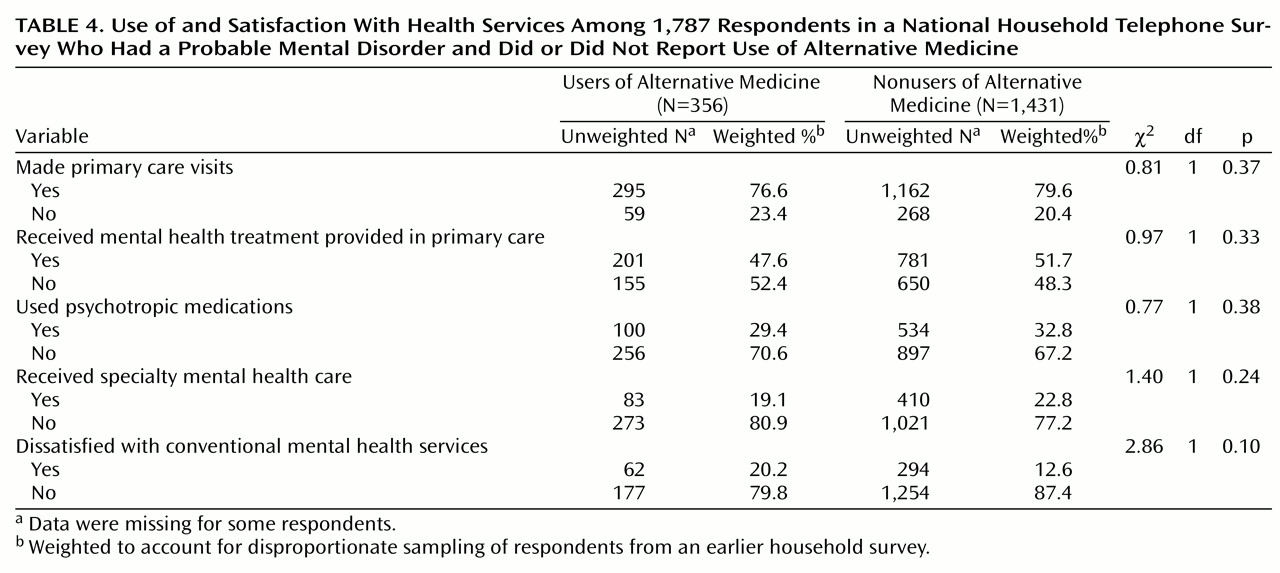
Table 4 shows the association between the use of alternative medicine, the use of conventional mental health treatments, and satisfaction with available mental health services among the 1,787 respondents who met criteria for at least one mental disorder and used any health services (primary, specialty, or alternative care) in the year before the survey. In this subgroup, respondents who used alternative medicine were as likely as those who did not to report having made primary care visits, having received mental health treatments in primary care, having used specialty mental health care, and having used psychotropic medications. All of the users of alternative medicine in this group also used at least one of the conventional mental health treatments we asked about (mental health treatment in primary care, a psychotropic medication, or specialty mental health care).
When we examined participants’ ratings of “health care available for personal or emotional problems during the past 12 months,” we found that 20.3% of those who used alternative medicine reported being dissatisfied, compared with 12.6% of those who did not use alternative medicine (χ2=2.86, df=1, p<0.10).
Among the 1,762 respondents who met diagnostic criteria for common mental disorders (anxiety or depressive disorders), those who used alternative medicine were more likely to have received appropriate treatment with psychotropic medications or counseling than those who did not use alternative medicine (50.1% versus 30.2%) (χ2=23.14, df=1, p<0.001).
Discussion
In our sample, about 21% of complementary and alternative medicine users met diagnostic criteria for at least one probable mental disorder (compared to about 13% of nonusers). About 15% of those who reported using alternative medicine said that they were using these services to help with emotional, mental, or substance abuse problems. This rate is consistent with the rates of 13% reported by Elder et al.
(23) and 11% reported by Kelner and Wellman
(24) but lower than the rates reported by Eisenberg
(4), who found that users of alternative medicine considered anxiety and depression some of the most common indications for the use of those services (for 28% and 20% of users, respectively). The discrepancy may be due to differences in the populations sampled, in the way we defined and elicited information about alternative medicine use, or in the way we elicited the reason for alternative medicine use.
Our findings suggest that practitioners of alternative medicine should be aware that a considerable number of their patients may be suffering from common mental disorders such as major depression or panic disorder. For these patients, consultation and collaboration with a specialty mental health practitioner should be strongly considered if they do not respond to alternative medicine treatments as expected. We also encourage all primary care providers and mental health specialists who are treating patients with major depression and anxiety disorders to inquire about the use of alternative treatments. Clinicians’ knowledge of such treatments and, when indicated, coordination with providers of alternative medicine might improve overall health care for these patients and prevent potentially harmful interactions between conventional and alternative treatments
(25,
26).
When we examined use of alternative medicine among individuals with specific mental disorders, we found relatively high rates of use among individuals with major depression and panic disorder, even after the analysis adjusted for comorbid mental disorders and demographic and health status variables. In addition, after this adjustment, the associations between use of alternative medicine, generalized anxiety disorder, and severe mental disorders were no longer significant, and individuals with dysthymia were actually significantly less likely to report use of alternative medicine. However, these results may be due to relatively high rates of comorbidity between these disorders.
Our research also confirmed previously identified associations between use of alternative medicine and number of factors, such as female gender, middle age, a higher level of education, a higher level of medical illness, and residence in the Western part of the United States
(7,
24,
27,
28).
Our overall estimates of alternative medicine use are lower than those previously reported
(4,
7,
20,
27,
29,
30) but higher than the rate reported by Druss and Rosenheck
(31). The discrepancy may be due to differences in the populations studied and the definitions of complementary and alternative medicine used. For example, we did not include chiropractic medicine in our definition of alternative medicine, as this treatment is now covered by a large number of health insurers and most states have health insurance mandates to cover chiropractic care
(28).
Our study sampled a larger population than most previously reported surveys about alternative medicine, but the data we collected have some limitations. We relied on respondents’ recall of services used over a 12-month period, and this long recall period may have resulted in some underreporting of alternative medicine use. We provided a definition of alternative medicine, but we relied on respondents to classify treatments they were reporting as “alternative.” We did not collect detailed information on why respondents used alternative medicine except for asking if the services had been used to treat mental or emotional problems. A number of theories for the use of alternative medicine have been advanced in earlier studies
(5,
24,
29,
30,
32–
35), and we cannot add to this discussion.
We did not collect detailed information about what specific types of alternative medicine treatments were used. We did collect information about medications taken several times a week for at least 1 month in the past year, and we found that 3.7% of the respondents with probable depression or dysthymia reported the use for at least 1 month of St. John’s wort (hypericum), an over-the-counter herbal product for which there is some empirical evidence of efficacy
(36–
38). We cannot determine from our data if the use of this compound represented self-use or was recommended by a traditional or alternative health care provider. Additional research should examine the nature of the alternative medicine treatments used by individuals with mental disorders in greater detail. It would, for example, be important to know whether people are using alternative treatments for which there is some evidence of efficacy.
Most users of alternative medicine also use conventional medical treatments, and some researchers
(31) have suggested that alternative medicine is used as a complementary treatment to conventional health care rather than as a substitute. In our study, users of alternative medicine who met criteria for mental disorders were as likely to use primary care or conventional mental health treatments as those who did not use alternative medicine. All respondents who met probable diagnostic criteria for mental disorders and reported using alternative medicine also reported using at least one of the conventional mental health services we asked about, suggesting that, in this sample, use of alternative medicine was indeed complementary to conventional treatments. Persons with high levels of psychological distress may be more likely to use a range of available treatments, including conventional mental health and alternative medicine treatments.
Alternative medicine users with probable depressive or anxiety disorders were somewhat more likely to receive conventional mental health care that met criteria for appropriate care than were those who did not use alternative medicine. On the other hand, respondents with probable mental disorders who used alternative medicine reported a somewhat lower level of satisfaction with available mental health services than those who did not, although the difference was not statistically significant. It is possible that patients with mental disorders attempt to get help in the conventional medical sector and then turn to alternative medicine if they feel that they have not been helped by conventional medicine. However, our cross-sectional data do not allow us to adequately test this hypothesis.
In summary, we found relatively high rates of use of complementary and alternative medicine in individuals with common mental disorders, particularly major depression and panic disorder. Further research is needed to examine the nature and quality of alternative medicine treatments used by persons with mental disorders and to determine whether these individuals use alternative medicine treatments because conventional medical and mental health care does not properly address their health care needs. Such research may help us improve conventional medical services for these persons and may suggest ways of coordinating services across the conventional and alternative health care sectors to provide better care to patients.