There is controversy over whether patients with panic disorder have elevated risks for suicidal behavior. Although some investigators found high risks
(1), others found this accounted for by comorbid disorders
(2–
4). The vast majority of information has come from retrospective studies.
The Harvard/Brown Anxiety Research Program has prospective follow-up data on 498 subjects with current or past panic disorder at intake. In this article, we examine whether prospectively observed suicidal behavior was largely accounted for by comorbid psychiatric disorders and provide a quick screening method for suicide risk that uses information obtainable during an intake interview.
Method
The Harvard/Brown Anxiety Research Program is a prospective, naturalistic, longitudinal, multicenter study of 711 patients with DSM-III-R anxiety disorders. Inclusion criteria were at least one of the following DSM-III-R current or past diagnoses: panic disorder (with or without agoraphobia), agoraphobia without a history of panic disorder, generalized anxiety disorder, and social phobia. All subjects were at least 18 years of age. A signed written consent form was obtained from each subject. Exclusion criteria were the presence of an organic mental disorder, a history of schizophrenia, or psychosis within the last 6 months. Further details on referrals and assessment are described elsewhere
(5). In this article we examine 498 subjects with panic disorder.
The initial evaluation used items from the Personal History of Depressive Disorders
(6), the Yale Greater New Haven Health Survey–Community Interview—Wave 1
(7), the Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P)
(8), and the Schedule for Affective Disorders and Schizophrenia—Lifetime Version (SADS-L)
(9). Items from the SCID-P and SADS-L were combined to create the SCALUP
(10), an instrument in use for the intake evaluations. Specifically, affective disorders were diagnosed according to Research Diagnostic Criteria
(11), and anxiety and all other disorders were diagnosed according to DSM-III-R.
Follow-up was conducted every 6 months for 2 years and yearly thereafter. The Longitudinal Interval Follow-Up Evaluation
(12) was used to assess course of illness and psychosocial functioning. Personality disorders were assessed at the 12-month interview with the Personality Disorder Examination
(13). Information on suicide attempts or gestures before intake was collected via SCALUP (10). Suicidal behavior during follow-up was assessed with the Longitudinal Interval Follow-Up Evaluation.
Kaplan-Meier life tables were used to estimate probabilities of suicide attempts or gestures during follow-up. Because follow-up data are “censored” (that is, some subjects were lost to follow-up before the end of 5 years), the raw percentage of subjects who made suicide gestures or attempts differs from the probability at the end of the 5 years of follow-up. Variables associated with past histories of suicidal behavior were examined with Cox regression analysis to see if they were predictive of suicidal behavior during follow-up. Because the number of events was small, predictors were examined with univariate models. We also divided subjects into two groups according to risk factors assessed at intake: high-risk subjects (N=289) had any affective or eating disorder, current or past alcohol/substance use disorders, or past histories of suicidal behavior, and low-risk subjects (N=209) did not have these risk factors.
Results
The probability of suicidal behavior during the 5-year follow-up period was 0.06. Subjects with past suicidal behavior had a 0.30 probability of making an attempt, compared with a 0.04 probability for subjects without such histories. Only 43 (9%) of the 498 subjects had past histories of suicidal behavior; a 30% probability for 9% of the subjects, compared with a 4% probability for 91% of the subjects, translated into the majority (N=13) of the 25 suicide attempts during follow-up occurring in subjects with no previous history of suicidality.
Attempts were rated for seriousness of intent. For the 25 subjects who made attempts, the maximum level of intent for 10 subjects (40%) was no or minimal intent, 10 (40%) had definite or serious intent, three (12%) had very serious or extreme intent, and two (8%) completed suicide.
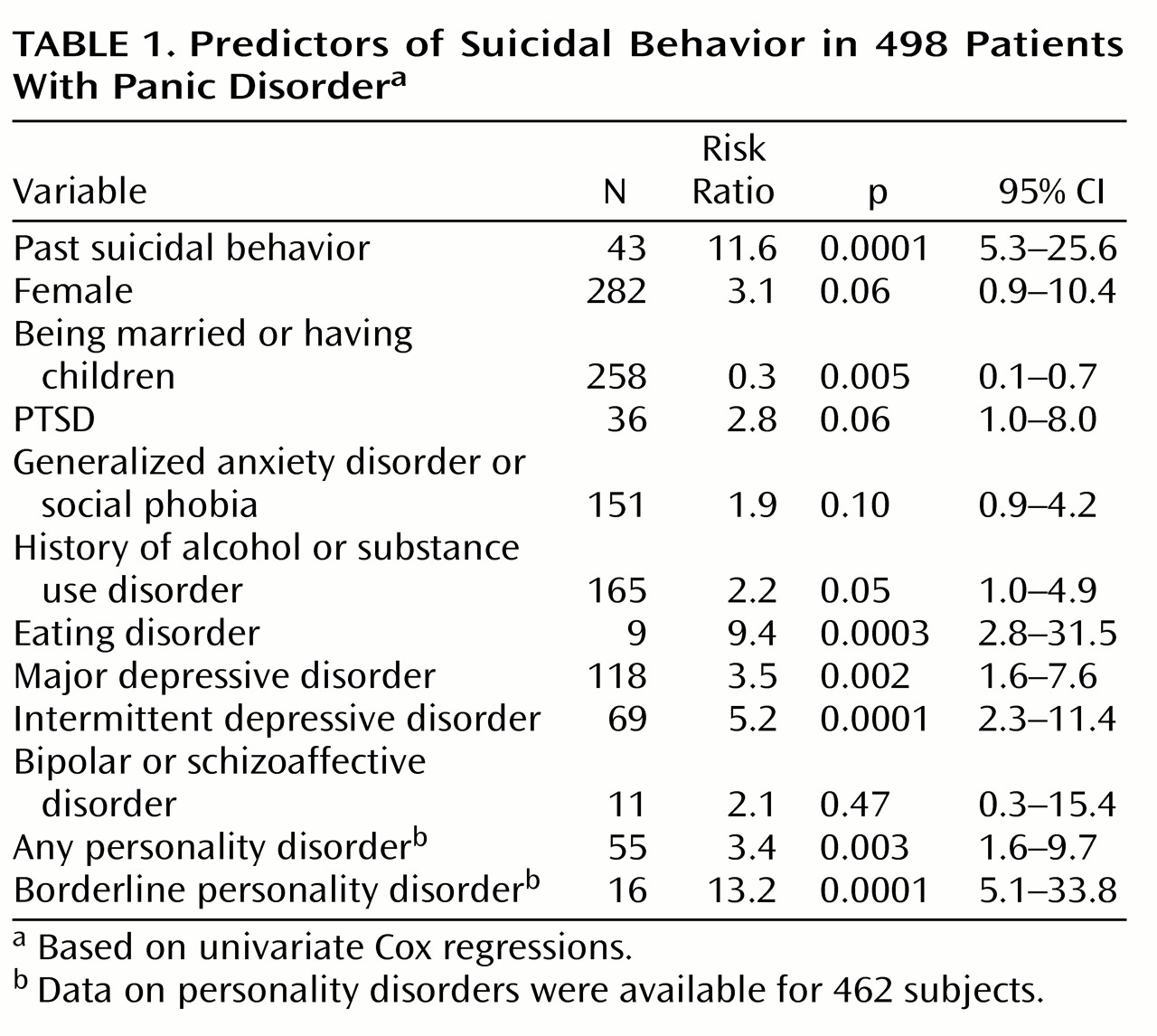
Table 1 summarizes Cox regression results for predictors of suicidal behavior. All variables had similar predictive value, as had been found in retrospective reports
(3); however, some effects were no longer statistically significant because of the small number of suicide attempts. Past suicidal behavior, current major depressive disorder, any personality disorder, borderline personality disorder, history of alcohol or substance use disorders, eating disorders, and intermittent depressive disorder were significant risk factors. Being married or having children was a protective factor.
We divided subjects into high-risk and low-risk groups using factors found both statistically and clinically significant in the previous analysis and easily assessed during initial contact. Subjects in episodes of affective or eating disorders, with current or past substance abuse, or with past suicidal behavior were categorized as high risk. Because personality disorders are difficult to diagnose in an initial assessment, they were not included in this measure.
The probability of making at least one suicide attempt during follow-up was 0.09 for high-risk subjects, compared with 0.01 for low-risk subjects (risk ratio=8.95, Wald χ2=8.83, p=0.003). Only two suicide attempts occurred in low-risk subjects; both of these subjects had developed major depressive disorder during follow-up before their suicide attempts.
Discussion
Our research supports previous findings that patients with panic disorder are not at high risk for suicidal behavior in the absence of comorbid disorders. However, because of high rates of comorbidity, it is important to assess patients with panic disorder carefully for the presence of other risk factors. Over half of the suicide attempts during follow-up were in subjects with no previous suicidal history.
Factors that can be assessed at initial clinical contact identified the vast majority of potentially suicidal patients: affective disorders, eating disorders, substance use disorders, or past suicidal behavior. We suggest that new patients with panic disorder be screened for these problems to assess their risk of self-harmful behavior. Borderline personality disorder is also associated with a dramatically elevated risk of suicide attempts or gestures and is therefore important to assess.
Our results suggest a quick method of assessing patients with panic disorder for risk of self-harmful behavior and underscore the need for follow-up. This study also supports previous findings that panic disorder is not predictive of suicide in the absence of other risk factors.
Acknowledgments
The Harvard/Brown Anxiety Disorder Research Program is conducted with the participation of the following investigators: M.B. Keller, M.D. (Chairperson); J. Eisen, M.D., K. Phillips, M.D., R. Stout, Ph.D. (Butler Hospital-Brown University School of Medicine); M.T. Shea, Ph.D. (VA Hospital, Providence-Brown University School of Medicine); M.G. Warshaw, M.S.S., M.A. (Massachusetts Veterans Epidemiology Research and Information Center, VA Boston Healthcare System-Boston University School of Public Health); R.M. Goisman, M.D. (Massachusetts Mental Health Center-Harvard University School of Medicine); G. Mallya, M.D. (McLean Hospital-Harvard University School of Medicine); F. Rodriguez-Villa, M.D. (Cambridge Hospital-Harvard University School of Medicine); M.P. Rogers, M.D. (Brigham and Women’s Hospital-Harvard University School of Medicine); R. Vasile, M.D. (New England Deaconess Hospital-Harvard University School of Medicine); A. Massion, M.D. (University of Massachusetts Medical Center); G. Steketee, Ph.D. (Boston University School of Social Work); K. Yonkers, M.D. (University of Texas, Dallas); I. Goldenberg, Psy.D.; and E. Fierman, M.D. Additional contributions from P. Alexander, M.D.; J. Curran, M.D.; J. Cole, M.D. (McLean Hospital-Harvard University School of Medicine); J. Ellison, M.D., M.P.H. (Harvard Pilgrim Health Care-Harvard University School of Medicine); A. Gordon, M.D., S. Rasmussen, M.D. (Butler Hospital-Brown University School of Medicine); R. Hirschfeld, Ph.D. (University of Texas, Galveston); J. Hooley, D.Phil. (Harvard University); P. Lavori, Ph.D. (Stanford University); J. Perry, M.D. (Jewish General Hospital-McGill University School of Medicine); L. Peterson (VA Hospital, Togus, Maine); J. Reich, M.D., M.P.H.; J. Rice, Ph.D. (Renard Hospital-Washington University School of Medicine); H. Samuelson, M.A. (Brigham and Women’s Hospital); D. Shera, M.S. (Harvard School of Public Health); N. Weinshenker, M.D. (New Jersey Medical School); M. Weissman, Ph.D. (Columbia University); and K. White, M.D.