Most studies support a three-fold higher risk for alcohol abuse or dependence (alcoholism) in the children of alcoholics as they reach adulthood
(1), but there is less agreement regarding problems likely to be seen earlier in life. Clinical syndromes potentially overrepresented include externalizing disorders such as conduct disorder and oppositional disorder; impairments in abstract reasoning, memory, and goal-directed behavior; problems in personal and social functioning; and excessive aggressiveness
(2–
6).
Several of these disorders are consistent with a diagnosis of attention deficit hyperactivity disorder (ADHD)
(7). High levels of motor activity and related behaviors can be relatively nonspecific symptoms, however, and are also seen with conduct disorder, the prodromal phase of the antisocial personality disorder. Thus, the association between ADHD and alcohol use disorders is not clear; negative results are more likely when the impact of conduct disorder is controlled for, although there are more consistent data regarding problems with other substances
(8–
11). Additional important methodological issues include the need to control for other comorbid disorders in subjects and relatives, comparability regarding socioeconomic status, and a lack of clear definitions for major psychiatric syndromes
(1,
12).
In this study we applied DSM-IV criteria to the offspring of carefully matched children of relatively highly functioning alcoholics without antisocial personality disorder and comparison subjects. Our hypothesis was that once additional characteristics are controlled for, children from alcoholic families will not have elevated rates of ADHD, conduct disorder, or oppositional disorder.
Method
Data were obtained after written informed consent was obtained from the parents of 162 children with a mean age of 11 years who were the offspring from an original study group of 453 sons of alcoholics and comparison subjects
(1,
13). The Caucasian and Hispanic men who were the fathers of the children in the current study entered the original study 15 years earlier as sons of alcohol-dependent fathers or as demographically matched comparison subjects whose fathers were not alcoholic.
During the follow-up, the mothers of these children reported on problems for children 7 years old and older during an interview with the Semi-Structured Assessment of the Genetics of Alcoholism
(14); the mothers also completed the Child Behavioral Checklist
(15). The children were not directly interviewed or observed.
The 162 children were divided into groups on the basis of their family history. Group 1 included 57 children (35%) with no alcohol dependence in their first-degree or second-degree relatives. Group 2 included 68 children (42%) with alcoholism in extended relatives only. Finally, group 3 included the 37 children (23%) with an alcoholic mother or father. In subjects with an alcoholic parent, 24 of the children had an alcohol-dependent father only, five had an alcohol-dependent mother only, and eight had two alcoholic parents. Only one mother had a relative with antisocial personality disorder, and, in cases where the mother was alcoholic, the birth of the child antedated the onset of alcoholism.
The chi-square statistic was used to evaluate categorical data across the three groups, Fisher’s exact test was used when groups 2 and 3 were combined into one group, and analysis of variance (ANOVA) was used for continuous variables across all three groups. Post hoc tests were applied to items with overall significant differences by ANOVA.
Results
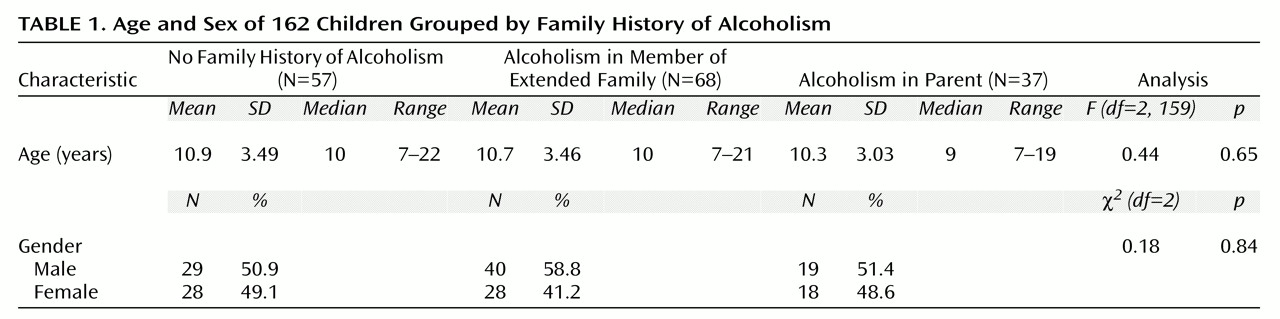
The mean age of the entire group of children (N=162) was 10.7 years (SD=3.37). Children in the three groups were comparable in gender and age (
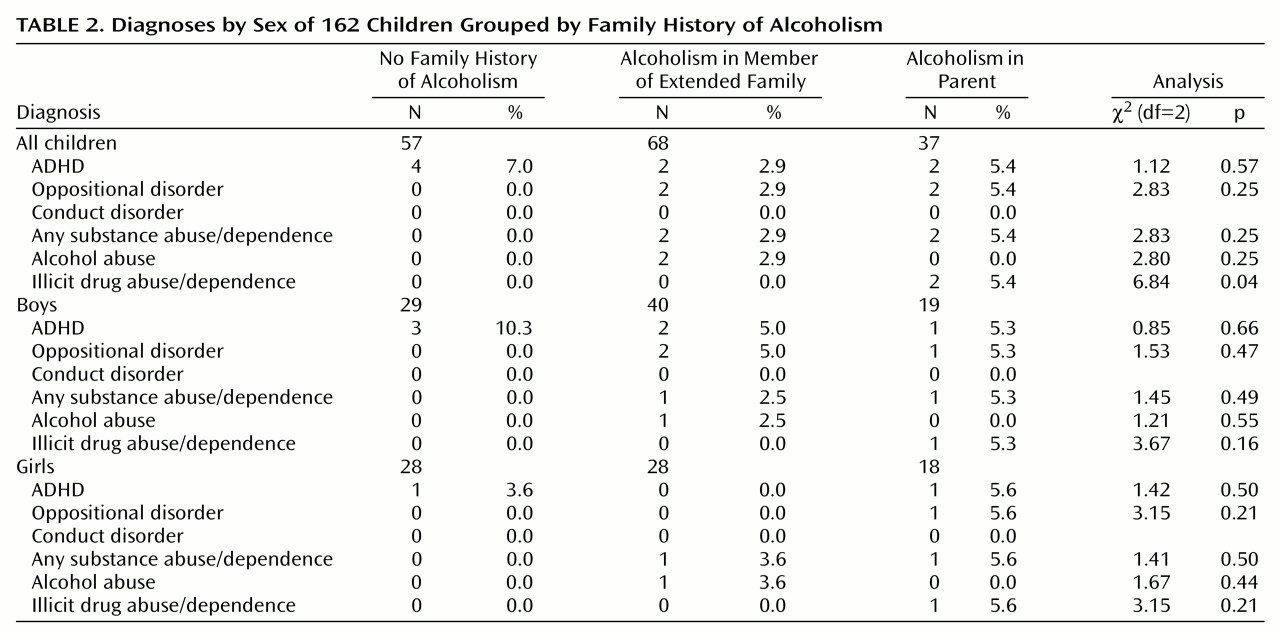
Table 1). There were no differences among the three groups in the proportion with ADHD, oppositional disorder, or conduct disorder, even when the data were analyzed separately by gender (
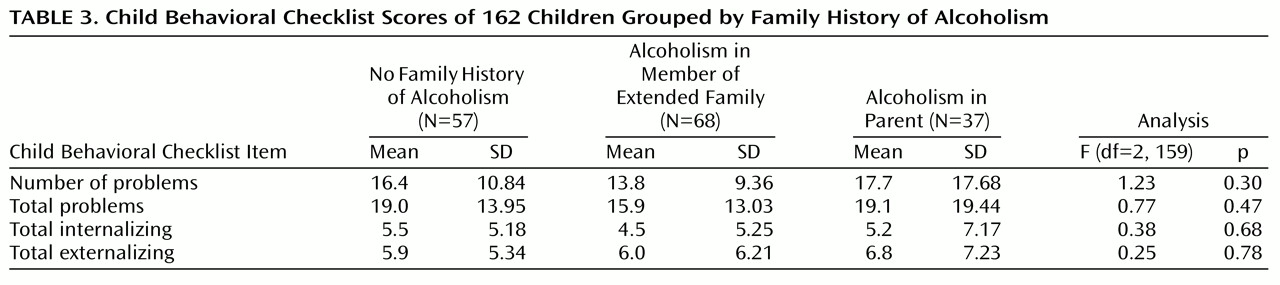
Table 2). Only illicit drug abuse or dependence differed among the groups: children with an alcoholic mother or father had higher rates of this disorder. Results were reanalyzed for subjects with no family history of alcoholism compared with groups 2 and 3 combined, and no significant differences were found according to Fisher’s exact test, with probabilities ranging from 1.00 to 0.15. There were no differences among the groups for four summary scores from the Child Behavioral Checklist (
Table 3).
Two additional steps were taken to evaluate the findings. First, the data were reanalyzed for the 87 children who were 10 years old or older. The results revealed no significant differences across groups for any diagnosis other than the already noted substance-related diagnosis, and this became nonsignificant with the Fisher’s test. Second, Child Behavioral Checklist scores were reanalyzed with the Kruskal-Wallis statistic, and no significant group differences were found (χ2=0.02–1.16, df=2, p=0.99–0.34).
Finally, the generally negative results raised a question of adequate power to detect group differences. For both ANOVA and chi-square there was sufficient power (0.80) at alpha=0.05 to detect down to at least moderate effect sizes, with only a small probability of a Type II error.
Discussion
The findings of this study, which controlled for socioeconomic status and family histories of antisocial disorders, do not indicate a higher risk for ADHD, oppositional disorder, or conduct disorder in the children of highly functional alcoholics. The only differences between children with and without alcoholic families related to possible higher risks for drug use disorders in children with a family history of alcoholism. The possible higher risk for drug but not alcohol use disorders in this group of young children with alcoholic relatives is not consistent with the findings of several large-scale studies
(16) or with our own evaluations of the original 453 subjects
(13). Perhaps the pattern of problems with substances will change as the children enter the major ages of risk for alcohol abuse and dependence.
These results are tentative for several reasons. First, although the number of children appropriate for evaluation will increase to more than 500 over the next 10 years, the size of the current study group is modest. Group differences for externalizing disorders, therefore, might appear as the study group grows. Second, the young age of the subjects allows for only tentative conclusions regarding substance use disorders. Third, data were available only through interviews with parents, although child interviews are incorporated into the ongoing 20-year follow-up. Thus, at this stage, parents might have been unaware of some substance use or psychiatric symptoms in their children. Fourth, none of the fathers of the original subjects had antisocial personality disorder, which is likely to have contributed to the low rate of conduct disorder in these children. Finally, these results might not reflect those likely to be observed if individuals from different socioeconomic strata and with different educational levels had been included.