Cigarette smoking is a great health problem in the general population
(1). It is extremely prevalent among patients with schizophrenia
(2). Smoking is associated with a lower risk of Parkinson’s disease and neuroleptic-induced parkinsonism
(3). Both the addictive effects and the controversial associations with schizophrenia and Parkinson’s disease are related to dopamine release in the central nervous system (CNS)
(1–
3).
In animal studies, nicotine, the neuroactive compound of tobacco, releases dopamine and stimulates energy metabolism in the basal ganglia, and especially in the ventral tegmental area and nucleus accumbens
(4), which have been suggested to be central in reinforcing the effect of addictive compounds
(5). In a human study, intravenously administered nicotine induced a dose-dependent increase in neuronal activity in a distributed system of brain regions, including the nucleus accumbens, amygdala, cingulate, and frontal lobes
(6).
There is, however, no direct evidence of smoking-induced or nicotine-induced increases in dopamine transmission in the human CNS. On the contrary, Geracioti et al.
(7) found that smokers had markedly lower dopamine metabolite homovanillic acid (HVA) levels than nonsmokers in the CSF but not in the plasma. Our aim was to study whether presynaptic dopamine transmission, measured by [
18F]fluorodopa ([
18F]DOPA) uptake with positron emission tomography (PET) techniques, is increased in the basal ganglia of healthy smoking men.
METHOD
The subjects were white Caucasian volunteers, 35 to 40 years old; all were healthy men working in a local shipyard. The smokers (N=9) had smoked cigarettes for at least the 15 previous years (mean=19.8 years, range=15–25) and smoked currently at least 15 cigarettes/day (mean=19.8 cigarettes/day, range=16–25). The age-matched comparison group (N=10) had never smoked regularly and had not smoked at all during the previous 5 years. There was no significant difference between smokers and nonsmokers in age (mean=37.1 years, SD=3.4, versus mean=36.8 years, SD=4.1) and body mass index (mean=24.8, SD=1.9, versus mean=24.0, SD=2.6).
All subjects underwent a physical and neuropsychological examination and psychiatric interview, including a standardized psychiatric interview (the Schedules for Clinical Assessment in Neuropsychiatry
[8]) and laboratory tests. Only subjects who had no CNS disease or trauma or DSM-IV psychiatric diagnosis and who were found to be healthy on physical examination were selected for the study.
The study protocol was approved by the Ethical Committee of Turku University/Turku University Central Hospital, Finland. After complete description of the study to the subjects, written informed consent was obtained.
Dopamine activity was measured by using [
18F]DOPA PET techniques. All subjects were allowed to have a light breakfast at about 8:00 a.m.; no food was allowed 3–4 hours before the PET scan. The smokers were allowed to smoke as usual 2 to 3 hours before the PET scan. [
18F]DOPA preparation and high performance liquid chromatography analysis of unchanged [
18F]DOPA and labeled metabolites in arterial plasma were performed as described elsewhere
(9). The PET experiments were performed by using a whole-body PET scanner (ECAT 931/08-12) and analyzed as described elsewhere
(10). The statistical analysis was done with a two-way repeated measures analysis of variance (ANOVA) and Student’s t test.
RESULTS
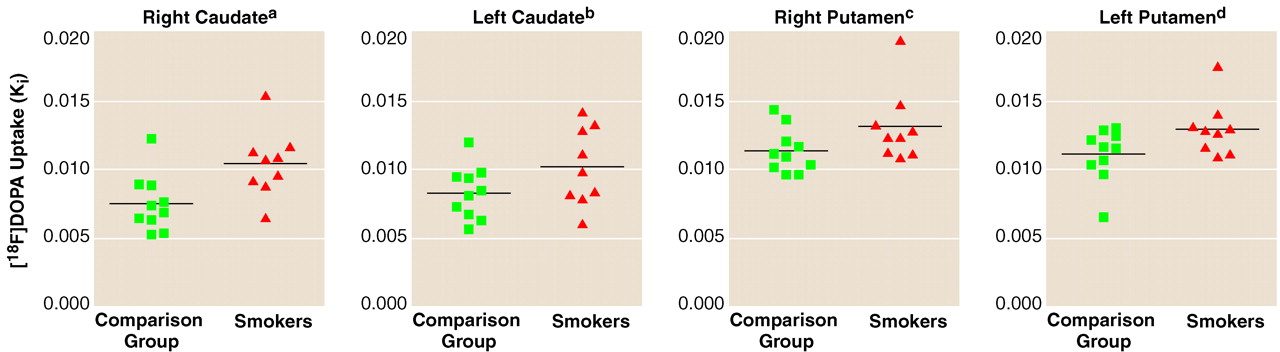
The K
i values for dopamine derived from a graphical analysis are summarized in
FIGURE 1.. The average value was 17.3% higher for smokers (mean=0.013, SD=0.002) than nonsmokers (mean=0.011, SD=0.001) in the putamen (t=2.17, df=17, p=0.04) and 30.4% higher for smokers (mean=0.010, SD=0.003) than nonsmokers (mean=0.008, SD=0.002) in the caudate (t=2.31, df=17, p=0.03). Differences between smokers and nonsmokers were also statistically significant in the left putamen (17.5%) and right caudate (38.2%) (
FIGURE 1.). Two-way ANOVA revealed no significant group-by-hemisphere interactions in the caudate (F=3.31, df=1, 17, p=0.09) or in the putamen (F=0.03, df=1, 17, p=0.87). The main effect of group was significant both in the caudate (F=5.36, df=1, 17, p=0.03) and in the putamen (F=4.65, df=1, 17, p=0.05).
DISCUSSION
Striatal dopamine activity, measured by [18F]-DOPA uptake, proved to be significantly higher in smokers than nonsmokers. To our knowledge, this is the first time it has been shown in vivo that cigarette smoking is related to increased dopaminergic activity in human basal ganglia.
As a central component of cigarette smoke, nicotine increases the release of dopamine in the smoker’s striatum and consequently can also stimulate the presynaptic dopamine synthesis in the striatum.
It has been reported that striatal monoamine oxidase A and B (MAO-A and MAO-B) levels in smokers are reduced
(11,
12). Given that dopamine is metabolized in the brain by both MAO-A and MAO-B
(13), our results on high [
18F]DOPA K
i values in smokers are in good agreement with the MAO inhibition finding. MAO is a predominantly intracellular enzyme; therefore, more dopamine may be directed to the synthesis pathway rather than to transformation to 3,4-dihydroxyphenylacetic acid. The low CSF HVA in smokers
(7) is also well explained by reduced MAO levels inhibiting both metabolic pathways (MAO-catechol
O-methyltransferase [COMT] and COMT-MAO) from dopamine to HVA. The low CSF HVA does not appear to index presynaptic dopamine function. Our measurements suggest that smoking and the development of nicotine dependence are associated with increased dopamine activity in the basal ganglia.
It is also possible that smokers form a group of people with a special neurophysiological sensitivity to presynaptic dopaminergic activation caused by nicotine. The finding that type 1 abstinent alcoholics also had high [
18F]DOPA uptake in the basal ganglia
(14) suggests that nicotine and alcohol dependence may have a similar dopamine-related mechanism.