Studies of psychotic and nonpsychotic siblings
(1–
4) and pairs of twins discordant for psychoses
(5–
9) have identified risk factors for psychoses. Among monozygotic twins discordant for schizophrenia, the twins with the illness tend to perform worse than the unaffected twins on most cognitive and personality measures
(5–
9). However, no significant differences were found on the same measures when the unaffected twins were compared with normal twin pairs (5, 9). Because these studies
(5–
9) were conducted after the affected twin had already been diagnosed with a psychotic illness, it is possible that at least some of the differences between the co-twins were not constitutional but were caused by active manifestations of the illness. Converging evidence from studies of high-risk subjects, birth cohort studies, and follow-back studies
(10–
12) indicates that subtle cognitive and behavioral abnormalities are present in healthy children and adolescents who later on manifest psychotic symptoms.
The current study used the twin study design to identify abnormalities common to both members of a pair of twins discordant for psychotic disorder that distinguish these twins from pairs of twins with no psychotic illness. To conduct the current study, we linked the Israeli National Psychiatric Hospitalization Case Registry with the Israeli Draft Board Registry for the population of male twins in Israel. This procedure enabled us to compare the premorbid cognitive and behavioral performance of all pairs of male twins in which one twin would later be hospitalized for either schizophrenia or affective psychosis. In addition, the performance of the discordant twin pairs was compared with the performance of the entire population of healthy pairs of male twins.
Method
Draft Board pre-induction assessment covers all Israeli adolescents between the ages of 16 and 17 to determine their eligibility for military service. As described in detail elsewhere
(13,
14), it consists of four cognitive tests (a modified version of Raven’s Standard Progressive Matrices; a modified, Otis-type verbal intelligence test; the Similarities—R; and the Arithmetic—R [
13,
14]) that, added together, form a valid measure of general intelligence and are transformed to an intelligence score with a mean of 100
(13). The behavioral assessment consists of a semistructured interview assessing social functioning and intimacy, individual autonomy, maturity and self-directed behavior, organizational ability and self-care, and physical activity and interest in sports
(13,
14).
The National Psychiatric Hospitalization Case Registry is a complete listing of all psychiatric hospitalizations in Israel, including the ICD-9 and ICD-10 diagnosis assigned by a board-certified psychiatrist. It was linked to the Draft Board twin file in compliance with local institutional review board approval. The merged file includes all pairs of adolescent twins (N=3,246 pairs) assessed by the Draft Board between 1985 and 1995, and all individuals reported to the National Psychiatric Hospitalization Case Registry between 1970 and 1998 given a diagnosis of schizophrenia or affective psychosis. This allowed for a follow-up of between 3 and 13 years.
The percentage of twins in the entire population of inductees was 1.1%. Since this is a registry study in which the confidentiality of the pairs with and without psychotic illness is preserved, it was not possible to establish zygosity. The merger identified 30 twin pairs with schizophrenia or affective psychosis. In 15 pairs, both twins were males, and 12 were discordant for psychosis. In seven pairs both twins were females, and all were discordant for psychosis. Because the full Draft Board test battery is administered only to males, the analyses focus on the 12 male twins who were discordant for psychosis. All of the affected twins included in the study were hospitalized at least 1 year after testing took place, a criterion that was used to help exclude prodromal illness but led also to the exclusion of two discordant male pairs. Therefore, 10 pairs of male twins were included in the analyses.
Results
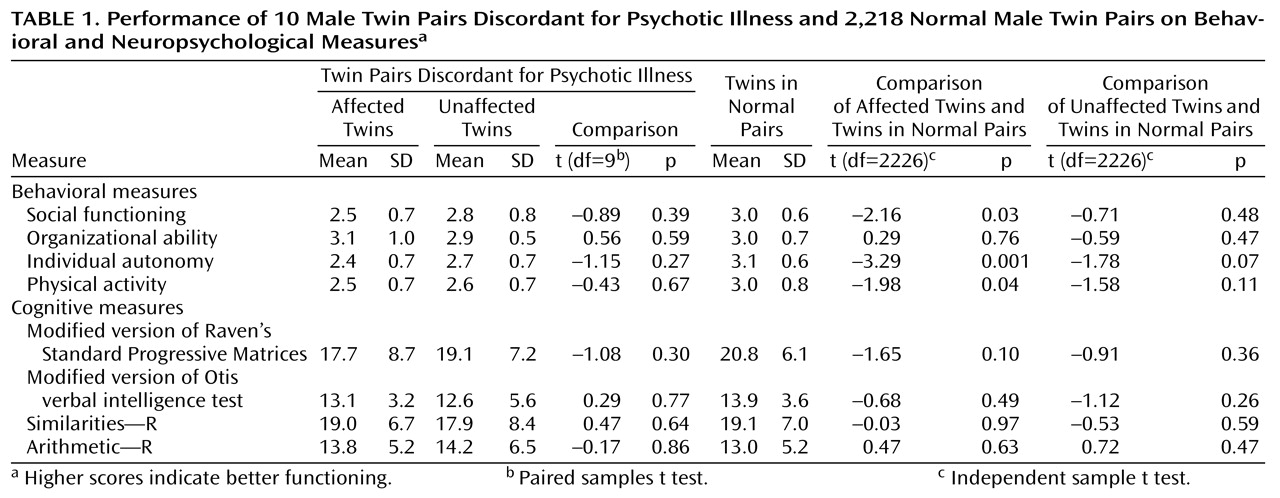
Table 1 shows that the affected twin pairs scored significantly worse than the healthy twin population on measures of individual autonomy, social functioning, and physical activity and nonsignificantly worse on the revised version of Raven’s Standard Progressive Matrices. The unaffected twins scored lower than the healthy twin population only on individual autonomy, and this difference was not significant. There were no significant differences in cognitive or behavioral scores between the affected and unaffected co-twins. However, three of the four behavioral measures as well as the revised version of Raven’s Standard Progressive Matrices followed a hierarchical pattern: the group of affected twins performed worst, the healthy twins performed best, and the unaffected twins in the discordant twin pairs fell in between. All findings were replicated by using nonparametric tests.
Discussion
We found that, as a group, apparently healthy twin adolescents who would manifest psychoses in the future performed below the level of the population of healthy twin pairs on measures of social functioning, individual autonomy, and physical activity as well as nonverbal reasoning. In addition, these four measures followed a stable hierarchical pattern: the twins with psychotic disorders performed worst, the healthy twins performed best, and the unaffected twins from the affected pair fell in between. This suggests that twins who develop psychotic disorders perform below the level of their genetic and environmental potential on several behavioral dimensions and on aspects of nonverbal intelligence.
The hierarchical pattern in the behavioral measures is consistent with results obtained in a study of behavioral and personality characteristics of monozygotic twins with schizophrenia
(9). However, unlike previous studies of cognitive measures
(5,
7), only the performance on the revised version of Raven’s Standard Progressive Matrices followed this hierarchical pattern. The discrepancy between the studies is probably because previous studies evaluated persons with already diagnosed psychoses, whereas the twins in this study were tested well before their first hospitalization (the mean time until first hospitalization for the affected twins was 4.9 years, SD=3.1). It is plausible that the overt expression of the disease causes an additional reduction in cognitive performance. These results might indicate that, although there is premorbid abnormal cognitive performance among future psychotic patients
(10–
12), the magnitude of this abnormality is relatively small at the premorbid stage of the disease. Furthermore, it might be possible that a robust decline only follows the overt expression of the psychotic symptoms.
Although this study is based on a population never reported before, it has a number of limitations. To obtain a population of same-sex discordant twins who were judged healthy at the time of testing and at least 1 year later, we had to reduce the sample to 10 pairs, which makes the conclusions vulnerable to all the limitations associated with small sample sizes, especially for comparisons within the discordant pair. Also, for reasons of confidentiality, it was impossible to establish zygosity. However, studies comparing performance in monozygotic and dizygotic twins discordant for schizophrenia with the performance of healthy twins have indicated that zygocity was not related to the differences found
(15) and that the same hierarchical pattern of results was evident in both monozygotic and dizygotic pairs
(16).
To our knowledge, this is the first study to use a national population of twins to examine premorbid cognitive and behavioral performance among individuals later hospitalized for psychotic illness, thus reducing some of the genetic and environmental biases. The results underscore the familial nature of the subtle abnormalities that precede psychotic illness.