The introduction of effective treatments for depression, including drugs and brief regimens of psychotherapy, has also drawn attention to the relatively high frequency of unfavorable outcomes
(1). This, in turn, has stimulated research interest in determining whether specific patient characteristics might predict favorable versus unfavorable outcomes
(2,
3). Reliable information of this nature would be very useful clinically.
One patient characteristic that many clinicians believe may interfere with the treatment of depression is the presence of personality pathology
(4). This idea is not a new one: both Kraepelin and Freud speculated that personality pathology was not only related to the etiology and presentation of depression but also to its responsiveness to treatment interventions
(5). The classification of depression into neurotic and endogenous subtypes relied in part on the idea that individuals with certain personality traits were more likely to develop neurotic depression and that this form of depression was less responsive to drug treatment. Paykel
(6) reported that “anxious depressives” (i.e., patients with a past history of “neurotic behavior”) had a worse response to amitriptyline than did other depressed patients. A number of early studies reported that patients with neurotic, hypochondriacal, or hysterical personality traits responded poorly to imipramine or amitriptyline—in fact, little or no better than to placebo
(7).
Over the past three decades, standardized instruments for diagnosing personality pathology have increasingly been used so that studies can now be systematically related to each other. The major diagnostic approaches are dimensional (favored by researchers and psychologists) and categorical (favored by clinicians and psychiatrists). The most important studies with dimensional measures used Eysenck’s dimension of neuroticism and Cloninger’s dimensions of harm avoidance, novelty seeking, and reward dependence.
Neuroticism is a major higher order personality dimension originally derived by factor analysis from large and diverse samples, the core of which is temperamental sensitivity to negative stimuli
(8). High neuroticism scores are associated with patients who tend to experience various negative affective states. Studies of the relationship between neuroticism and depression have largely used two personality measures: the Maudsley Personality Inventory
(9) and the Eysenck Personality Inventory
(10), which are very similar.
In the last 10–15 years, a promising new scale for measuring personality, the Tridimensional Personality Questionnaire, has been studied in relation to outcome in depression. The Tridimensional Personality Questionnaire measures three personality dimensions: novelty seeking, harm avoidance, and reward dependence. Variation in these dimensions is said to be associated with specific monoamine pathways
(11,
12). Novelty seeking is hypothesized to reflect heritable differences in the behavioral activation system. High novelty seeking scores manifest as exploratory behavior and active avoidance of monotony and impulsivity. Harm avoidance is said to reflect individual differences in the behavioral inhibition system. Individuals with high harm avoidance scores are worried, fearful, shy, and fatigable. Finally, reward dependence is hypothesized to reflect heritable individual differences in the behavioral maintenance system. Reward-dependent individuals are described as dedicated, warm, loving, and emotionally dependent.
Studies that used standardized categories of personality pathology began in 1980. The introduction of a separate axis for personality disorders in DSM-III has resulted in most studies over the past two decades using DSM axis II criteria. Personality disorders are conceptualized as the presence of enduring personality traits that are “inflexible and maladaptive and cause significant functional impairment or subjective distress” (DSM-IV, p. 630). Studies have generally reported that a very high proportion of individuals diagnosed with major depression also meet criteria for at least one axis II personality disorder. Estimates have ranged from 18% to 95%
(13), although prevalence rates usually fall between 35% and 65%
(5).
Most studies have reported that personality pathology appears to be very common in patients with depression. This suggests that there may be potentially significant treatment implications for these patients. Personality may affect overall treatment response or response to certain treatment modalities or influence what treatments patients receive. This article will systematically review studies that have used standardized instruments to measure personality pathology in depressed patients and have related these measures to treatment outcome. This will hopefully lead to some useful clinical recommendations.
Method
The databases PsycINFO and MEDLINE were searched for citations up to and including November 2000. First, the term “major depression” was used as a qualifier and combined with “personality” and “personality disorder.” A second search used the terms “depression” and “personality disorder” as qualifiers and combined them with “psychotherapeutic outcome” and “treatment outcome.” All published citations were also cross-referenced for other studies.
The initial PsycINFO searches yielded 355 citations for depression and personality, 337 citations for depression and personality disorder, 190 citations for personality disorder and treatment outcome, and 671 citations for depression and treatment outcome. The initial MEDLINE searches yielded 656 citations for depression and personality, 116 citations for depression and personality disorder, 255 citations for personality disorder and treatment outcome, and 733 citations for depression and treatment outcome.
I looked for empirical articles that involved depressed patients who received some type of standardized personality assessment and included some measure of treatment outcome. Inclusion criteria were broad and allowed for 1) a reasonable definition of depression for the patient group, 2) a systematic assessment of personality pathology, 3) depression outcome measures that were related to the personality pathology, and 4) a clear report on the treatment(s) received and whether treatment was controlled or uncontrolled (i.e., whether all patients either received the same treatment or were placed in different treatment groups by random assignment). The studies were grouped according to the model used to assess personality pathology. A meta-analysis was attempted for the small subgroup of studies that incorporated DSM structured interviews and in which treatment was controlled.
Results
Aspects of Dimensional Measures
Neuroticism
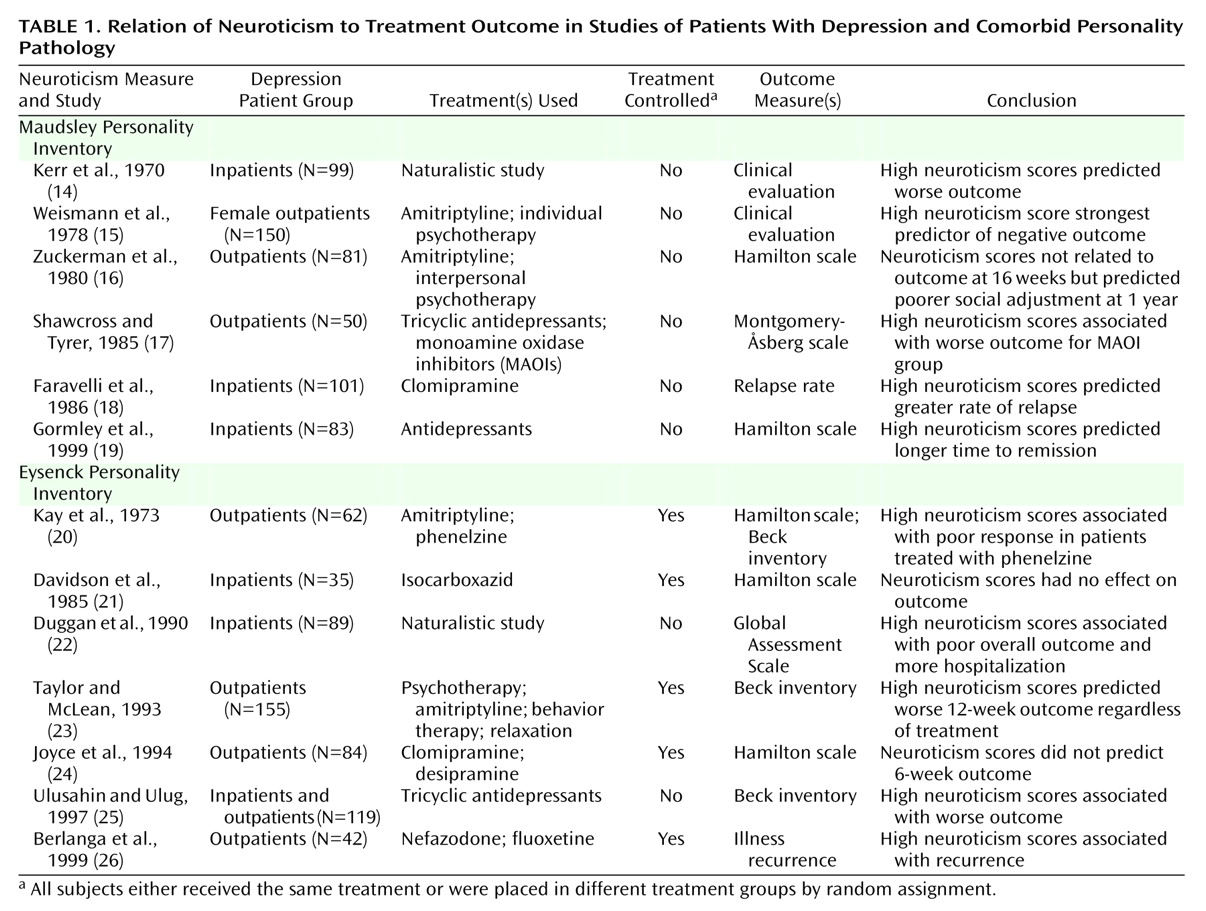
From
Table 1, it can be seen that in most studies high neuroticism scores predicted worse treatment response in depressed inpatients and outpatients. There are two important points to note. First, most of the studies looked at long-term outcomes. The four that considered short-term response were more equivocal. Zuckerman et al.
(16) reported that neuroticism scores did not predict 16-week outcome, only 1-year outcome. Davidson et al.
(21) and Joyce et al.
(24) found no relationship to 6-week outcome, while Kay et al.
(20) reported that neuroticism predicted poor response to phenelzine but not amitriptyline. Only Taylor and McLean
(23) reported that high neuroticism scores predicted worse outcome at 12 weeks. Second, only five of the studies randomly assigned patients to treatment; the rest were naturalistic studies.
Harm avoidance, novelty seeking, and reward dependence
The first study that considered the relationship of Tridimensional Personality Questionnaire measures to outcome was by Strakowski et al.
(27). They reported that high novelty seeking scores in manic patients at discharge predicted poorer functional recovery. Since then a number of studies of depressed patients have been undertaken (
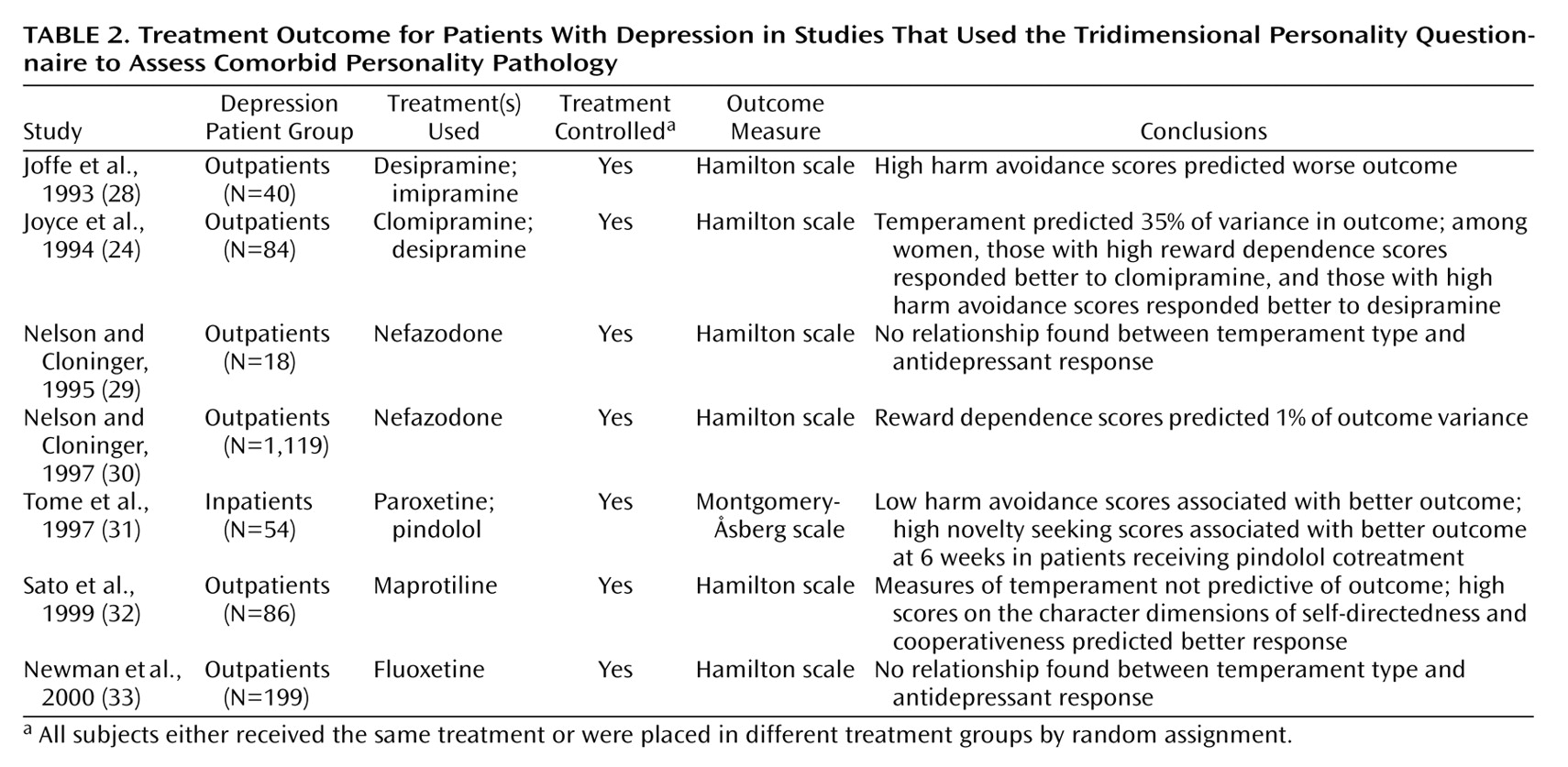
Table 2). Joffe et al.
(28) reported that high harm avoidance scores predicted worse outcome in 40 depressed outpatients. The study by Joyce et al.
(24) found that temperament accounted for 35% of the variance in outcome in depressed outpatients. In addition, women with high harm avoidance scores responded preferentially to desipramine, while those with high reward dependence scores responded preferentially to clomipramine. At the time, these results suggested that personality might prove clinically useful in helping to decide which drug to give to which patient.
In a small study that partly replicated these results, Nelson and Cloninger
(29) initially reported that reward dependence accounted for 37% of the variance in percentage change in depressive symptoms. However, they discovered that they had wrongly analyzed their study data and that, in fact, Tridimensional Personality Questionnaire measures were not significantly related to outcome. Since then, results have been much less compelling: in a much larger study
(30), Nelson and Cloninger reported that lower reward dependence scores predicted better response to nefazodone, but this result only explained 1% of the variance in outcome measures and was in the opposite direction from the Joyce et al.
(24) study. One study reported that low harm avoidance and high reward dependence scores predicted better outcome in an open paroxetine trial
(31), but another found that Tridimensional Personality Questionnaire scores were unrelated to response
(32). A recent attempt to replicate the Joyce et al.
(24) study failed to find any relationship between Tridimensional Personality Questionnaire scores and depression outcome
(33).
The studies that used the Tridimensional Personality Questionnaire had generally reasonable methods. They were prospective, and all patients either received the same treatment or were randomly assigned to different treatments. The outcome measure most commonly used was the Hamilton Depression Rating Scale.
Aspects of Categorical Measures
Method of diagnosis
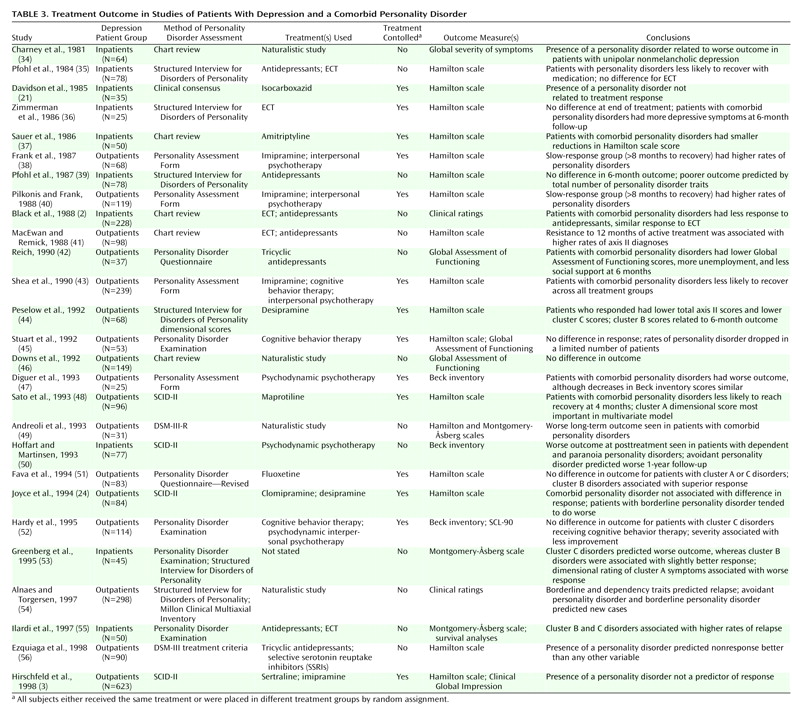
Twenty-seven studies that used or claimed to use DSM axis II criteria are presented in
Table 3. Overall, 15 studies reported a worse outcome, five reported a partially worse outcome, and seven reported no difference in treatment outcome. There were a wide variety of assessments of personality disorders, treatments offered, and outcome measures used, so simply grouping the studies together was not feasible.
The studies that used dimensional measures of personality pathology may have used different treatments for varying time periods, but they at least had the same measure of personality. In contrast, the ways of assessing DSM personality disorders ranged from chart review to questionnaires and structured interviews. How personality disorders are measured significantly affects the rate and type of personality disorders
(57). For example, Hunt and Andrews
(58) reported that outpatients with anxiety disorders had nine times the chance of having a personality disorder when diagnosed according to the Personality Disorder Questionnaire rather than the Personality Disorder Examination interview. Reich and Noyes
(59) reported similar disparities between the Structured Interview for Disorders of Personality and the Millon Clinical Multiaxial Inventory and Personality Disorder Questionnaire. Zimmerman and Mattia
(60) reported that the rate of borderline personality disorder was significantly higher when using a structured interview than in a clinical evaluation (14% versus 0.4%). These differences are far from trivial and clearly imply that subjects diagnosed as having a personality disorder in one study may be very different from those in another study if an alternative instrument is used.
Structured interviews
Deciding what measures of personality disorder are most valid is a difficult task. Intuitively, interviews appear to be more valid than self-administered questionnaires. Interviews allow questions to be clarified, allow an attempt to disentangle state and trait characteristics, and allow elements of mental state and presentation to be used as data
(57). They have good to very good interrater reliability. Although they generally report higher rates of personality disorders than do clinical evaluations, Zimmerman and Mattia
(60) showed that when clinicians are given the information from the semistructured interview, they are prompted to diagnose personality disorders much more frequently so that their rate is closer to that obtained by using the semistructured interviews. It seems reasonable to say at this point that using standardized structured interviews is probably the best way to proceed.
There are three structured interviews that have been used outside of the groups that invented them: the Structured Interview for Disorders of Personality, the Structured Clinical Interview for DSM Axis II Disorders (SCID-II), and the Personality Disorder Examination. Thirteen of the studies in
Table 3 used one of these instruments (one
[53] used two): four used the SCID-II, six used the Structured Interview for Disorders of Personality, and four used the Personality Disorder Examination, although one of the latter
(52) only assessed cluster C disorders. Of these 13 studies, six reported that the presence of a personality disorder in depressed patients predicted worse outcome
(39,
44,
48,
50,
54,
55). Three reported somewhat worse outcome. Specifically, Pfohl et al.
(35) showed that outcome was worse for drugs but not ECT. Hardy et al.
(52) reported worse outcome for interpersonal psychotherapy but not for cognitive behavior therapy, and Greenberg et al.
(53) noted that patients with comorbid cluster C personality disorders had worse outcome but patients with cluster B tended to have better outcome. The other four studies
(3,
24,
36,
45) reported no difference in outcome.
Treatment control
Another significant methodological problem is controlling for treatment. Not all studies ensured that subjects received the same treatment or ensured random assignment of subjects to different treatment groups. Not controlling for treatment almost certainly introduces bias, since there is strong evidence that depressed subjects with a personality disorder are offered different treatments on the basis of their comorbid personality disorder. For example, Charney et al.
(34) found that depressed patients with a personality disorder were much less likely to receive ECT or medication, while Black et al.
(2) reported that only 29% of patients with a personality disorder received an adequate course of drug therapy compared with 49% of patients without a personality disorder. Therefore, although uncontrolled studies generally support the notion that axis II pathology predicts poorer outcome, the methodological weaknesses of such studies limit the value of their results
(5).
Of the 13 studies that used structured interviews, seven controlled for a standard treatment or randomly assigned subjects to treatment
(3,
24,
36,
44,
45,
48,
52). These seven included all four studies
(3,
24,
36,
45) that showed no difference, one that showed a mixed outcome
(52), and two
(44,
48) that showed worse outcome. Therefore, if the best-designed studies are considered to be those that used structured interviews to diagnose personality disorders and those in which treatment was controlled, then the evidence suggests that depressed subjects with personality disorders fare little if any worse than those without personality disorders, at least in the short term. A meta-analysis of these seven studies was attempted but proved impossible. The inclusion criteria, including the definition of depression, varied markedly. The type of treatment, the duration of treatment, the outcome measures, and the time of assessment of recovery were also very different. No meaningful statistical inferences could be made.
Other Methods of Personality Assessment
One research group used its own personality measures, the clinician-rated Personality Assessment Form. It requires 6-point dimensional ratings for the 11 DSM-III personality disorder categories. This was used in the landmark NIMH Collaborative Program on the Psychobiology of Depression. There are three reports from the study; two
(38,
40) reported that the so-called slow-response group had a higher rate of personality disorders than did “normal responders.” Shea et al.
(43) later reported that subjects with comorbid personality disorder were less likely to recover across all treatment groups. All three appear to report on subjects from the same study at different stages of investigation. Diguer et al.
(47) used the Personality Assessment Form in an unrelated study of 25 subjects. They reported a worse outcome for those with personality disorders but also noted that these subjects were more depressed at intake (i.e., had higher Beck Depression Inventory scores) and that the drop in symptom scores was the same.
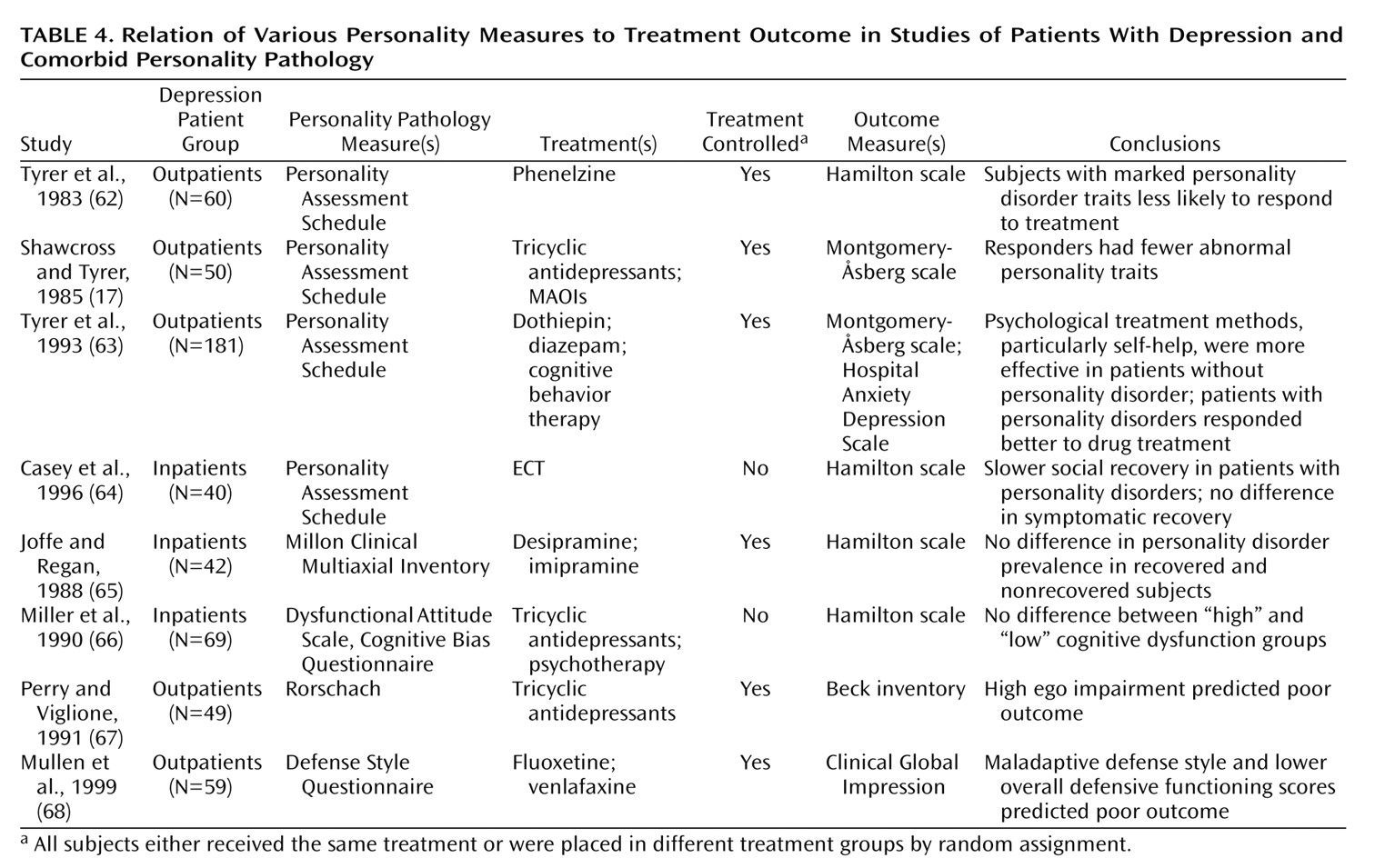
There are a number of studies by Tyrer and his group that used their instrument, the Personality Assessment Schedule
(61) (
Table 4). This is a standardized interview in which the interviewee is asked for information related to 24 personality characteristics. Ratings are made for traits and level of impairment. Studies using this instrument have reported mixed results. Early studies by Tyrer et al.
(62) and Shawcross and Tyrer
(17) showed that subjects with significant personality pathology were less likely to respond to medications. In a more recent study by Tyrer et al.
(63), those with personality disorders had more severe psychopathology than those with no personality disorder. However, presence of a personality disorder did not predict outcome, except that subjects with personality pathology tended to respond better to drug treatment than to psychological treatments. In a naturalistic study of ECT response, Casey et al.
(64) reported that although the presence of a personality disorder affected short-term outcome, it did not affect the outcome at 12 months.
Finally, four studies used unique instruments (
Table 4). Joffe and Regan
(65) used the Millon Clinical Multiaxial Inventory and reported no difference in personality disorder diagnoses in recovered versus nonrecovered subjects. Miller et al.
(66) rated subjects as having high or low cognitive dysfunction according to the Dysfunctional Attitude Scale and Cognitive Bias Questionnaire; they found this had no relationship to outcome. However, subjects with high scores on the Cognitive Bias Questionnaire scale responded better to combined treatment with a tricyclic medication and cognitive behavior therapy than to treatment with medication alone. Perry and Viglione
(67) used the Rorschach and reported that high ego impairment predicted poor outcome. Mullen et al.
(68) used the Defense Style Questionnaire and found that poor outcome was predicted by a maladaptive defense style and lower overall defensive functioning.
Discussion
Issues of measurement remain the major problem when considering the relationship of personality pathology to outcome in patients with major depression. There are four major problems: 1) the validity of the personality pathology measures themselves, 2) their relationship to mood, 3) the characteristics of depressed patients with personality disorders versus those without personality disorders, and 4) the nonuniformity of the effect of personality pathology on treatment response.
Validity of Personality Pathology
What measures of personality pathology are actually measuring is a subject of considerable debate. Studies that use self-report inventories may be reasonably reliable but are based on the unproven notion that if you want to know why a person acts in a particular way, you need only to ask, and the person will tell you
(69). This is unlikely to be true. Item endorsements, therefore, are self-presentations, not self-reports. Kagan
(70), for example, showed that when adults fill out a self-report, 40% state that they are shy, but less than half that percentage usually are when assessed with a more comprehensive battery of behavioral assessments. Such self-presentations may be even more distorted when subjects are depressed. In addition, all self-reports are by nature restrictive. A host of other stable and possibly significant human qualities may be missing. Whether the Eysenck Personality Inventory and Tridimensional Personality Questionnaire self-reports measure the most useful and valid behavioral traits in a depressed clinical population remains unknown.
Much attention has been given to the use of reliable personality disorder categories, but relatively little thought has been devoted to the fundamental question underlying the whole concept of personality disorders
(71). While the use of structured interviews is generally acknowledged as the best way of assessing axis II personality disorders
(72), the validity of the diagnoses themselves remains open to question. Ideally, the validity of instruments diagnosing personality disorders should be examined through the predicted correlates of the personality disorder construct. Unfortunately, it has not yet been demonstrated that the proposed operational criteria in DSM are themselves valid
(57,
73). Researchers are thus faced with the difficult task of validating diagnoses as well as instruments.
The current categories are based on committee consensus, historical precedent, and political argument and opinion. The individual criteria are poorly defined, and many are highly reliant on the clinician’s judgment
(71). The overlap among the personality disorders is too great. Most studies suggest that mixed personality disorders are the rule rather than the exception
(74–
76). The distribution of personality disorder symptoms in depressed patient groups gives no support to the concept that there are distinct and separate personality disorder categories. The distribution of symptoms is dimensional and continuous, with no evidence of a point of rarity in the distribution of the symptoms and signs of personality disorders in any category
(77). Empirical data with respect to bimodality, admixture analysis, and predictive validity have been most consistent with a dimensional model
(78). Therefore, we have a classification system at odds with the limited data available. The inconsistent and unexpected findings may be due to the diagnostic system rather than measurement or sampling error.
At the very least, researchers should be wary of these validity problems in their analyses. To analyze a single personality disorder as an independent category, without making allowances for comorbidity and subclinical cases, is difficult to justify. It may be preferable to use dimensional scores as predictors rather than categorical personality disorders and to use multivariable analytic techniques. There is evidence that this can lead to different results. In the Sato et al.
(48) study, for example, simple comparisons that used t tests or chi-square tests suggested that patients with any personality disorder had a significantly worse outcome. Using a log-linear model to assess the independent effect of personality disorders on outcome showed that only the presence of cluster A personality disorders worsened outcome; the presence of cluster B or C personality disorders did not have an effect. Greenberg et al.
(53) reported that a positive categorical diagnosis of cluster C (but not dimensional) and a positive dimensional diagnosis of cluster A (but not categorical) disorders predicted poorer outcome. They suggested that this was because cluster A diagnoses were rare in their study group and that the statistical tests for dimensional and categorical models are not conceptually similar.
Classification problems mean that it remains unclear whether personality disorder categories are a general measure of personality pathology affecting outcome or whether individual categories, or clusters, predict different outcomes. Most studies that have looked at this problem report that the presence of two or more personality disorders predicts worse outcome than one
(35), but most of the studies involve patient numbers too small to study the effects of personality disorder clusters, let alone individual personality disorders. The largest study, with 623 patients, reported no difference in response for any of the DSM-III-R personality disorder categories except that the presence of comorbid passive-aggressive personality disorder predicted slightly better outcome
(3).
Relationship of Personality to Mood
The reports on the relationship of neuroticism and Tridimensional Personality Questionnaire measures to mood are reasonably consistent. Nearly all studies that have looked at this relationship have reported that neuroticism scores are strongly correlated with depression severity. Neuroticism scores were higher in depressed patients than in a group of randomly selected students
(79). Scores were higher still in more severely depressed patients
(16,
80) but tend to normalize with treatment
(13,
17). Studies that use the Hamilton depression scale as an outcome measure have a particular problem: 19 of the 24 neuroticism items appear in the Hamilton depression scale
(81). Like neuroticism, harm avoidance scores appear to be related to depression severity
(82) and decrease with successful treatment in all the studies that have reported on this
(26,
82,
83). The other Tridimensional Personality Questionnaire dimensions, novelty seeking and reward dependence, appear to be relatively unaffected.
The obvious question therefore is whether neuroticism and harm avoidance scores reflect personality characteristics that may affect recovery or whether they are subclinical depression symptoms that are related to poorer recovery and a higher chance of relapse.
The relationship of personality disorder categories to mood is less consistent. While most authors argue that mood affects the assessment of personality disorders
(63,
84), some report that it does not. What limited evidence there is suggests that clinical interviews, in which clinicians are encouraged to exercise their clinical judgment to allow for the potential distortion produced by the dysphoric mental state, may be less prone to trait-state artifacts than personality inventories and questionnaires
(85). However, using structured interviews is no guarantee of unbiased independent assessment of personality disorders.
One way around this problem is to take a pragmatic approach. If measures of personality consistently predict something about outcome or choice of treatment, then they are useful. Whether they are actually measuring personality, chronic depression symptoms, or current mood is of more interest to a researcher than a clinician. A clinician is interested in making predictions and plans, which usually means studying patients during an acute illness. If measures of personality, whether distorted by the illness or not, aid treatment planning, then they are useful.
Differing Depression Characteristics
Another probable source of bias is the characteristics of depressed patients with personality disorders versus those without. The personality disorder symptoms may be correlated with other features of depression which themselves are related to treatment outcome. The only ones studied systematically are depression severity and age at onset. Several studies have reported that depressed subjects with comorbid personality disorders were significantly more severely depressed at treatment onset than subjects without a personality disorder
(35,
42), whereas others have detected no difference
(24,
34,
36,
48). There is some evidence that depression severity affects response to treatment, although this probably depends largely on the outcome measures that are chosen
(86). Whatever the case, it seems prudent to control statistically for the potential confounding effect of pretreatment depression severity upon treatment outcome. This was rarely done in any of the studies reviewed.
A study by Fava et al.
(87) reported that patients with early-onset major depression had higher rates of personality disorder than did those with later-onset depression, but Skodol et al.
(13) failed to replicate this. They reported however that early-onset dysthymic disorder was associated with a higher rate of personality disorders. This is consistent with most studies that have reported higher rates of personality disorder in patients with dysthymia
(88). Given the difficulties distinguishing dysthymia and recurrent major depression, particularly retrospectively, it seems reasonable to suggest that mood disorders with recurrence and the presence of at least some mood symptoms much of the time are more likely to be diagnosed with a comorbid personality disorder. This implies that measures of age at onset and chronicity should be systematically obtained and statistically controlled for when considering the effect of personality disorder on outcome. There is no evidence from many of the studies reviewed that this was done.
Differential Effects on Treatment Outcome
One of the most important clinical questions is whether there is evidence that depressed patients with personality pathology respond differently to treatment. There have been hints of this, but no consistent results have emerged. Two controlled studies reported that high neuroticism scores predicted worse outcome for patients treated with MAOIs but not tricyclic antidepressants
(17,
20). Fava et al.
(51) reported that the presence of a cluster B personality disorder predicted positive outcome to fluoxetine, as measured by the change in Hamilton depression scale scores. This is consistent with a number of small open studies that have reported that borderline personality disorder symptoms respond to SSRIs but poorly to tricyclic antidepressants
(89–
91).
Peselow et al.
(92) reported that individuals with high autonomous traits (i.e., those who attempt to maximize control over their environment) and low sociotropic traits (i.e., those who are very concerned with rejection from others) showed greater response to antidepressants than did those who had high sociotropic and low autonomous traits. Joyce et al.
(24) reported that women with high reward dependence (similar to high sociotropy) responded better to clomipramine than to desipramine. These results were interesting and suggested that personality might enable better matching of patients to specific treatments for depression. Unfortunately, neither study has so far been replicated.
There is reasonable evidence that ECT seems to be as effective in depressed patients with personality disorders and in those without. The four studies that have looked at this have reported no significant difference
(35,
41,
67,
93). These studies also found that in those subjects treated with antidepressants, personality pathology predicted worse outcome. However, as Ilardi and Craighead
(5) reported, these studies had small numbers of subjects receiving ECT, and all showed a tendency toward worse outcome, although it was not statistically significant. In addition, none of the studies was controlled, so it is possible that patients considered suitable for ECT may have been substantially different in terms of their personality pathology from those receiving alternative treatments.
There are conflicting results on the use of psychotherapy in patients with personality pathology. Shea et al.
(43) claimed that although there were no statistically significant interactions between treatment condition and personality disorder in the NIMH Treatment of Depression Collaborative Research Program, there was a pattern of worse outcome for personality disorder patients in all treatment conditions except for cognitive therapy (i.e., in patients who received interpersonal psychotherapy, imipramine, and pill placebo). Stuart et al.
(45) also reported that comorbid personality disorders did not affect outcome in patients treated with cognitive therapy, and a study by Hardy et al.
(52), which only studied cluster C personality disorders, showed that cluster C personality pathology worsened outcome in those receiving interpersonal therapy but not in those receiving cognitive therapy. There is also an unpublished study cited by Shea et al.
(94) that found that personality disorder comorbidity did not affect treatment outcome in patients receiving cognitive therapy. On the other hand, Tyrer et al.
(63) reported that patients with comorbid personality pathology fared better with drugs than with psychotherapy, although cognitive therapy was superior to self-help in their study. The two studies that used psychodynamic psychotherapy reported worse outcome for depressed patients with personality disorders
(47,
50). The limited evidence appears to favor structured psychotherapeutic interventions such as cognitive behavior therapy over less structured ones, but well-conducted randomized studies are obviously needed.
Summary and Conclusions
Personality pathology does not improve outcome in patients receiving treatment for major depression. This uninspired statement is probably the most accurate one that can be made at this point. Whether it worsens outcome depends on what is meant by personality, who is being treated, how the treatment is conducted, and how outcome is defined.
High neuroticism scores appear predictive of poor prognosis. This is particularly true when longer-term outcome is considered. There are three significant limitations to these reasonably consistent findings. First, neuroticism is strongly related to depression. Second, many of the neuroticism score items also appear in the Hamilton depression scale, which is by far the most common outcome measure used in studies. Third, neuroticism is a broad construct that appears to convey vulnerability in a nonspecific way for a range of “distress disorders.” Such a broad construct is not particularly useful for clinicians as an aid to treatment planning
(8).
Cloninger’s Tridimensional Personality Questionnaire dimensions do not, on present evidence, appear to have a consistent relationship to treatment outcome in depressed patients. There is some suggestion that high harm avoidance (which is state dependent and strongly related to neuroticism) predicts poorer outcome, but this has not been consistent. The finding that harm avoidance and reward dependence were related to differential treatment response has not been replicated. Only one study
(32) has used the expanded seven dimensions of temperament and character to predict response; the authors reported that the character measures of self-directedness and cooperativeness, but not temperament measures, predicted better response. Whether such measures will aid clinical management remains to be seen.
Personality disorders, largely measured according to the DSM system, have inconsistent effects on outcome in depressed patients. Certain treatments (particularly ECT as well as properly conducted trials of antidepressants and possibly cognitive behavior therapy) appear to be equally effective regardless of the presence of comorbid personality disorders. The best-designed studies, which used structured clinical interviews and in which treatment was controlled, found the least evidence that personality disorders adversely affect treatment outcome. Those that did not control treatment reported that depressed patients with personality disorders appear less likely to receive antidepressants and ECT, which may partially explain their worse outcome. The last comprehensive review (which only looked at somatic treatments) by Ilardi and Craighead
(5) 6 years ago, while noting the methodological problems, concluded that “Axis II comorbidity predicts negative outcomes, both acute and long-term, with pharmacological treatments for depression” (p. 214). The evidence, particularly regarding acute outcome, is now much less conclusive. This is particularly so since trials that produce findings at odds with the null hypothesis are more likely to be published.
The interminable questions of what constitutes depression and what constitutes personality remain unresolved. All the so-called personality measures may be partially picking up aspects of depression not detected in current symptom measures or clinical constructs. These include depression severity, chronicity, atypical features, or additional important symptoms such as irritability, impulsivity, paranoia, and anger, which are outside our current diagnostic systems. It is also possible that the measures reviewed may not be the most appropriate ones to predict prognosis and guide treatment.
This review has emphasized methodological problems and now offers several specific recommendations to try and reduce errors in future investigations. First, the use of a structured interview for assessing personality disorders seems the only reasonable recommendation at present
(5,
57). Criteria obtained should be included in statistical models as dimensional scores as well as categories. The effects of overlap in personality disorder diagnoses need to be carefully considered. Using an additional personality questionnaire as a paper standard to compare with interviewer diagnoses is also advisable. Second, differences between patients with and without a personality disorder need to be sought; these should include severity, chronicity, and age at onset as well as age and sex. If significant differences are found, they need to be statistically controlled. Third, ensure that subjects receive the same treatment or are randomly assigned to treatment for roughly the same amount of time. Personality pathology is clearly a variable clinicians consider when selecting treatments for their patients, so naturalistic studies will almost certainly be biased. Fourth, ensure that the samples are as representative as possible (i.e., do not exclude certain personality disorders or individuals with a history of alcohol and drug use) and large enough to detect at least moderate-sized effects of personality pathology upon treatment response. Fifth, use a continuous rather than dichotomous measure of posttreatment depression. Measures other than Hamilton depression scale should be considered, particularly if neuroticism is one of the personality measures used as a predictor. Sixth, include evaluation of social support and interpersonal difficulties, since they themselves may relate to poor treatment outcome
(95). Seventh, multivariable analytic techniques incorporating all the variables of interest need to be included simultaneously in a predictive outcome model to try and distinguish the unique properties of personality pathology (if there are any) that are responsible for treatment outcome.
In conclusion, the strongest support for the idea that personality pathology predicts poorer outcome when treating depressed patients comes from the methodologically weakest studies or when the construct studied (such as neuroticism) overlaps significantly with depressive symptoms. More recent and more carefully designed studies tend to report little or no difference in short-term outcome. The studies reviewed here were heterogeneous, took place within a wide variety of settings, and covered a range of psychopathology. It is little wonder that general recommendations are presently impossible. There is also no doubt that more guidance is needed on how to choose treatments for patients. Measures of personality that predict outcome will continue to be sought no matter whether they in fact measure personality. In particular, personality variables that help predict differential response to treatments may be clinically useful. It is to be hoped that studies will be more carefully designed to try to adjust for some of the confounding variables that are inevitable when measuring such a complex construct.
Finally, from a clinician’s point of view, there is good news. The presence of a comorbid personality disorder does not appear to worsen outcome for patients with major depression, provided that the patients receive good standard treatment for their mood disorder. Their outcome is probably as good as in patients with no measurable personality pathology unless, as often seems to happen, they receive less than adequate trials of medication, psychotherapy, or ECT.