Sample Characteristics
The five cohorts of patients from 1975, 1980, 1985, 1990, and 1995 included a total of 2,861 subjects (1,689 male patients and 1,172 female patients). The mean age at first admission was 28.1 years (SD=13.9), and the most common ages at first admission were between age 20 and 25 years. The matched comparison group included 2,861 subjects and was identical to the patient group in gender and age distribution. The number of patients in the 1995 cohort was artificially elevated by a delay in recording data for patients who were actually first seen in 1994. Separating the two groups was problematic, so all were included in the study.
Convictions
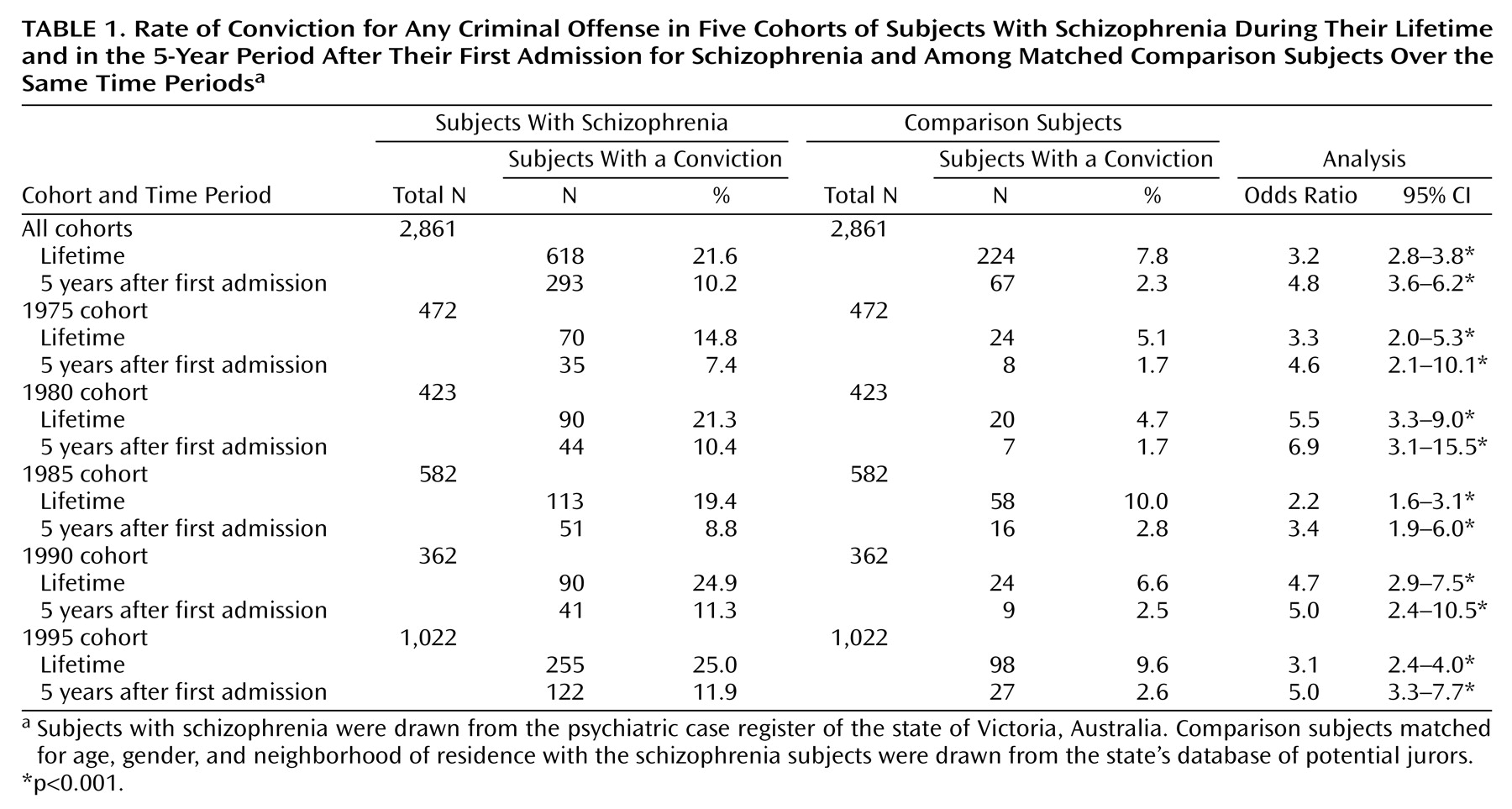
The patients with schizophrenia were significantly more likely to have been convicted of at least one offense than the community comparison subjects, both during their lifetime to date (21.6% versus 7.8%) and in the 5-year period after their first admission (10.2% versus 2.3%) (
Table 1). When the cohorts were examined individually, all five were found to be more likely than the comparison subjects to have had a conviction over their lifetime and in the 5 years after their first admission (
Table 1). Male patients with schizophrenia in the combined cohorts had significantly higher rates of conviction than the male comparison subjects over their lifetime (31.3% versus 11.7%) (odds ratio=3.4, 95% CI=2.9–4.1, p<0.001) and in the 5 years after their first admission (15.0% versus 3.5%) (odds ratio=4.9, 95% CI=3.7–6.6, p<0.001). The differences remained significant when the cohorts of male patients were each considered separately. For female patients, the rate of offending was significantly higher, relative to the female comparison subjects, in the combined cohorts for lifetime offending (7.7% versus 2.2%) (odds ratio=3.7, 95% CI=2.4–5.7, p<0.001) and in the 5 years after the first admission (3.3% versus 0.7%) (odds ratio=5.0, 95% CI=2.3–10.8, p<0.001), but the results for individual cohorts of female patients were not significantly different from those for the female comparison subjects.
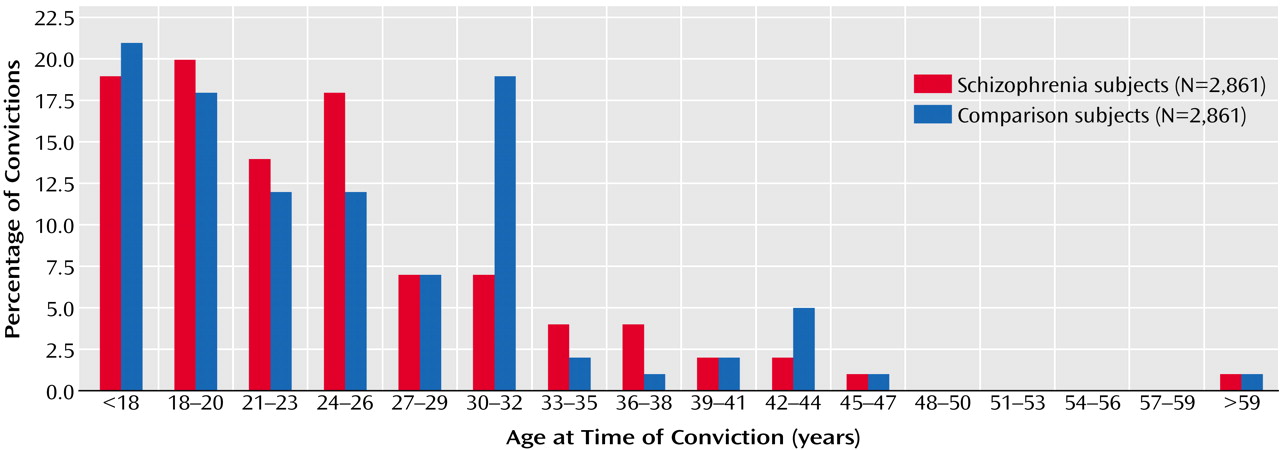
The total number of convictions among the subjects with schizophrenia was also higher than that among the comparison subjects (8,791 versus 1,119); both male and female patients with schizophrenia had a higher total number of convictions than their matched comparison subjects (male subjects: 8,115 versus 1,045; female subjects: 676 versus 74). The mean number of convictions for each offender was significantly higher in the schizophrenia cohorts than among the comparison subjects (14.2 versus 5.0; p<0.001, t test); the male patients with schizophrenia had a higher mean number of convictions than the male comparison subjects (15.4 versus 5.3; p<0.001, t test), but there was no difference between the female patients and the female comparison subjects (mean=5.1 versus mean=2.9; n.s., t test).
The rate of criminal conviction over the lifetime to date among patients with schizophrenia gradually increased from 14.8% in the 1975 cohort to 25.0% in the 1995 cohort (
Table 1). This increase occurred even though the number of years at risk for offending was greater in the earlier cohorts than in the later cohorts, because the earlier cohorts had an older average age. The patients’ rate of offending during the 5-year period after the first admission increased over the years, from 7.4% in the 1975 cohort to 11.9% in the 1995 cohort (
Table 1). The rates of overall offending also increased over the years of the study in the comparison group. Among comparison subjects, the lifetime-to-date rate of offending rose from 5.1% in the group matched to the 1975 patient cohort to 9.6% in the group matched to the 1995 cohort (
Table 1). Similarly, the comparison subjects showed an increase in offending in the 5 years after their matched subjects’ first admission, from 1.7% in the group matched to the 1975 cohort to 2.6% in the group matched to the 1995 cohort (
Table 1). When we calculated the odds ratios for offending among subjects with schizophrenia relative to their matched comparison subjects, no consistent pattern suggestive of either a relative increase or a decrease over time in the schizophrenia group was apparent (
Table 1). This finding suggests a similar increase in the rate of convictions over the period of the study among both the patients with schizophrenia and the comparison subjects.
Violent offenses
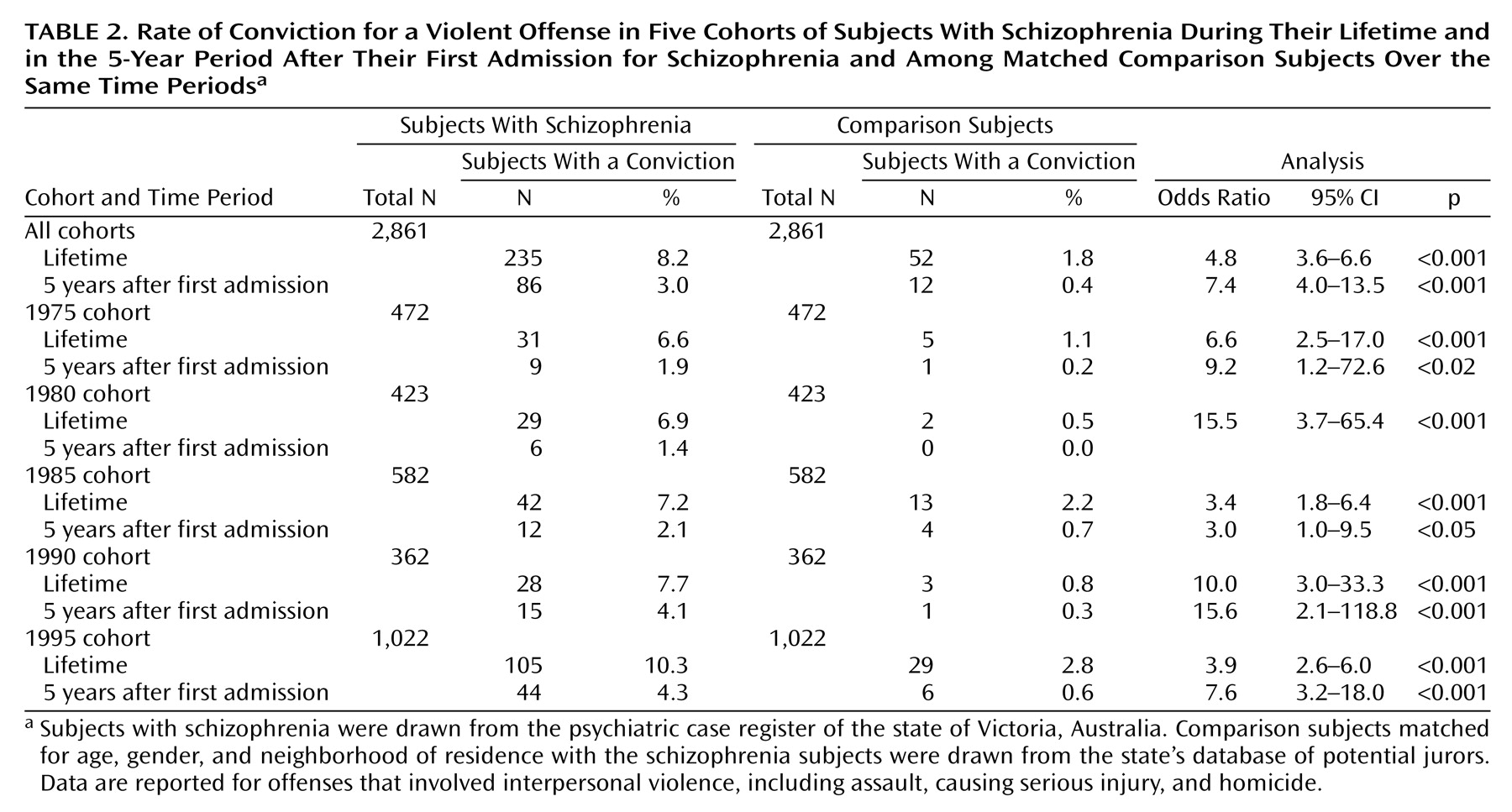
The overall frequency of violent offenses was significantly higher among the patients with schizophrenia than among the comparison subjects (8.2% versus 1.8%) (
Table 2). The rate of violent offending among the patients with schizophrenia gradually increased over the years of the study from a lifetime conviction rate of 6.6% in 1975 to 10.3% in 1995 (
Table 2). This increase coincided with a proportionately similar increase in the conviction rate in the comparison group, from 1.1% to 2.8%. There was no difference in the rate of increase in violent offending between the schizophrenia patients and the comparison subjects over the period of the study. The 235 patients with schizophrenia who had convictions for violent offenses over their lifetime to date had 855 separate convictions for such offenses (a mean of 3.6 per offender), compared to a total of 76 convictions accumulated by the 52 comparison subjects with convictions for violent offenses (a mean of 1.5 per offender). Thus, the rate of conviction for a violent offense was 2.4 times greater among the violent offenders with schizophrenia than among the comparison subjects who were violent offenders.
Nine subjects in the schizophrenia cohort were charged with murder. Four were convicted, one was adjudicated insane, three were convicted of lesser offenses, and one was acquitted. No murder convictions were recorded among the comparison subjects, although one comparison subject was charged and acquitted.
Male subjects in the schizophrenia cohorts had significantly more lifetime-to-date convictions for violent offenses than the male comparison subjects (13.0% versus 2.9%) (odds ratio=5.0, 95% CI=3.6–6.9, p<0.001) and significantly more convictions for violent offenses in the 5-year period after their first admission (4.6% versus 0.7%) (odds ratio=7.3, 95% CI=3.9–13.8, p<0.001). Violent offenses were largely limited to male subjects, although the rate of violent offenses by female patients with schizophrenia in the overall sample was significantly higher than that in the overall sample of female comparison subjects (1.4% versus 0.3%) (odds ratio=5.4, 95% CI=1.6–18.6, p<0.003). However, there were too few convictions for violence among women to analyze the data separately by cohort.
Property-related offenses
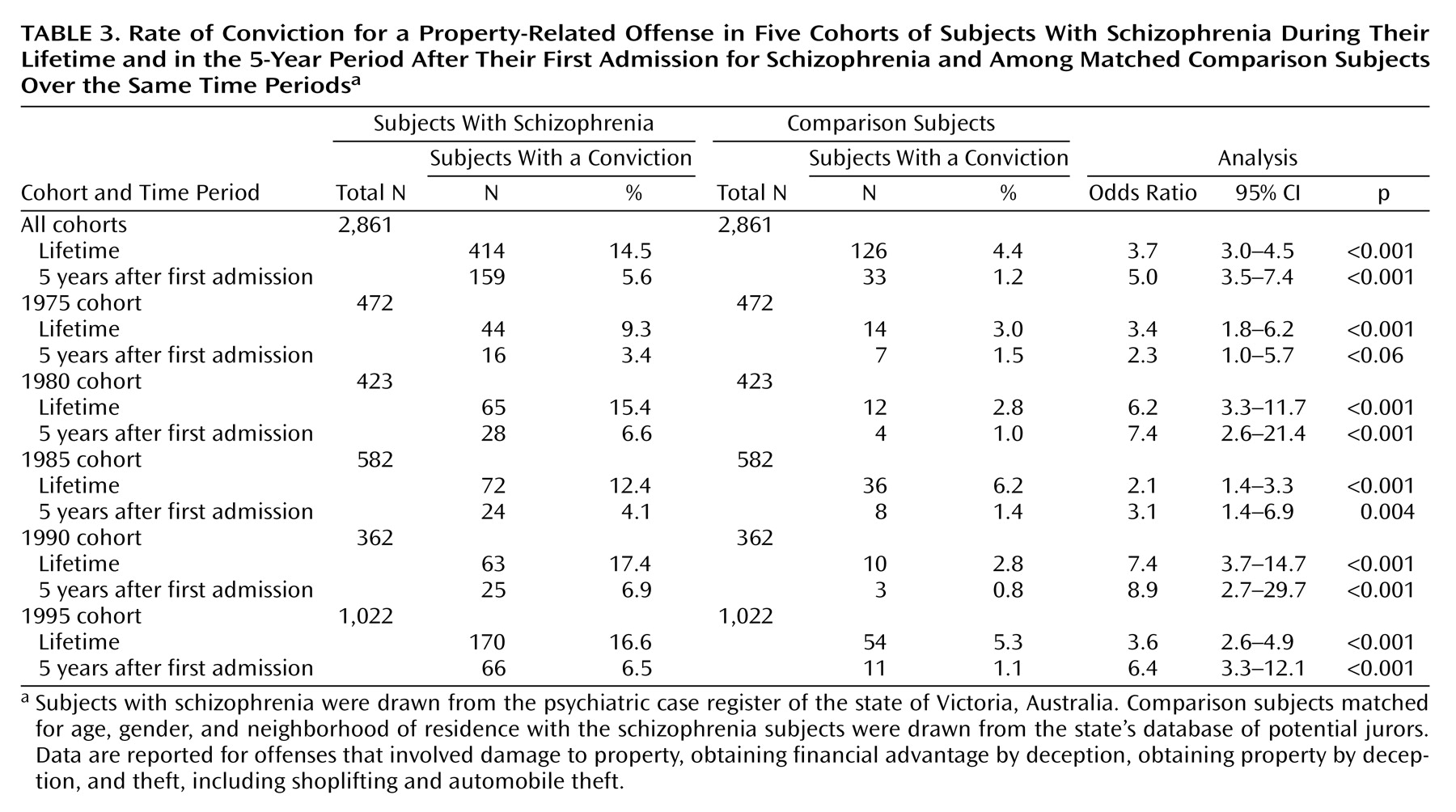
Property-related offenses were recorded for 14.5% of the patients with schizophrenia and 4.4% of the comparison subjects (
Table 3). Relative to the male comparison subjects, the male schizophrenia patients had significantly higher rates of property-related offenses during their lifetime to date (20.7% versus 6.2%) (odds ratio=4.0, 95% CI=3.2–5.0, p<0.001) and during the 5 years after their first admission (7.9% versus 1.6%) (odds ratio=5.3, 95% CI=3.5–8.0, p<0.001). The differences remained significant for each of the male cohorts. In the overall sample, female patients with schizophrenia had a significantly higher lifetime-to-date rate of property-related offenses than the female comparison subjects (5.6% versus 1.9%) (odds ratio=3.1, 95% CI=1.9–5.0, p<0.001) and a significantly higher rate for the 5 years after their first admission than the female comparison subjects (2.2% versus 0.5%) (odds ratio=4.4, 95% CI=1.8–10.8, p<0.001). However, the conviction rates were too low among women to allow a meaningful analysis by cohort. The rate of convictions for property-related offenses increased steadily from 1975 to 1995 among the schizophrenia patients, but the rate of increase was similar to that observed among the matched comparison subjects.
Substance-related offenses
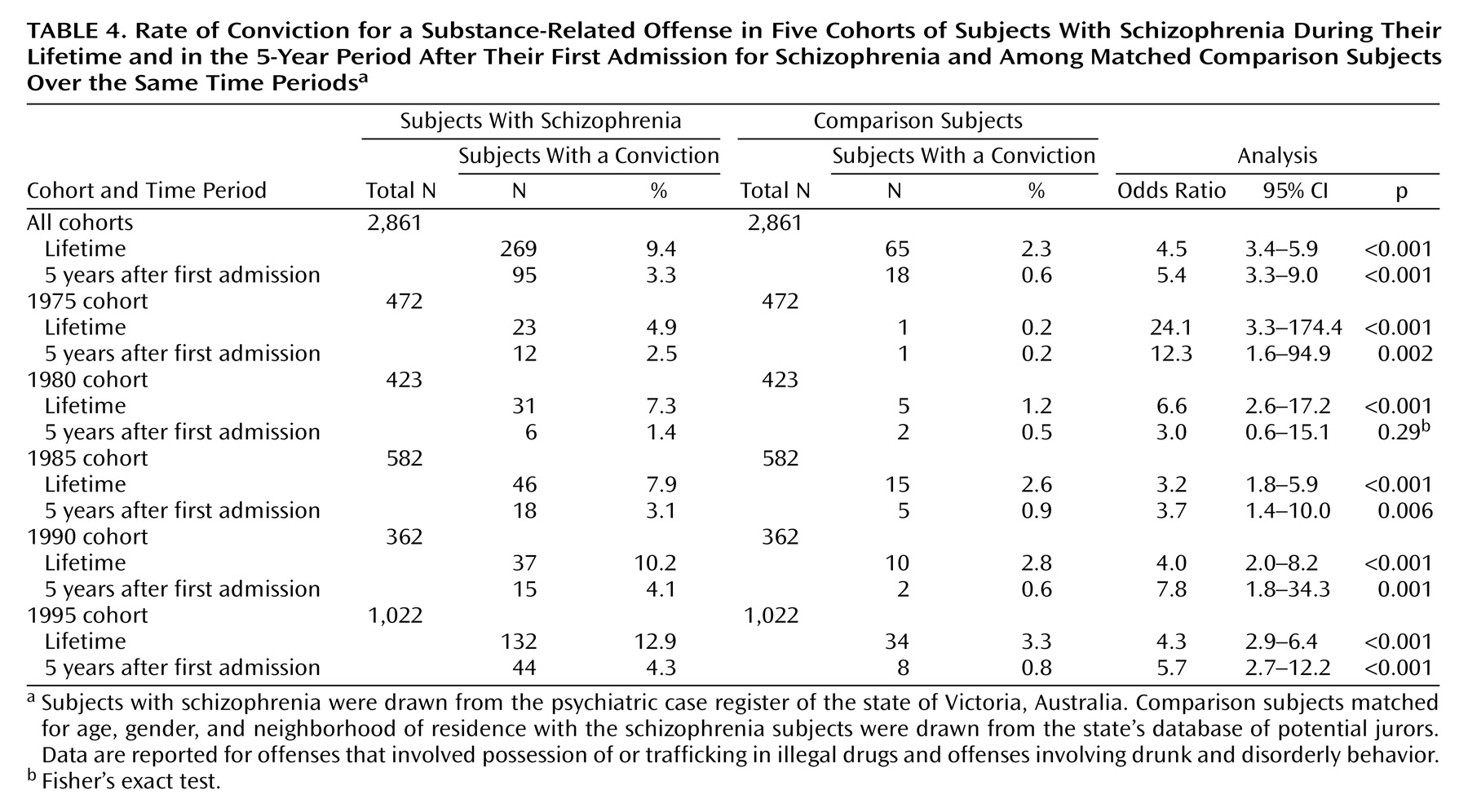
A total of 9.4% of the schizophrenia patients and 2.3% of comparison subjects had lifetime-to-date convictions for substance-related offenses (
Table 4). Male schizophrenia patients were significantly more likely to have such convictions than male comparison subjects in the total sample and in every cohort. The rates of substance-related offenses among female subjects were again too low for cohort-by-cohort analysis, although in the total sample, the female schizophrenia patients had a significantly higher rate of substance-related offenses than the female comparison subjects (1.9% versus 0.3%) (odds ratio=7.5, 95% CI=2.2–25.0, p<0.001). The frequency with which subjects with schizophrenia were convicted of a substance-related offense in their lifetime to date climbed steadily from 4.9% in 1975 to 12.9% in 1995, but this increase was matched by a proportionately similar rise among the comparison subjects (0.2% to 3.3%), resulting in no difference in the rate of increase between the schizophrenia patients and the comparison subjects (
Table 4).
Sexual offenses
Male schizophrenia patients were more likely than male comparison subjects to be convicted of a sexual offense during their lifetime (1.8% versus 0.7%) (odds ratio=2.6, 95% CI=1.3–5.1, p<0.01). However, the rates of sexual offending were too low to allow a meaningful analysis by cohort for male subjects. Only nine convictions for sexual offenses occurred among female subjects overall, which precluded meaningful analysis.
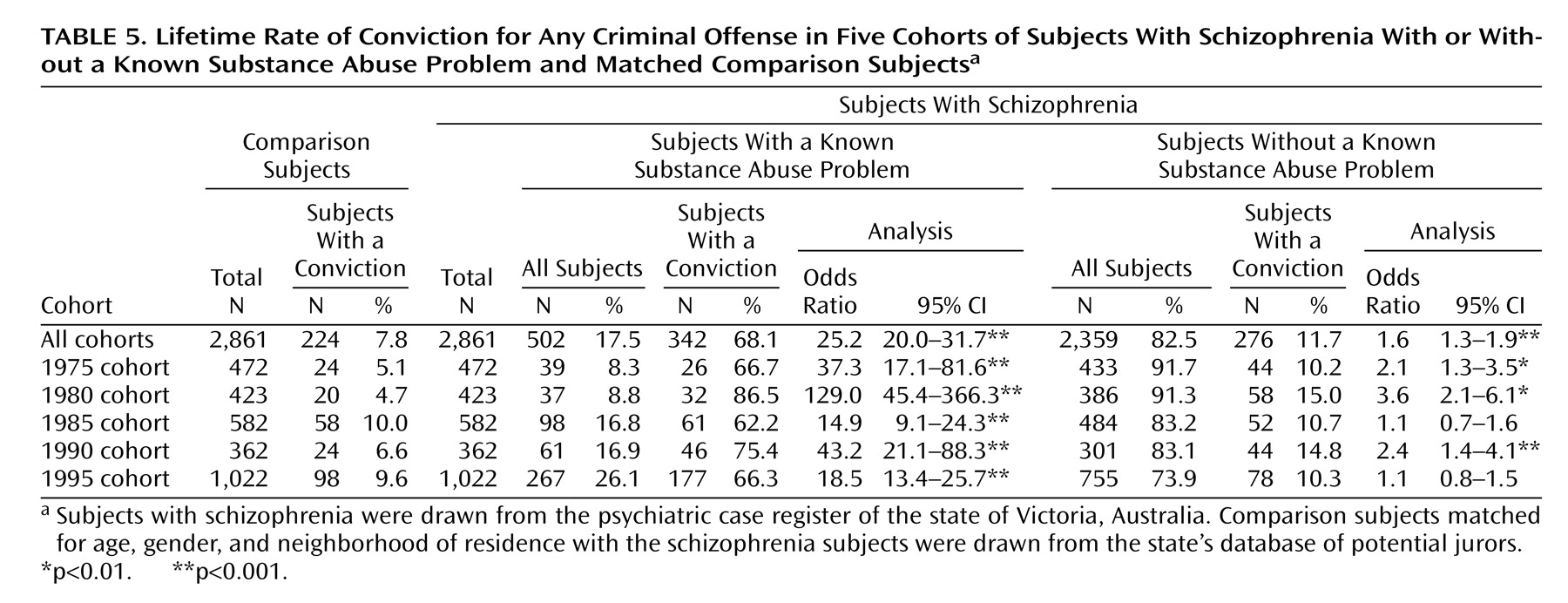
Interaction of Substance Misuse, Schizophrenia, and Offending
In the overall sample of schizophrenia patients, 327 (11.4%) had a record of a comorbid diagnosis of a substance use disorder and 94 of those subjects also had a conviction for a substance-related offense. Among the 269 schizophrenia patients (9.4%) who had a conviction for a substance-related offense, 175 (6.9%) subjects did not have a recorded comorbid diagnosis of a substance use disorder. Thus a total of 502 (17.5%) patients with schizophrenia had a known substance abuse problem; 421 of those subjects were male, and 81 were female. The schizophrenia patients who also had a known substance abuse problem were significantly more likely to have been convicted of an offense during their lifetime to date than those without a known substance abuse problem (68.1% versus 11.7%) (odds ratio=16.1, 95% CI=12.9–20.2, p<0.001). The relationship between a higher rate of total offending and known substance abuse problems held for both male schizophrenia patients (73.4% versus 17.3%) (odds ratio=13.2, 95% CI=10.2–17.2, p<0.001) and female schizophrenia patients (40.7% versus 5.2%) (odds ratio=12.5, 95% CI=7.4–20.9, p<0.001).
The rate of known substance abuse problems among patients with schizophrenia increased steadily from 8.3% in the 1975 cohort to 26.1% in the 1995 cohort (
Table 5). This increase paralleled the rise in the rate of a recorded diagnosis of a comorbid substance-related disorder among subjects with schizophrenia from 3.8% in 1975 to 19.0% in 1995. However, the proportion of subjects with criminal offenses remained relatively stable over time among both the schizophrenia patients with a known substance abuse problem (approximately 60%–80%) and those without a known substance abuse problem (10%–15%), except for the higher rate of nearly 87% among the subjects with a known substance abuse problem in the 1980 cohort.
The results for violent offending show a similar overall pattern, with a significantly higher rate in the patients with a known substance abuse problem, compared to those without a known substance abuse problem (26.1% versus 4.4%) (odds ratio=7.7, 95% CI=5.8–10.01, p<0.001), and a similar pattern in the various cohorts. Among male schizophrenia patients, 125 (29.7%) subjects with a known substance abuse problem had a conviction for violence during their lifetime to date, compared to 94 (7.4%) subjects without a known substance abuse problem. Relative to the rate of violent offenses in the male comparison subjects (2.9%), the rate of violent offenses was significantly higher both among male schizophrenia patients with a known substance abuse problem (odds ratio=14.1, 95% CI=9.9–20.1, p<0.001) and male schizophrenia patients without a known substance abuse problem (odds ratio=2.7, 95% CI=1.9–3.8, p<0.001). The proportions of patients in these two groups who had a violent offense remained relatively constant over the years, ranging from 4% to 5% for those without a known substance abuse problem and 20% to 30% for those with a known substance abuse problem.
Among the schizophrenia patients who did not have a known substance abuse problem, lifetime rates of offending remained significantly higher than those among the comparison subjects for total offending (11.7% versus 7.8%) (odds ratio=1.6, 95% CI=1.3–1.9, p<0.001), violent offenses (4.4% versus 1.8%) (odds ratio=2.5, 95% CI=1.8–3.5, p<0.001), and property-related offenses (7.6% versus 4.4%) (odds ratio=1.8, 95% CI=1.4–2.3, p<0.001). The rate of total offending among the schizophrenia patients with a known substance abuse problem differed markedly from the rate for the matched comparison subjects (
Table 5). A marked difference between these groups was also found for violent offending (26.1% versus 18%) (odds ratio=19.1, 95% CI=13.6–26.8, p<0.001). Relative to the rates of total offending among the comparison subjects, the rates in the schizophrenia patients without a known substance abuse problem were significantly greater in the 1975, 1980, and 1990 cohorts but not in the 1985 and 1995 cohorts (
Table 5). The difference in the rates of violent offending between the schizophrenia subjects without a known substance abuse problem and the matched comparison subjects was significant in 1975 (5.3% versus 1.1%) (odds ratio=5.2, 95% CI=2.0–13.9, p<0.001) but nonsignificant in 1995 (4.4% versus 2.8%) (odds ratio=1.6, 95% CI=0.9–2.6, n.s.).