The recent public debate concerning the death penalty has centered on the appropriateness of this punishment for violent crimes when committed by a person with “diminished capacity.” This question shifts the focus from whether the “punishment fits the crime” to whether it fits the criminal. Two types of exception to the rule of being equal before the law have been raised: an accused person who is mentally retarded and one who suffers from a mental disorder. This article is concerned with an additional category: a person accused of a violent act that was committed during an episode of temporarily impaired consciousness due to a sleep disorder. While there are standardized tests for establishing reduced mental capacity due to mental retardation and diagnostic criteria for determining the presence of a psychosis that limits rational thought, to my knowledge there is at this time no agreed-on protocol for establishing that an accused adult suffers from a sleepwalking disorder. This presents a particularly difficult problem because of the episodic, time-limited nature of such episodes and their complete reversibility once the person is fully awake.
Case reports of violence committed during a state of sleepwalking have appeared in the forensic literature over many years
(1–
9). What appears to be the first such report was written by Yellowless
(1) and appeared in 1878; it describes a 28-year-old man with a long history of night terrors with “a vivid feeling that some dreadful evil is impending.” He was tried for murder after smashing his 18-month-old son against the wall in the middle of the night, believing he was dealing with a wild beast about to attack his family. He was found not guilty after a statement by Lord Justice Clerk that the child was killed when the defendant was unconscious of the nature of the act by reason of somnambulism. Howard and d’Orban
(9) quoted a case first reported in 1933 of a 31-year-old firefighter who “woke to find himself battering his wife’s head with a shovel. The shock was so great he fainted and, when he realized his wife was dead, attempted suicide. He had no memory of getting out of bed, fetching the shovel and there was an entire lack of motive as he lived amicably with his wife” (p. 916).
These early case reports often described the behavior as a curiously isolated incident, out of keeping with that person’s usual behavior, without apparent prior motivation and after which no memory of the event was retained. This literature focuses on questions of responsibility for the harm done in light of the accused’s not having formed any prior intent, appearing not to have been in a conscious state at the time, and proving afterward not to be insane.
When such cases are brought to trial, the idea that it is possible to engage in complex injurious behavior while in a mixed state of sleep and wakefulness is usually met with considerable skepticism. As a result, there have been very different verdicts rendered in similar cases. There are also differences in the law applied.
This paper compares two cases of homicide in which I served as a sleep consultant pro bono; neither defendant was a patient of mine. In one case the defendant was judged under Canadian law as innocent owing to the act being a noninsane automatism. This case has been fully published
(10). The other defendant was judged guilty of murder in the first degree in a U.S. court. In both there was clear evidence that the homicide had been committed by the accused. The question raised was the degree of consciousness at the time. In each case, several nights of sleep recordings were conducted at a hospital in the same locality as the facility where each defendant was being held. The purpose of this report is to provide a second full report to examine similarities between these two cases in order to shed light on the state of mind during sleepwalking violence, to differentiate it from other diagnoses, and to provide guidance for further research.
Background on Sleepwalking Disorders
Sleep research has been slow in providing an understanding of sleepwalking in comparison to the rapid progress made in other sleep disorders. A diagnosis of sleep apnea is routinely made by identifying the number and severity of respiratory pauses and episodes of oxygen desaturation during a standardized all-night sleep study. The diagnosis of narcolepsy is aided by the presence of two or more episodes of sleep-onset REM sleep during a series of daytime naps following a night of recorded sleep. There are no such clear indicators of a sleepwalking disorder in the standard clinical sleep study.
Sleepwalking is one of a group of sleep-related behaviors that are relatively common in young children
(11–
15). Called the parasomnias, these also include sleep terrors and nocturnal enuresis. While disturbing to parents, childhood parasomnias do not usually pose a danger to the child or to others and typically go untreated. In a 1968 review of laboratory studies of parasomnias in children, Broughton
(15) argued that all three share a common characteristic: they occur during the first hour or two of the night after an abrupt arousal from slow-wave sleep. Further, since these events are not initiated from REM sleep, when most dreaming occurs, they are not psychologically based phenomena. Rather, they are a result of an abnormality in the transition from deep to highly activated sleep, that is, from non-REM to REM sleep. This abnormality aborts the usual shift into REM sleep, which, because of its accompanying loss of muscle tone, prevents simultaneous motoric behavior. Broughton also presented additional data showing that when aroused from slow-wave sleep, both sleepwalkers and comparison subjects have impaired responsiveness to visual stimuli but that this effect lasts significantly longer in sleepwalkers. This finding supports reports in the forensic literature that sleepwalkers display a period of mental confusion following an aggressive act before they regain full waking consciousness.
After publication of Broughton’s article, Bonkalo, a forensic psychiatrist, reviewed 50 reports of adult sleepwalking violence
(16). In this 1974 landmark article, the author pointed out several common characteristics: a marked predominance of men (47 of the 50 cases), an age range of 27 to 48 years, a strong childhood and/or family history of sleepwalking, nocturnal enuresis, nightmares, and agitation on awakening. He then offered a set of guidelines for the “Clinical and Forensic Evaluation of Cases.” The most important of these was that the “arousal is from early deep sleep usually about thirty minutes to two hours after sleep onset.” This has been confirmed in laboratory studies of children who sleepwalk
(12–
15). However, Bonkalo believed that adult forensic cases differ from the benign sleepwalking of children. In children, he stated, the movements are simple, slow, and more random. The child is more passive and can be led back to bed, while in adult sleepwalking violence, the movements are quick, impulsive, and inappropriate yet integrated and goal directed. Further, the person “when interfered with tends to be negativistic, resistive and assaultive”
(16, p. 407).
Since this publication, the number of descriptive cases and laboratory studies comparing large numbers of sleepwalking patients and comparison subjects has greatly expanded
(17–
22). These have generally supported Bonkalo’s observations of the predominance of males, with a strong childhood and genetic history of the various parasomnia disorders. The current DSM-IV-TR outlines six characteristics needed to support a diagnosis of sleepwalking disorder. The first four conform to those identified by both Broughton and Bonkalo. The six criteria are 1) repeated episodes of arising from sleep and walking about, usually from the first third of the major sleep period, 2) a blank staring face, relative unresponsiveness to others, and an inability to be awakened except with great difficulty during sleepwalking, 3) amnesia for the episode after full awakening, 4) some confusion or disorientation after awakening, 5) clinically significant distress or impairment in social, occupational, or other important functioning related to the sleepwalking, and 6) lack of evidence that the disturbance is due to the direct effects of a substance such as a drug of abuse, a medication, or a general medical condition. The text of DSM-IV-TR describes a range of severity from mild, simple behaviors to complex motor acts such as operating machinery with risk of injury to self or others.
DSM-IV-TR assigns the same classification number to a second diagnostic entity, sleep terror disorder, noting that these two may be difficult to differentiate. Among the differences listed are that sleep terrors begin with abrupt sitting up, a panicky scream, signs of intense fear, and autonomic discharge. Also the person “may actively resist being held or touched” and may demonstrate self-protective “swinging, punching or fleeing” (DSM-IV-TR, p. 635). The overlap of these two disorders may occur not only in the same person but also in the same episode. An event that begins as a night terror may progress into sleepwalking. That these two may also appear in the reverse order—a benign episode of sleepwalking may evolve into an aggressive episode if the ongoing behavior is interrupted suddenly—has not been generally recognized. This appears to be the case in both homicides to be reviewed here. These differed from previous cases of patients in my own laboratory. Of the 36 who have been studied for reported injury to themselves or others, only four were charged for the violence to another (
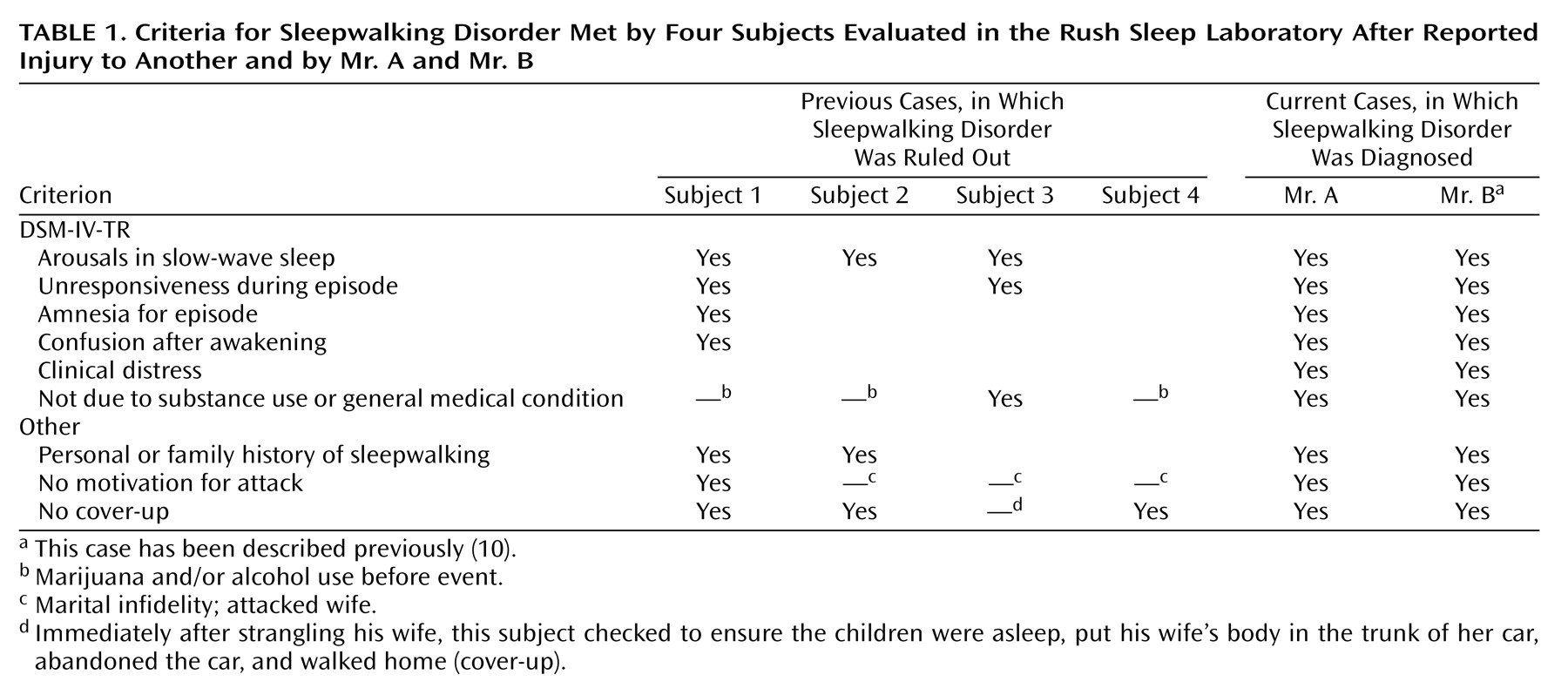
Table 1). In all, the violence was reported to be immediate on arousal and none of the subjects met the criteria for sleepwalking disorder(s).
Genetic vulnerability to the various parasomnias of childhood naturally extends into adulthood
(23), but their overt expression becomes less frequent. As maturation proceeds, the proportion of slow-wave sleep, which dominates the first 3 hours of sleep in preadolescents, is reduced and so too are the episodes of sleepwalking, sleep terrors, and nocturnal enuresis. It is likely that the episodes of violence that emerge in young adulthood do not represent a different pathology but a response to additional triggering factors, such as hormonal surges, substance abuse, and/or psychotropic medications
(3,
4,
9,
13,
24,
25).
The slow progress in understanding adult parasomnias may be due to the misconception that this is a rare disorder. This impression was corrected in the first epidemiological study
(26). It set the rate of adults reporting current episodes of sleep-related aggression at 2.1%. Although this rate is much lower than the estimated 15% of parasomnias in young children, it is surprisingly high given the potential seriousness of this disorder. Clearly, most adults have neither come to the attention of the courts nor sought help. Likely their behavior is of a milder, less dangerous nature.
In addition, a specific diagnostic sleep protocol to confirm the diagnosis is lacking. While the standard recording and scoring of EEG sleep stages
(27) is useful in ruling out other possibilities, such as sleep seizures, it has not yielded a unique signature of sleepwalking. DSM-IV-TR cites the sleep characteristics as a high number of transitions out of slow-wave sleep and low sleep efficiency but notes the sleep EEG is “otherwise not remarkable.” However, frequent partial arousals from slow-wave sleep are also found in sleep apnea and narcolepsy. One other “sign,” a burst of hypersynchronous delta waves prior to a behavioral arousal, is not a consistent finding and again not specific to this disorder
(28,
29). Unless a behavioral arousal from slow-wave sleep occurs during an evaluation, the sleep study is usually inconclusive.
Another reason this diagnosis has received little attention is its episodic nature. Progress in understanding the pathophysiology had to await either clear signs in the sleeping brain or the ability to elicit the behavior under controlled conditions. Many strategies have been used to provoke a behavioral arousal: preloading the patient with fluids to increase bladder pressure, touching the patient, or calling the patient by name during the first slow-wave sleep cycle. These have proved more effective in children than in adults. In my laboratory we have not had success in provoking adult sleepwalking by any of these methods.
Promising New Research
There are now several new approaches that have improved the differential diagnosis of sleepwalking violence. The first is a more refined scoring of the sleep EEG by means of power density analysis using fast Fourier transform. Three studies using spectral analysis have demonstrated differences between sleepwalkers and comparison subjects in delta power
(28–
30). Patients’ recordings have lower levels of slow-wave (delta) activity in the first sleep cycle than do those of age- and sex-matched comparison subjects. Patients also fail to show the decrease in delta activity across the night that is typical of normal comparison subjects.
A second promising advance is brain imaging. Bassetti et al.
(31) captured a behavioral arousal episode by using single photon emission computed tomography. This showed 25% lower activity in the frontal parietal association areas and greater activity in the thalamic cingulate circuits than in comparison subjects. Further, Bassetti et al. noted that stimulation of the cingulate cortex in normal humans results in motor, autonomic, and emotional responses similar to those observed in patients with sleepwalking or sleep terror.
Progress in provoking sleepwalking episodes in the laboratory by prior sleep deprivation has also been reported. When sleepwalkers and comparison subjects were deprived for 36 hours, not only were more behavioral arousals recorded, but there was a measurable increase in the complexity of the behavioral events after deprivation, as judged by blind ratings
(32). Other triggers for parasomnias suggested by case reports are alcohol, marijuana, and caffeine. Caffeine has been implicated in studies by Moldofsky et al.
(19) and by Howard and d’Orban
(9) and was a possible factor in the new case to be presented here.
Human leukocyte antigen (HLA) class II typing of the family members of sleepwalkers also appears to be promising. That there is a strong genetic component in parasomnias has been well established in twin studies
(23) and in families
(33). However, the mode of transmission has not been clear. Ongoing studies suggest that the DBQ1*05 allele may distinguish sleepwalkers from comparison subjects
(34).
All of these help define the brain state of this disorder. We now turn to another level of analysis: that of the mind state during sleepwalking violence. Many forensic case reports indicate that the sleepwalker was undergoing a period of emotional stress before an attack and that the aggression resembled an emergency response to a threat
(35,
36). This suggests that these patients offer a model for insight into interactions between the waking and sleeping mind.
Perception
One of the difficulties juries have expressed when faced with a case of sleepwalking violence is understanding how it is possible for an accused person to orient well in space, walk, climb, and drive without harm and yet not recognize the face of a loved one the sleepwalker is attacking. Studies of the neuroanatomy of the visual system have established that the pathways involved in guiding movement and in facial recognition are different. The pathway for visually guided movement terminates in the posterior parietal cortex, while that for recognizing faces and assigning meaning to visual stimuli terminates in the midtemporal cortex
(37,
38).
Broughton
(15) reported that sleepwalkers have a greater delay in reaction to visual stimuli when they are aroused from slow-wave sleep than do comparison subjects, and this finding was also noted by Kales et al.
(13). There are other apparent perceptual difficulties during sleepwalking episodes. In sleepwalking violence the sleepwalkers do not appear to hear their victims cry out, nor do they register pain when they hurt themselves. These suggest hormonal changes and/or brain pathways that may still be “asleep” while complex motor behaviors take place.
Motor and Affect Control
Juries have questioned how an accused person is able to carry out complex, nonviolent, seemingly purposeful motor behaviors over extended periods of time, such as working on a motorbike
(20), without waking before acting violently. There are now several published cases in which prior long-distance driving took place
(4,
10,
39). The total time before consciousness fully returns has been estimated to be as long as an hour. However, how or why some complex, but benign, behavior suddenly shifts into an emergency fight-or-flight response is puzzling.
Aggressive behaviors that erupt from sleep and are followed by amnesia suggest a dissociative disorder. Hartman et al.
(40) tested the hypothesis that sleepwalkers would have more psychological trauma in their histories and would score higher on a waking test of proneness to dissociate than would comparison subjects. Their data did not support this. In fact, sleepwalking violence has not been associated with any specific psychopathology. The results of personality studies are most often within normal limits. Only tendencies to overcontrol emotion and to have compulsive behaviors have been noted
(4,
10,
41).
Motivation
Perhaps the most vexing question for juries is that of motivation, since these attacks appear to be unpremeditated, to take place without awareness during the event, and to be followed by retrograde amnesia and remorse. Motivation was one factor for ruling out a diagnosis of sleepwalking violence in two forensic cases studied in my laboratory. In both, prior marital discord due to continuing infidelity suggested a possible motivation for the aggressive attack on the wife. Forensic reports often note extensive sleep deprivation before an aggressive event and suggest that the sleep loss was secondary to psychological stress
(5,
6,
10). Perhaps the sleepwalker’s “integrated, goal-directed behavior,” noted by Bonkalo
(16), represents a response to the waking stress.
In the belief that detailed descriptions provide useful guides to further research, I am presenting a new case of homicide (Mr. A) for which the defense argued that the act took place during a sleepwalking episode. An extensive pretrial workup included a complete neurological examination, psychological testing by a court-appointed psychologist, 4 nights of all-night sleep recording, and the development of a family pedigree of relatives with a history of sleepwalking, nocturnal enuresis, and sleep terrors. These data were ordered by the court to parallel those developed for the trial of another homicide defendant, Mr. B, and were included in a published report on that case
(10). Although the two accused men differ markedly in demographic characteristics, the homicides have many common features. Mr. A was older than Mr. B (42 versus 22 years), was better educated (Mr. A was an electrical engineer with an additional M.B.A. degree and Mr. B had not finished high school), and had higher social class (upper middle class) and income (Mr. B was unemployed and deeply in debt). Mr. A was 5 ft. 9 in. tall and was described as a wiry “nerd,” whereas Mr. B was a 6 ft. 5 in., 280-lb. “gentle giant.”
The Case of Mr. A
The subject of this report is aware of and has provided permission for the publication of his case.
Events Preceding the Homicide of Jan. 16, 1997
At the time of his wife’s death, Mr. A was employed at Motorola’s semiconductor plant in Arizona as a product manager with an annual income of about $100,000. He had been married for 20 years to his high school sweetheart. There were two teenage children, a daughter 15 and a son 12. He and his wife were both raised in the Roman Catholic Church. Mr. A became an active and committed member of the Church of Jesus Christ of Latter-Day Saints before his marriage. His wife joined him in this affiliation after they married. As Mormons, they neither smoked nor drank alcohol. Accounts of the marriage all describe them as a close and loving family, active in their community, and without financial, health, or marital difficulties. The children told police that differences between their parents were few and settled by discussions.
Mr. A is the eldest of five children. His parents both had problems involving alcoholism, and his father was abusive when drinking. Although he was not the target, Mr. A witnessed the abuse of his mother. The parents divorced when he was 17. His wife’s parents had been divorced earlier, and she was helpful to him during this upsetting period. He describes her as his best friend and the only girl he ever dated. After high school they attended separate colleges but continued dating during holidays and summers. They married in 1976, when they were both 20. Their long, happy marriage ended with her sudden death at his hands.
In April of 1996, 9 months before his wife was killed, Mr. A entered a period of high work-related stress. He was assigned to be project manager of a new product, a chip to be used in the disk drive of computers. It was Mr. A’s judgment that the project was doomed to failure as his company was far behind the competition in this development. He continued to work hard at trying to solve the problem. Work success was a very important element in his self-esteem. He held himself to a high level of competence. He was also afraid that he would be viewed responsible for a failure that would cost the company millions of dollars and would lead to the loss of jobs for members of his team. By December he felt he must advise upper management that the project should be shut down. He felt alone in his dilemma, caught between being seen as a quitter by those above him and as a betrayer by those who worked under him. He put in long hours and went to bed late as he approached a decision point. He reports feeling exhausted and depressed, and he began using caffeine tablets to stay awake at work. His sleep pattern alternated between 2 to 4 late nights of short, poor-quality sleep followed by a night of “crashing” early into a night of catch-up sleep.
The day of the homicide Mr. A arrived home between 7:00 and 7:30 p.m. and had dinner with his wife and children. During dinner he discussed his work problem with his wife. She advised him to just smile and tell his manager and team what they wanted to hear. He remembers saying that he had gone along too much already. His wife also asked him to see what was wrong with the filter for their backyard swimming pool. After dinner, his wife watched television, the children did homework, and Mr. A worked at his computer, preparing materials for teaching a church youth group the next morning. He led this group every morning before work. The children went to bed at 9:00 p.m. Mr. A went out to inspect the pool motor problem. He started work on it but reports that it became too dark for him to finish the repair. He put his tools into the trunk of his car in the garage. His wife was still downstairs on the couch watching television. He remembers kissing her good night and going up to bed somewhere between 9:30 and 10:00 p.m. He changed into pajama bottoms but did not remove his contact lenses before “crashing” into sleep. This is his last memory of the day.
The Homicide
The next memory Mr. A reports is of waking in bed and hearing his dogs barking and voices down below. He ran downstairs. Before he reached the bottom he was met by police with drawn guns, who ordered him to lie face down, handcuffed him, and asked, “How many people are in the house?” He answered, “Four,” unaware that his wife was lying dead in the pool. Mr. A was placed in the back of a squad car, where he waited for about an hour while the police completed their initial investigation. He could hear the police and emergency personnel close to the car talking about what was happening. From this conversation he gathered that his wife had been badly hurt. He thought the police must be hunting for the responsible person. He did not realize that she was dead nor that he was the one to be accused. That did not become clear to him until he was taken to the Phoenix police department for interrogation and the interviewing detective asked him repeatedly about his motive for killing her.
The Eyewitness
The police were called to the house by a neighbor who dialed 911 after looking over a common wall to see why dogs were barking and a woman screaming. As he reported to the police, the neighbor went to bed about 10:00 p.m. and got up about 10:30. What he saw was a body lying beside the pool. There was a light on in a second-story room of Mr. A’s house. Through the window he had a partial view of Mr. A moving from one room to another. Mr. A then reappeared in the backyard and stood staring blankly over the body; then he returned to the house but came back out through the garage door, pulling on heavy canvas gloves. The neighbor reports that he saw Mr. A drag the body to the edge of the pool and roll it into the water. When he realized that this was Mr. A’s wife, he called the police. The record shows that the call was made at 10:56 p.m. When the neighbor returned to look over the wall again, he saw the body floating in the pool. Mr. A was no longer visible. The presumption is that he had gone back to bed and was asleep until the noise of the police woke him.
The Medical Investigation
The medical examiner reported that Ms. A had suffered multiple stab wounds, 44 in all. There was blood beside the pool and more found in the pool. There were bloodstains on Mr. A’s work clothes, which the police found in the trunk of his car, and there was more blood on a knife. Some blood remained on Mr. A’s neck, and he had a fresh bandage on one hand. He seemed puzzled when these were pointed out to him during the videotaped interrogation and had no explanation of how these had been acquired.
The report from a medical examination of Mr. A indicates that he is in good health with an unremarkable health history. A neurological workup ruled out a seizure disorder or tumor on the basis of a clinical EEG in both waking and sleep and a magnetic resonance imaging scan of the brain. The report of the neurologist concludes that in his opinion the homicide was the result of a parasomnia rather than any primary neurological condition. A forensic psychologist administered an extensive battery of standardized tests to rule out psychopathology. These included an MMPI, a Thematic Apperception Test, a Rorschach test, and a sentence completion test. The results of these were all also reported to be within normal limits. Both children were interviewed, as were Mr. A’s mother and father, in the search for some explanation for this bewildering event. The children had slept through the attack. They did not hear their mother’s cries. They agreed that there was no dissension between their parents.
Sleepwalking Defense
A search of previous homicides led the defense attorneys to the case of Mr. B, in which the accused was acquitted on the grounds that he was sleepwalking. In Canadian and British law this was termed a “noninsane automatism.” Fenwick
(6) quoted the legal definition as, “The deed does not make a man guilty unless his mind is guilty. If, at the time of the offense, there is an absence of mind, so that any action carried out was automatic, then in law the defense of automatism is possible.”
Interviews of Mr. A’s relatives supplied many instances of his sleepwalking as a child. One later example, when he was 20 years old, involved some violence toward a sister when she attempted to restrain him as he tried to leave the house dressed in pajamas at about midnight.
As I had been an advisor on the case of Mr. B, I was asked to review documents relevant to the possibility that Mr. A had also been sleepwalking during the attack on his wife. Many similarities between the two cases were noted, as was their consistency with the Bonkalo criteria:
1.
The attack occurred following an arousal soon after sleep onset.
2.
The episode involved an extended period of complex, goal-directed motor behavior that was at first nonviolent, before repeated stabbing took place.
3.
The person attacked was well loved by the attacker.
4.
The victim was not recognized at the time.
5.
The attack was followed by a period of observed mental confusion.
6.
There was profound amnesia for the event.
7.
There was no apparent motivation for the attack.
8.
There was no attempt to cover up the crime.
9.
The accused had a history of childhood parasomnias that was substantiated by friends and relatives.
10.
The accused had been undergoing an extended period of psychological stress involving a sense of personal failure, shame, and self-recrimination without a good solution in view.
11.
The accused had been sleeping poorly for many nights before the event.
12.
There was no previous history of violence.
13.
The attacker was not taking any medication or using alcohol or illegal substances.
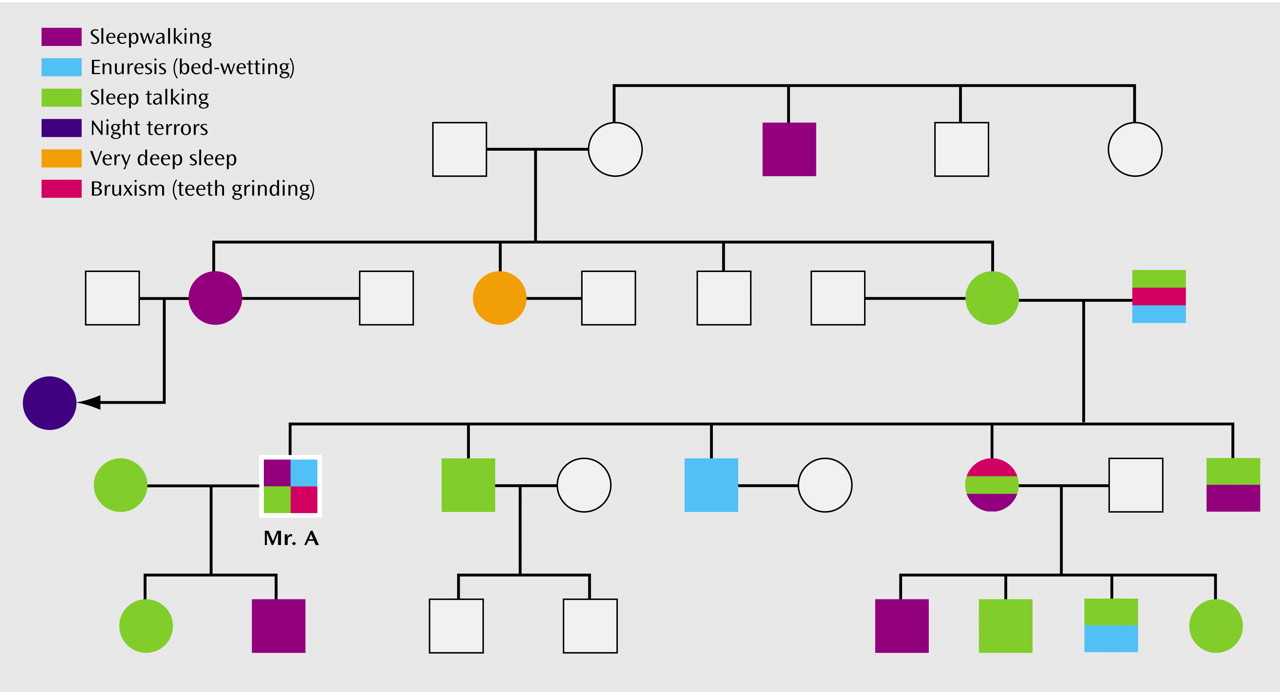
After reviewing the documents in the case of Mr. A, the family pedigree (
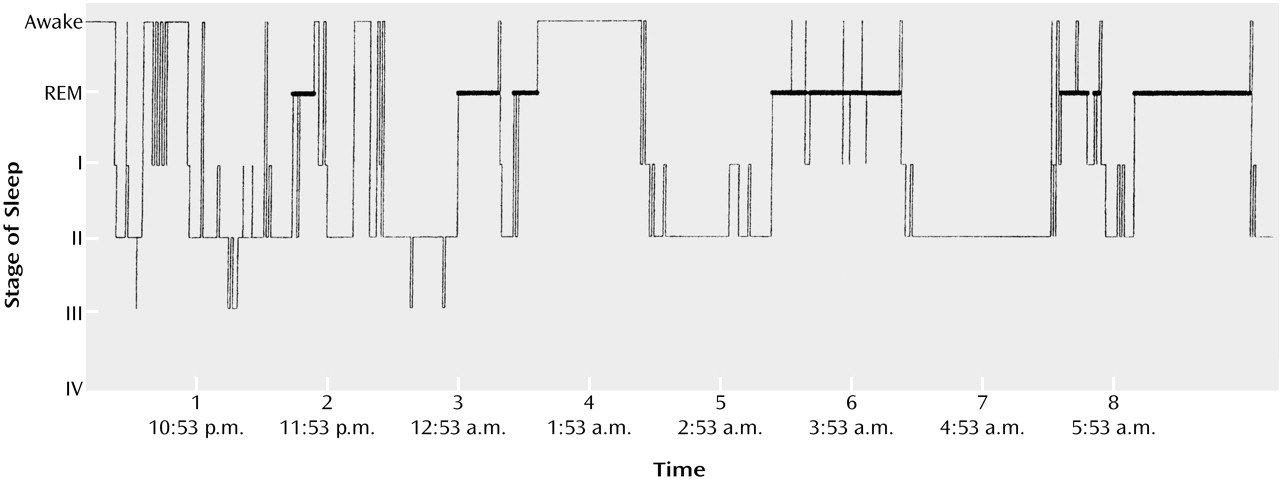
Figure 1), the psychologist’s report and the raw test responses, the medical and police reports, and the videotape of his initial police interrogation, I could not rule out the possibility of a sleep disorder. I requested an interview with Mr. A and asked that sleep studies be conducted. If a behavioral arousal from early non-REM sleep occurred or there were a significantly higher number of EEG arousals than expected, in the absence of other causes (indications of sleep apnea or narcolepsy), support would be added for this disorder. Four nights were requested, to allow him to adapt to the experimental setting, although the difference between the emotional circumstances of these nights to those of his typical home sleep could not be controlled. Three consecutive nights were uninterrupted. On the fourth night, the technician attempted to stimulate an arousal by using a sound stimulus. As the research identifying low delta power in these patients had not yet been published, these records were not subjected to power spectral analysis. They were scored according to the standard sleep stage criteria
(27) by the hospital technician and subsequently rescored by two independent, well-experienced sleep specialists. All nights illustrate a large number of arousals from early non-REM sleep and a significantly higher total number than expected on the basis of sex-specific age norms: the mean number of arousals for 40–49-year-old men is 4.67
(42, p. 58), and the mean for Mr. A across three nights was 26.5 (
Figure 2).
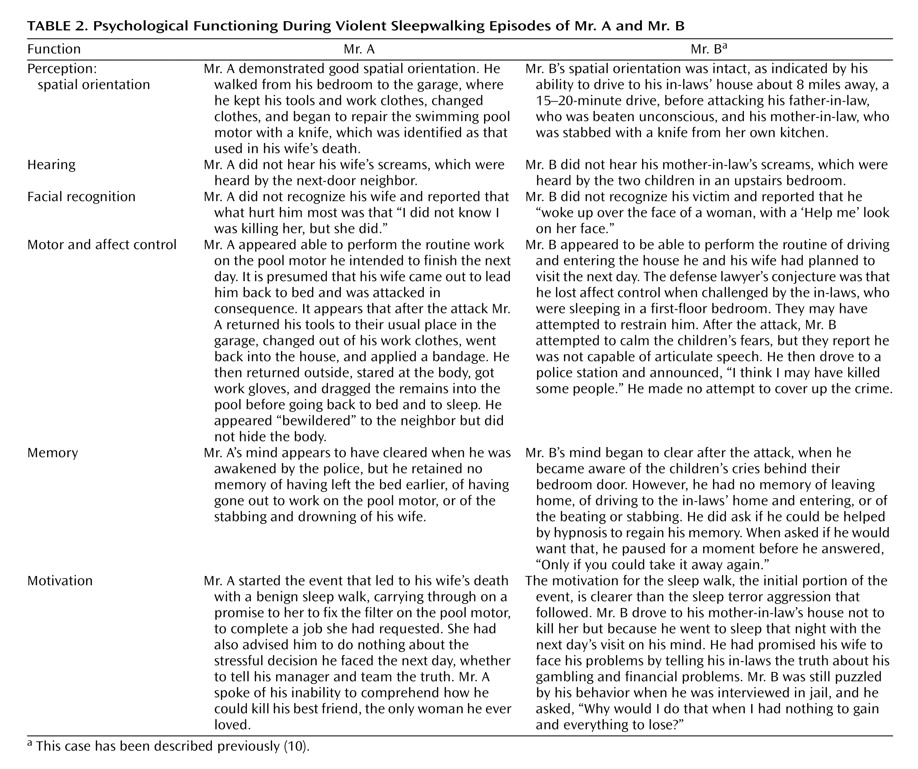
After an interview with Mr. A, I compared what I could deduce of his psychological functioning during and following the episode to that of Mr. B on the basis of the parallel documents from his file and my interview with each of them (
Table 2).
In neither case was the prosecution able to develop a motive for the attack: no financial gain, no bad relationship, no infidelity, only the demoralizing psychological stress of a sense of impending humiliation and failure to be confronted the next day. This was also suggested as a possible explanation in an earlier case
(2). In both Mr. A and Mr. B there was an intent to “do the right thing”; in the case of Mr. B, this was to tell his in-laws about his compulsive gambling and resulting debts, and for Mr. A this was to successfully finish the pool repair before telling his manager and team that he could not bring the work project to a satisfactory conclusion. Each man was halted while attempting an ego-restorative act and lashed out as if his life was in danger. Without the ability to recognize the person who stood in his way and while the higher cortical areas controlling judgment were partially blocked, the primitive impulse to attack took over. Only after the trial, when I reviewed the literature for this report, did the fact that Mr. A had begun using caffeine tablets to maintain wakefulness suggest a possible effect on his sleep. As a Mormon, Mr. A had not drunk coffee or tea for many years. The effect of the new substance may well have been a precipitating factor in an abnormal arousal
(9,
19).
Conclusions
The research reviewed here suggests recommendations for forensic cases. A standard protocol should be followed to rule out other diagnoses associated with violent behaviors, such as malingering, a fugue, temporal lobe epilepsy, complex partial seizures, and encephalopathy due to toxic agents. REM behavior disorder typically occurs in older patients whose episodes occur later in the night. A differential diagnosis between sleepwalking violence and REM behavior disorder can be confirmed by a standard sleep study. In REM behavior disorder the arousal is from REM periods that show inconsistent atonia, permitting behavioral dream enactment
(43). In contrast to the parasomnia patient, the patient with REM behavior disorder has vivid recall. The presence of family and personal histories of parasomnias should be investigated. At least 3 nights of digital sleep recordings should be ordered and should include one preceded by 36 hours of sleep deprivation. The sleep data should be analyzed both by sleep stage, using appropriate age and gender norms
(42), and by power spectral methods. All nights should be video recorded.
In general, physicians should be urged to include questions concerning parasomnia behaviors in their health history of adult patients, including use of any new medications or other substances. Adults who report continuing episodes of behavioral arousals from the first hours of sleep without awareness or recall should be counseled to avoid sleep deprivation and sleep schedule disruptions, and if they are undergoing periods of prolonged stress, they should receive preventive treatment. For many patients, 0.5 to 3.0 mg of clonazepam has effectively controlled parasomnias over long periods of time
(44). Mr. B has been successfully treated with this medication since his release. Mr. A remains incarcerated and untreated, as a sleep disorder was judged not to be credible in his case.
Continuing research into this disorder should be encouraged in all domains: genetic, hormonal, psychological, neuropsychological, and brain imaging, as well as sleep studies. Treatment programs should be tested for their efficacy over long time periods and should include single and combined trials of the benzodiazepines, hypnosis, stress management, and psychotherapy.
Sleepwalking violence offers a unique window into the mind-body interaction in the various states of waking, sleep, and the in-between state of parasomnia. The original question of responsibility for acts carried out in this state will be better answered when research has more thoroughly defined the functioning of the mind during this disorder.