As of this writing, more than a dozen antidepressants have been demonstrated effective for the treatment of depression and are available in the United States. At least one other medication has received Food and Drug Administration approval and is scheduled to be marketed this year, and others are in various stages of clinical trials. More antidepressants undoubtedly will be developed during the next decade that will work through putatively different mechanisms of action from the current classes of medications
(1–
3).
Although there is already a wide array of choices of antidepressants, there is little empirical evidence to guide clinicians in their selection. Most reviews of the antidepressant literature, including APA’s revised
Practice Guideline for the Treatment of Major Depressive Disorder (Revised)
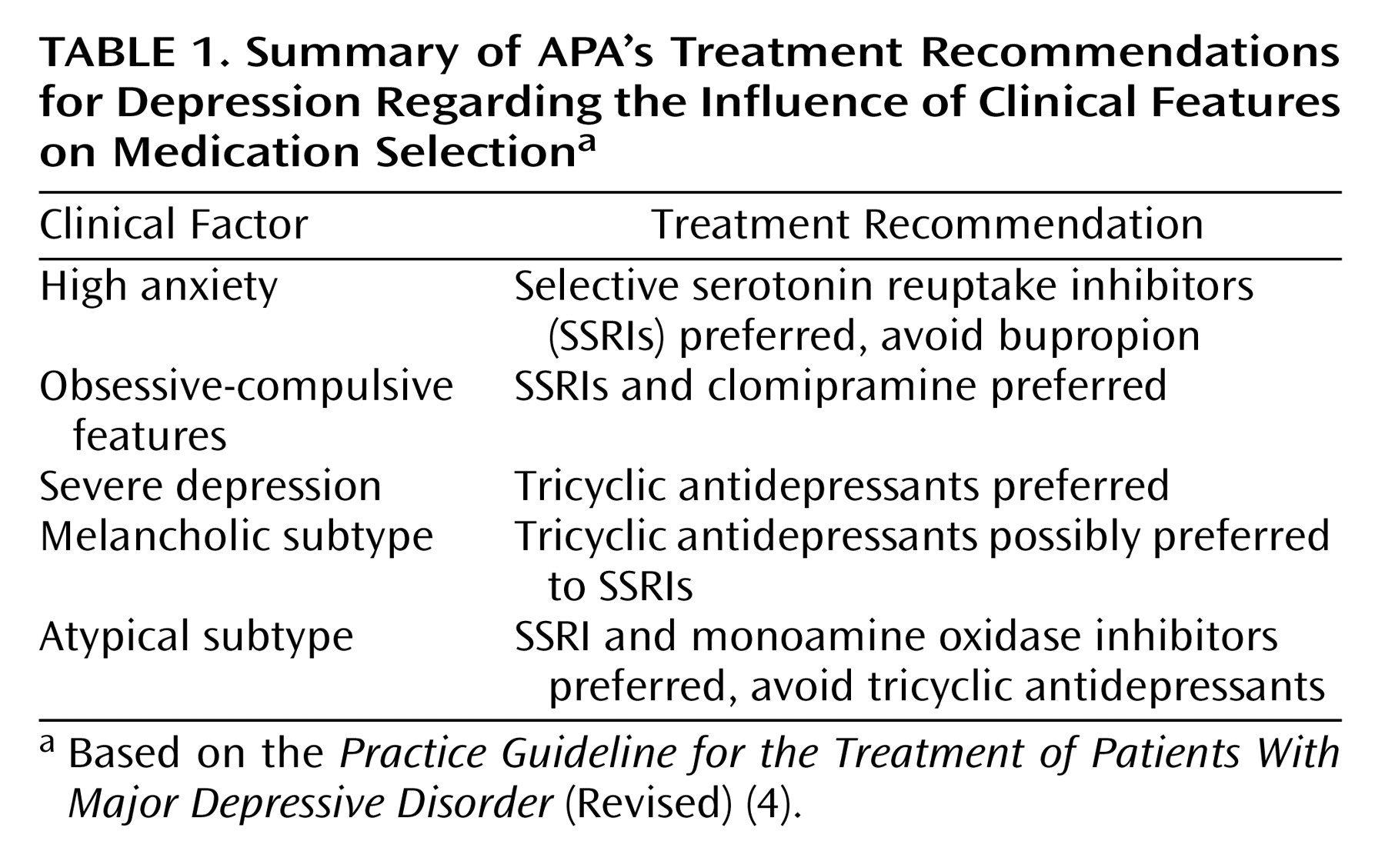
(4), conclude that these medications are generally equally effective. Although the APA practice guideline suggests that the choice of an antidepressant be based principally on side effects, tolerability, patient preference (although this is not elaborated upon in the guideline), and cost, the guideline also reviews evidence of differential treatment response related to patients’ clinical profiles. For patients with nonpsychotic, nonbipolar major depressive disorder, the guideline indicates that the presence of anxiety symptoms, atypical features, melancholic subtype, symptom severity, and borderline personality disorder may be associated with differential response to antidepressants. These suggestions are summarized in
Table 1.
What is most striking in the guideline’s review of evidence regarding differential antidepressant response is how limited in scope and utility are the data to guide the outpatient psychiatrist in selecting an antidepressant. Melancholia and severe depression are relatively infrequently encountered in the outpatient setting
(5). The most frequent comorbid conditions in depressed outpatients are anxiety disorders
(6,
7); the guideline simply says that bupropion may be anxiogenic and therefore should be avoided and that although monoamine oxidase inhibitors (MAOIs) may work well in depressed patients with anxiety, other medications are preferred. The guideline does not discuss the possible influence of specific symptoms on antidepressant selection.
In the absence of replicated empirical research guiding antidepressant selection, other than perhaps the use of MAOIs for atypical depression, it is of interest to examine what factors psychiatrists consider when prescribing antidepressants. As recently reviewed by Petersen and colleagues
(8), little research has examined the antidepressant prescribing practices of psychiatrists. Most of the existing literature has looked at prescribing trends over time, rather than the reasons for selecting particular medications
(9–
11). The study of the factors used by psychiatrists to choose antidepressants can highlight areas in which controlled research should be directed in order to confirm or disconfirm prescribing tendencies. In the absence of empirical evidence demonstrating the importance of considering patient factors when selecting an antidepressant, it is possible that nonclinical factors, such as marketing efforts, will assume greater influence over prescribing decisions. In addition, in the absence of empirical evidence demonstrating differential treatment response, it is more difficult to argue against formulary restrictions.
Petersen et al.
(8) surveyed 439 psychiatrists attending an annual psychopharmacology course regarding their first-line preferences in prescribing antidepressants in general and when treating depressed patients with certain clinical characteristics, such as high anxiety or an atypical subtype. They found that clinicians preferred different medications, depending on the characteristics of the depression, although the authors did not determine how often these clinical features actually influenced the choice of medication. They also asked which antidepressants were most likely to cause specific side effects, such as sexual dysfunction and agitation. Again, they found differences among the medications but did not determine how often the concern about particular side effects influenced prescribing behavior.
We are not aware of any prospective studies of psychiatrists’ decision making at the time antidepressants are being chosen. In the Rhode Island Factors Associated With Antidepressant Choice Survey
(12), we examined psychiatrists’ choices by having them complete a questionnaire immediately after they newly prescribed an antidepressant to a patient. In the present report, we describe which factors psychiatrists did and did not consider when prescribing an antidepressant medication for depression.
Method
The study was conducted from August 2001 until February 2002 in the Rhode Island Hospital Department of Psychiatry outpatient practice, a community-based, hospital-affiliated, multispecialty group practice of psychologists and psychiatrists. This private practice group predominantly treats individuals with medical insurance (including Medicare but not Medicaid) on a fee-for-service basis, and it is distinct from the hospital’s outpatient residency training clinic that predominantly serves lower-income, uninsured, and medical assistance patients. Ten psychiatrists participated in the study. The psychiatrists worked in three separate locations, and there was little interaction between the sites.
For 1,137 depressed patients who were newly prescribed an antidepressant for depression, the treating psychiatrist completed a 43-item yes/no questionnaire listing factors that might have influenced the choice of that antidepressant for the patient. The items listed on the form are presented in the tables in the Results section. The items on the survey were derived from review articles and treatment guidelines discussing variables differentiating the antidepressants, our knowledge of empirical literature of the treatment of depression, and clinical experience. The form was drafted by the first author, circulated for comment, and revised accordingly.
Clinicians were encouraged to complete the questionnaire for every depressed patient who was newly prescribed an antidepressant. The patients were not identified on the form. Thus, we were unable to check whether surveys were completed for all patients who were newly prescribed an antidepressant, although discussions with the treating psychiatrists suggested a high level of compliance. The psychiatrists wrote down the name of the medication prescribed, the patient’s age and gender, and whether the medication represented the initiation of treatment for the depressive episode, a switch from one medication to another, or an augmentation of another antidepressant. Antidepressant prescriptions to counteract the side effects of another medication or for nondepressive comorbid disorders were not included. After this, the psychiatrists indicated which of 43 listed factors influenced their choice of medication. Multiple factors could be checked. Three items (comorbid disorders, specific symptoms, and specific side effects) included a list of influencing factors as well as an open-ended question about other factors not listed. Because the forms were completed anonymously and patient-identifying information was not included on the form, the institutional review board of Rhode Island Hospital indicated that informed consent was not necessary. Patients could be taking other psychotropic medications at the time the antidepressant was chosen, although this was not recorded.
Results
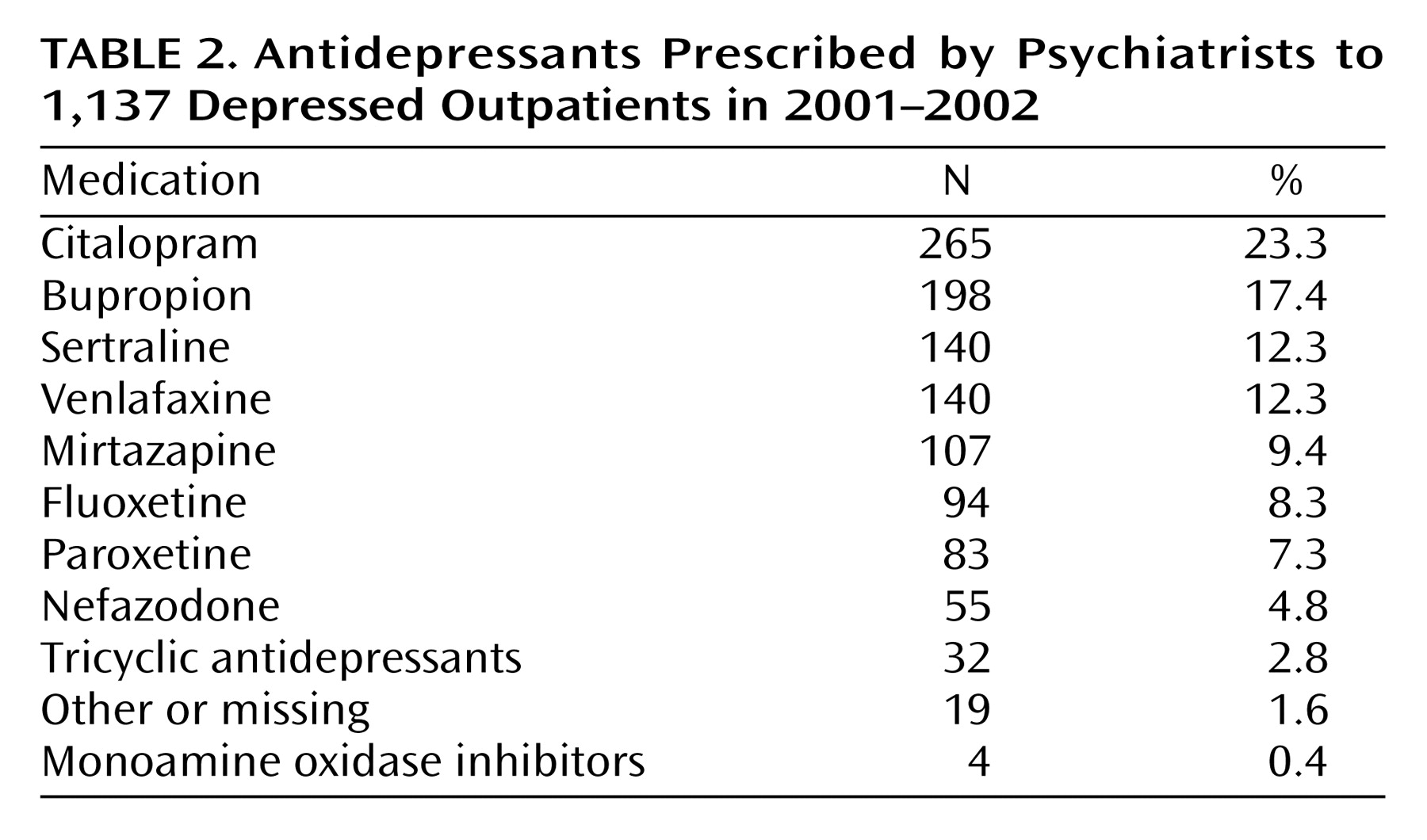
The majority of the 1,137 prescriptions were written for women (62.4%). The mean age of the study group was 42.0 years (SD=13.7). The majority of prescriptions were for the initiation of antidepressant treatment (N=669, 58.6%). Approximately 1/10 of the trials represented augmentations of existing regimens (N=102, 9.0%), and 26.6% (N=302) were switches from one medication to another. The type of medication trial was not recorded for 64 prescriptions (5.6%). The data in
Table 2 show the medications prescribed. About half of the prescriptions were for selective serotonin reuptake inhibitors (SSRIs). Older generation tricyclic antidepressants and MAOIs were infrequently prescribed.
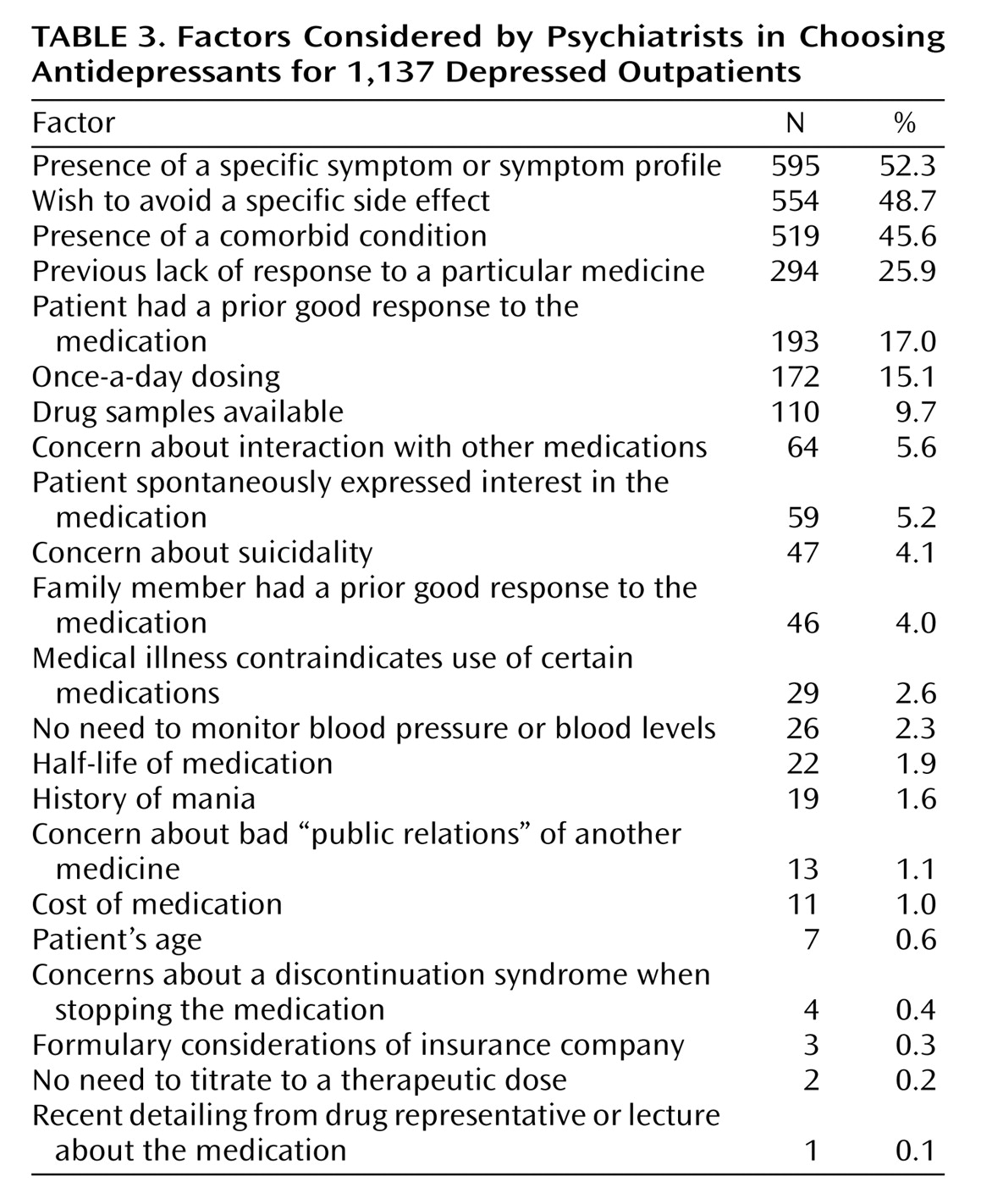
The most common influences on antidepressant selection were the avoidance of specific side effects, the presence of comorbid psychiatric disorders, and the presence of specific clinical symptoms (
Table 3). Prior treatment history, including a prior positive or negative response, was the next most frequently endorsed factor influencing medication choice. Some factors that have been frequently discussed in the literature, such as concern about discontinuation syndrome and drug-drug interactions, rarely influenced antidepressant selection.
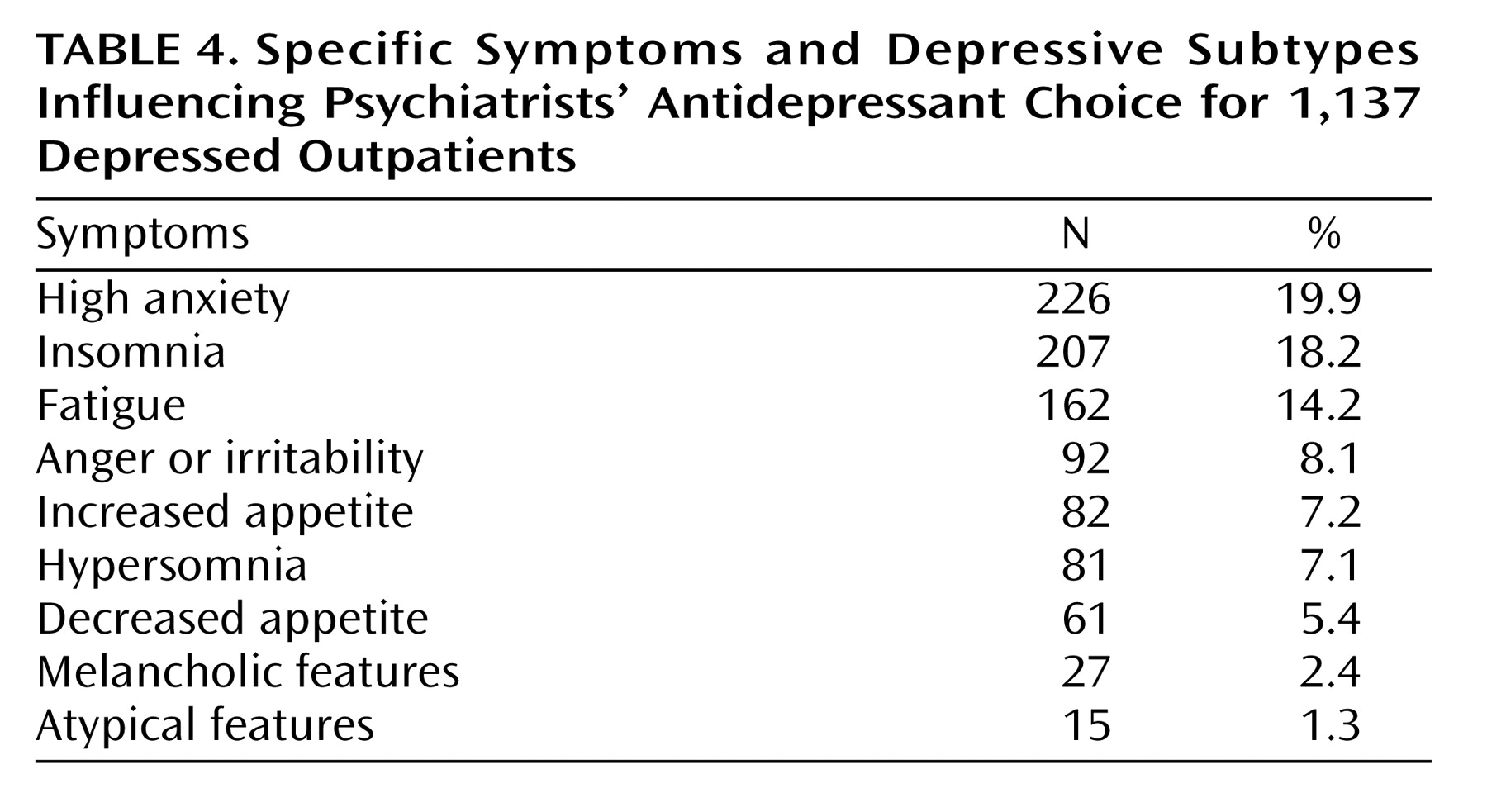
For more than half of the prescriptions, the presence of specific clinical features influenced antidepressant choice. The presence of insomnia, high levels of anxiety, and fatigue most frequently were reported to influence medication selection (
Table 4). Of interest, DSM-IV’s approach toward identifying phenomenologically homogeneous subtypes of major depressive disorder, based on the presence of atypical or melancholic features, rarely influenced the choice of antidepressant.
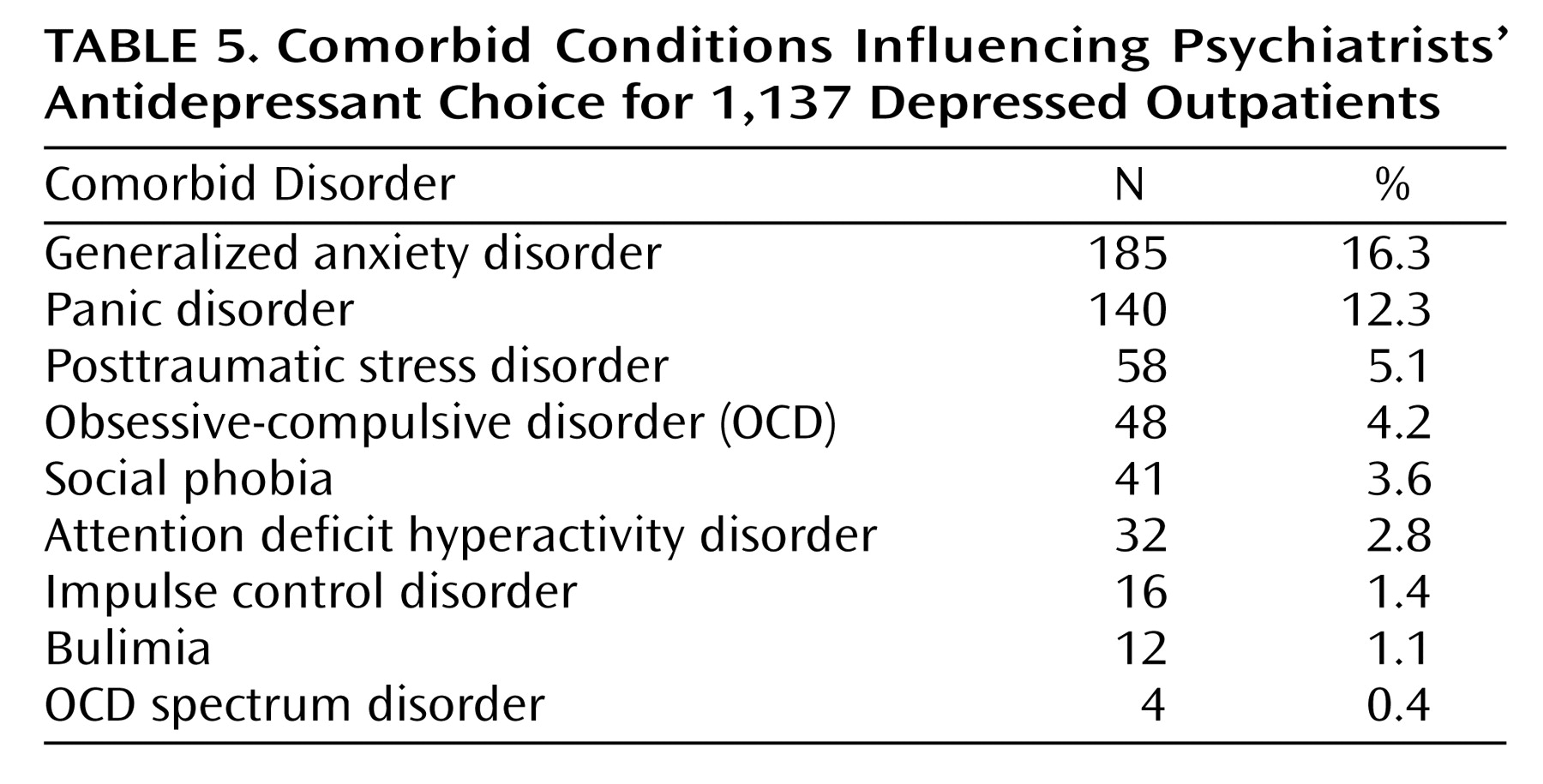
With regard to the influence of diagnostic comorbidity, the presence of comorbid anxiety disorders, particularly panic disorder and generalized anxiety disorder, most frequently influenced antidepressant selection (
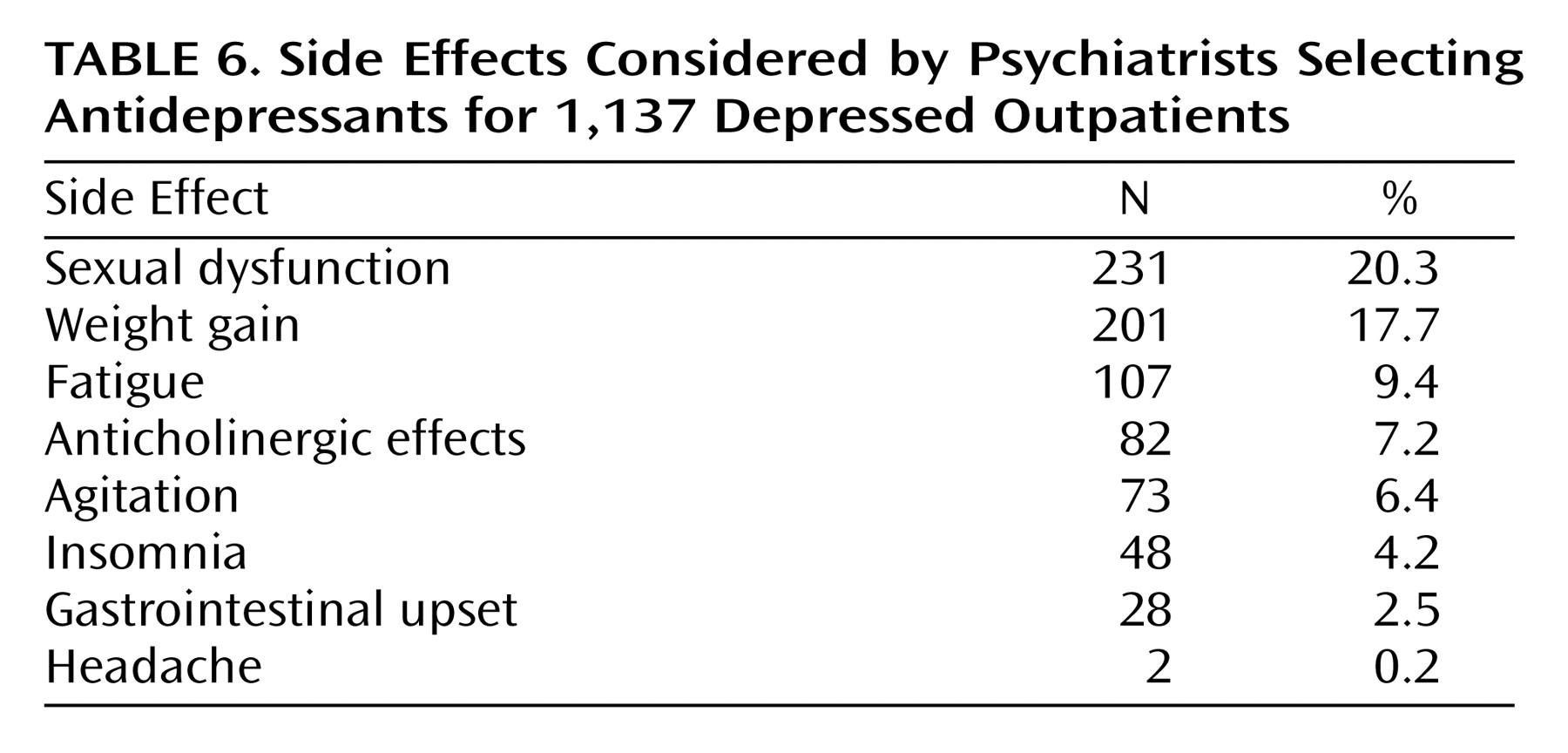
Table 5). Concern about the occurrence of sexual dysfunction and weight gain were the side effects that had the greatest impact upon medication selection (
Table 6).
Discussion
The objective of the present study was to better understand the factors considered by psychiatrists when selecting an antidepressant for depressed patients. Because relatively little research has examined which clinical features are associated with differential response to the newer generation of antidepressants, a study of psychiatrists’ prescribing practices highlights priorities for future controlled research.
Our results suggest that one priority area is the treatment of depression with coexisting anxiety symptoms/anxiety disorders. Several studies of clinical study groups have reported that nearly half or more of depressed patients have a concurrent anxiety disorder
(6,
7). An even higher proportion of depressed patients have coexisting anxiety when the construct is expanded to include high levels of anxiety symptoms as well as diagnosable anxiety disorders
(13). Anxiety in depressed patients is thus highly prevalent, and it frequently influences the choice of antidepressant; however, we are unaware of any studies demonstrating the superiority of one medication over another for this large subgroup of patients
(14). In fact, some studies have failed to demonstrate differential response to antidepressants of different classes. For example, Rush and colleagues
(15,
16) have published two independent reports that failed to find a difference in response to bupropion and sertraline in depressed patients scoring high on the Hamilton Rating Scale for Anxiety. This contrasts with unpublished analyses from the present data set that found that psychiatrists were strongly disinclined to prescribe bupropion when anxiety features influenced medication selection.
Antidepressant choice was frequently guided by the presence of particular symptoms. The APA treatment guideline did not discuss using individual symptoms as the basis of antidepressant selection. Rather, the guideline suggested that atypical and melancholic subtyping are associated with preferential medication response; however, the psychiatrists in the study rarely based treatment decisions on these approaches toward subtyping. Because melancholia is relatively rare in depressed outpatients, it is not surprising that this feature was not commonly a significant factor in choosing a medication. Also, the survey worded the melancholia item as “melancholic features/severe depression.” While these two constructs are related, they are not synonymous
(17), and this might have reduced the frequency of endorsement of this factor. Atypical depression is more common than melancholia, although the validity of the criteria used to identify the subtype has recently been called into question
(18). Although atypical subtype was an uncommon reason for choosing an antidepressant, the reverse vegetative symptoms characteristic of the subtype commonly influenced selection. Also, the best evidence regarding differential treatment response favors using a rarely prescribed class of medication: MAOIs for atypical depression. Perhaps if differential response were related to a newer generation antidepressant, it would have a greater influence on treatment decision making.
A limitation of the present study was that the data were collected from a small group of 10 psychiatrists treating patients in a private practice setting in New England. Although the psychiatrists worked in three different locations, presumably, there was some influence on each other’s practices. It is possible that there are systematic differences between psychiatrists in different regions of the country in the reasons used to select antidepressants. The reasons given for prescribing seem in line with current wisdom; nonetheless, replication of the findings in other sites is warranted.
Another limitation is that not all possible factors influencing antidepressant choice were included on the survey. For example, the presence of a substance use disorder, axis II condition, or dysthymic disorder might have affected antidepressant choice. However, the questions about symptoms, comorbid conditions, and side effects each included an item labeled “other” with a space to write in a variable that had not been listed, and for each of these variables, the “other” item was selected in less than 5% of the patients.
A strength of the study was that economic factors did not significantly influence prescribing. At the time of the study, there were no formulary restrictions influencing prescribing habits, and tiered copayments were not widespread and thus did not influence decisions regarding choice of antidepressant. Also, the only newer-generation medication available in generic form was bupropion, although this was infrequently prescribed because of the availability of sustained-release bupropion, which was not available in generic form. Consequently, our results more accurately reflect the influence of patient and medication factors on psychiatrists’ selection of antidepressants.
The depressed patients in the study had health insurance and were treated in a community-based, general adult clinical practice. As described in other reports from our group, the majority has comorbid conditions
(7), and most would not qualify for antidepressant efficacy trials
(19). Many patients were administered other psychotropic medications, although we did not systematically record these. We could have examined the factors influencing antidepressant choice in depressed patients without comorbid conditions who were not taking other psychotropic agents. However, this would have markedly limited the generalizability of the findings.
In general, the overall prescribing patterns of the clinicians represented national prescribing trends. The SSRIs as a class were the most frequently prescribed medication, and the MAOIs and tricyclic antidepressants were the least frequent. The frequency of the other newer generation antidepressants also roughly paralleled national data. However, citalopram was more frequently prescribed than the other SSRIs, and this was at variance with national data. This might reflect the fact that it was the most recently approved of the antidepressant medications and thus was more likely tried for those patients who did not respond to prior drug trials.
The results of the study have implications for studies comparing antidepressants that are not based on random assignment to treatment group. For example, large-scale studies that identify groups through pharmacy records to compare compliance with medication or the likelihood of taking an antidepressant 6 months after it is first prescribed cannot assume that patients given different medications are clinically similar. In fact, preliminary analyses of the data from the Factors Associated With Antidepressant Choice Survey
(12) found significant differences between the medications in the reasons ascribed to their selection. Thus, in studies based on a nonrandomized design, differences between medications may be due to group differences in the clinical characteristics of the patients rather than to inherent properties of the medication. Future reports from the Rhode Island Factors Associated With Antidepressant Choice Survey will examine differences between specific medications.