Psychological trauma occurs at high rates in children and adolescents
(1), and posttraumatic stress disorder (PTSD) in this age group has attracted considerable clinical and research interest. However, the diagnosis of acute stress disorder, introduced in DSM-IV, has received relatively little attention in younger populations
(2), despite a growing body of research in adults
(3). Unlike PTSD, which is diagnosed at least 4 weeks after trauma, acute stress disorder is diagnosed 2 days to 4 weeks after trauma. Acute stress disorder also differs from PTSD in being explicitly conceived as a dissociative response to trauma requiring at least three of a possible five dissociation symptoms. An important public health marker of the utility of acute stress disorder is its ability to predict later PTSD, thus allowing clinicians to focus resources on susceptible individuals
(4). In adults, acute stress disorder is a good predictor of later PTSD
(5,
6), but the dissociation symptoms appear to add little
(7).
Several studies have examined acute stress disorder symptoms in younger populations
(8–
12). However, only one study
(11) examined the power of the acute stress disorder diagnosis (derived solely from questionnaire responses) to predict later PTSD. Results indicated that acute stress disorder had low predictive sensitivity (unlike in adults) but that this was improved by
removal of the dissociation items. Further research on the predictive utility of acute stress disorder in younger samples is urgently needed.
To our knowledge, the present study is the first to assess acute stress disorder in children and adolescents using structured clinical interview. Participants were assessed 2–4 weeks and 6 months after physical assault or motor vehicle accident. These events were selected because both are common, single-incident traumas with comparable rates of acute stress disorder in adults
(5,
6). Our goal was to compare the utility of diagnoses of acute stress disorder, subacute stress disorder (acute stress disorder minus the dissociation criterion)
(3), and “early PTSD” (PTSD without the duration criterion)
(7) in predicting later PTSD.
Method
Children and adolescents (10–16 years old) who were treated in a London emergency department following motor vehicle accident or assault met study criteria (N=343). One hundred nineteen (34.7%) of these patients could not be contacted because of incomplete emergency department records, two (0.6%) were immediately referred for treatment, and 116 (33.8%) declined to participate. The 106 children and adolescents (30.9%) who consented to participate were assessed within 4 weeks. Of these, 93 (87.7%) completed an initial clinical interview and 64 (60.4%) completed a second interview at 6 months. The mean age of the 93 patients who completed the initial interview was 13.9 years (SD=1.9); 33 were girls.
There was no difference between participants and nonparticipants in terms of sex, type of trauma, injury severity, or ethnicity, although participants were significantly younger (nonparticipants’ mean age=14.8, SD=1.9) (t=1.98, df=364.1, p<0.05). Participants reinterviewed at 6 months were no more or less likely than participants not reinterviewed to meet criteria for initial acute stress disorder. After description of the study, written informed consent from both children and their caregivers was obtained for all participants.
The child version of the Anxiety Disorders Interview Schedule for DSM-IV
(13) was used to diagnose acute stress disorder and PTSD. This instrument is a structured interview schedule with good psychometric properties
(13,
14) for the assessment of anxiety disorders in young subjects. It does not include the dissociative symptoms of acute stress disorder. Therefore, we designed a number of supplementary interview items (available from R.M.-S.) to assess these symptoms, guided by DSM-IV and existing adult acute stress disorder interview schedules
(15).
Subacute stress disorder was defined as the full acute stress disorder diagnosis minus the dissociation criterion. Early PTSD was defined as PTSD at initial assessment minus the duration criterion
(7). Internal reliabilities for acute stress disorder, subacute stress disorder, and early PTSD diagnoses in the current study were high (Cronbach’s alpha=0.85–0.87). There was unanimous diagnostic agreement between independent raters for 11 initial and 10 follow-up interviews (kappa=1.00).
Results
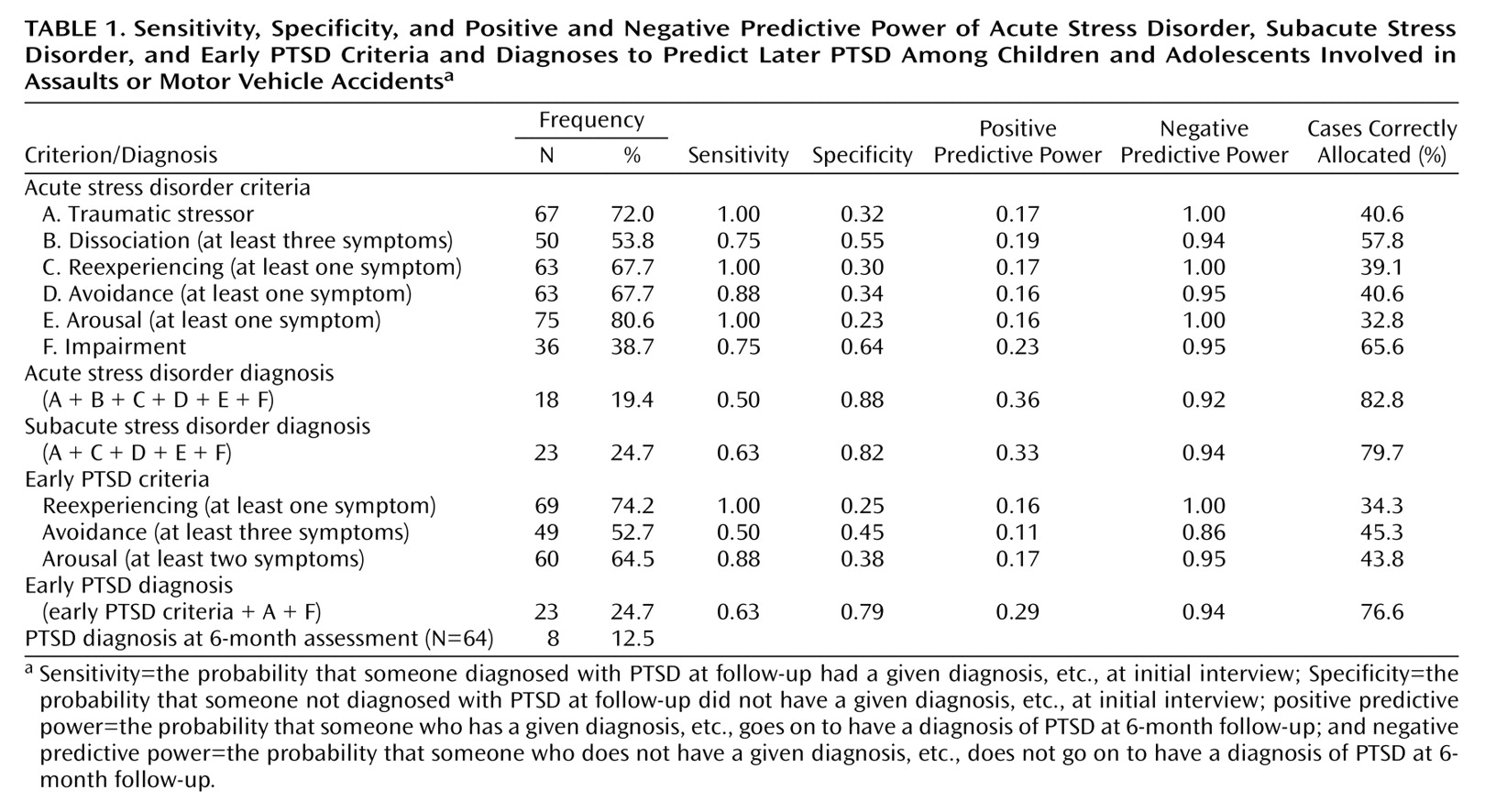
Table 1 shows how many children and adolescents met criteria for acute stress disorder, subacute stress disorder, and early and later PTSD. Chi-square analyses revealed no significant differences in prevalence for any diagnosis between those exposed to assaults and those involved in motor vehicle accidents.
Table 1 also shows the sensitivity, specificity, and positive and negative predictive power of the individual symptom criteria and the acute stress disorder, subacute stress disorder, and early PTSD diagnoses at initial interview to predict later PTSD, as well as the number of later PTSD cases that were correctly diagnosed by each criterion or diagnosis. Subacute stress disorder was the diagnosis that gave the best balance of sensitivity and specificity.
We used logistic regression to examine whether the acute stress disorder dissociation criterion explained any unique variance in later PTSD. Subacute stress disorder was entered in the first step, resulting in a significant model (χ2=6.56, df=1, p<0.01) and accounting for unique variance (Wald χ2=6.33, df=1, p<0.01). Entering the dissociation criterion in the second step did not significantly improve the model’s ability to predict later PTSD and did not account for any unique variance.
Discussion
The rate of acute stress disorder in this group of children and adolescents (19.4%) is similar to that found in adults
(5,
6) but slightly higher than in other child studies
(8,
11). As in adult studies, acute stress disorder occurred at similar rates among subjects involved in assaults or motor vehicle accidents
(5,
6).
The acute stress disorder diagnosis was a good predictor of later PTSD at follow-up, correctly classifying 82.8% of PTSD cases. However, subacute stress disorder provided a better balance between sensitivity and specificity at predicting later PTSD than full acute stress disorder. Furthermore, regression analysis revealed that the dissociation criterion did not significantly enhance the ability of subacute stress disorder to predict later PTSD. As in the adult literature
(7), acute stress disorder and early PTSD were equally effective predictors of later PTSD.
The study had two important limitations. First, the relatively small number of subjects may have weakened statistical power. Second, the study group comprised older children (essentially preadolescents) and adolescents. Studies examining acute stress disorder in larger and younger populations are therefore needed.
In conclusion, the acute stress disorder diagnosis is a good predictor of later PTSD in children and adolescents. However, our data indicate no unique role for the dissociation criterion of acute stress disorder in these patients.