Continuation of antidepressant therapy for depression beyond the acute phase of treatment is widely recommended as a means of consolidating treatment response and reducing the risk of relapse
(1–
3). However, despite broad consensus regarding the clinical importance of continuing antidepressant therapy for 4 or more months
(1–
4), there is accumulating evidence and growing concern that substantial numbers of patients discontinue antidepressant treatment during the first several weeks of treatment.
Early discontinuation of antidepressant treatment has been demonstrated in several clinical contexts. High rates of early antidepressant discontinuation have been documented in Medicaid patients
(5), privately insured populations
(6), managed pharmacy benefit plans
(7), and specialty mental health
(6,
8,
9) and primary care
(10,
11) practices. In one large primary care group practice, for example, approximately one-third of patients discontinued antidepressant therapy within 1 month and approximately one-half discontinued within 3 months of initiating treatment
(11).
Little is known about individual determinants of early discontinuation of antidepressant therapy in the community. In privately insured populations, sociodemographic characteristics tend not to predict risk of early antidepressant discontinuation
(12). In one group of privately insured patients, for example, early antidepressant discontinuation was not significantly related to patient age, gender, race, marital status, education, or employment status
(12). A separate study of privately insured primary care patients also reported that patient age, sex, and education were not differentially related to antidepressant continuity
(13). In contrast, female sex, older age, white race/ethnicity, and more years of education increased the likelihood of receiving guideline-consistent care in a nationally representative sample of adults with probable anxiety or depressive disorders
(14). In this study, higher patient income and the presence of health insurance did not increase the likelihood of receiving guideline-consistent care
(14).
Some evidence suggests that medication choice and tolerability may influence the duration of antidepressant treatment
(15–
18). Observational studies from several treatment settings indicated that patients treated with older tricyclic antidepressants are more likely to discontinue their medications within the first 4 weeks
(9,
11) to 6 weeks
(19) of treatment, compared with patients treated with newer classes of antidepressants. In one randomized, controlled trial, patients from a private health maintenance organization who were initially treated with fluoxetine were more likely than patients treated with imipramine or desipramine to continue taking their initial medication
(20,
21). However, the extent to which medication choice influences treatment duration in community practice remains unknown.
In privately insured populations, the provision of psychotherapy has also been linked to longer durations of antidepressant treatment for depression
(9,
18). Whether psychotherapy is associated with greater continuity of antidepressant treatment in the general population is also unknown.
In the current analysis, we examine sociodemographic, service access, and clinical correlates of continuity of antidepressant therapy in a nationally representative sample of adults initiating a new episode of antidepressant treatment for depression. We first examine the characteristics of patients who discontinued antidepressant treatment during the acute (0–30 days) phase of treatment. Among patients who completed the first 30 days of antidepressant therapy, we compare the characteristics of patients who discontinue antidepressant therapy at some point during the following 60 days with those of patients who continue antidepressant therapy beyond this period. A greater understanding of the determinants of antidepressant treatment patterns may help to identify patients at high risk of early antidepressant discontinuation.
Method
Sources of Data
Data were drawn from the household component of the Medical Expenditure Panel Survey (MEPS) for 1996–2001
(22,
23). To obtain a sample of sufficient size of new episodes of antidepressant treatment for depression, all available MEPS data were combined. These annual surveys were sponsored by the Agency for Healthcare Research and Quality to provide national estimates of the use of, expenditures for, and financing of health services.
The MEPS is conducted in a national probability sample of the U.S. civilian, noninstitutionalized population. Samples of 21,571 (in 1996), 32,636 (in 1997), 22,953 (in 1998), 23,565 (in 1999), 23,839 (in 2000), and 32,122 (in 2001) participants were drawn from 8,655 (in 1996), 13,087 (in 1997), 9,023 (in 1998), 9,345 (in 1999), 9,515 (in 2000), and 12,852 (in 2001) households, respectively. The response rates for the surveys were 70.2% in 1996, 66.4% in 1997, 67.9% in 1998, 64.3% in 1999, 65.3% in 2000, and 66.3% in 2001. In each survey, a designated household informant was queried about all related persons who lived in the home.
Structure of Survey
Each MEPS respondent is evaluated longitudinally over a 2.5-year period through six rounds of in-person interviews. Respondents are instructed to record health conditions, health events, and medication prescriptions as they occur in a calendar/diary. At the interviews, the diary is reviewed, and respondents are asked about their entries, including the reason for every outpatient visit and the name and dose of all medications used. After written permission is obtained from the survey respondents, survey staff contact medical providers to supplement and validate the diagnostic and other clinical information about the medical visits reported by the respondents.
Visits for Depressive Disorders
Respondents were asked the reason for every outpatient visit during the reference period. Conditions were recorded by interviewers as verbatim text and then subsequently coded by professional coders according to the ICD-9 as revised for the National Health Interview Survey
(24). Depression was identified if the respondents reported one or more outpatient visits that were subsequently coded with ICD-9/DSM-IV codes 296.2, 296.3, 300.4, or 311. Respondents were not specifically questioned about the severity of their depressive symptoms. Patients who reported use of mood stabilizer medications (lithium, carbamazepine, valproic acid, divalproex, gabapentin, and lamotrigine) during the study period were excluded from the analysis.
Sociodemographic and Clinical Characteristics
The MEPS data include information on the age, gender, self-identified race and ethnicity, current marital status, number of completed years of education, employment status, and income of respondents. On the basis of total annual family income, participants were grouped according to the U.S. Census Bureau poverty threshold as low income (<200% of the poverty threshold), middle income (200%–400% of the poverty threshold), or high income (>400% of the poverty threshold).
At the start of each round of interviews, the interviewers used items from the Medical Outcomes Study 36-Item Short-Form Health Survey
(25) to probe for the respondents’ perceptions of their mental and physical health status. In the current analysis, we selected ratings from the round preceding the first use of an antidepressant medication for depression. Responses on the instrument’s 5-point Likert-type scale were dichotomized as follows: ratings of excellent, very good, or good versus ratings of fair or poor
(25)Social limitation was assessed with a probe to determine whether individuals were “limited in participating in social, recreational, or family activities because of an impairment or a physical or a mental health problem.” Cognitive limitations were assessed with a probe to determine whether individuals “experience confusion or memory loss that interferes with daily activities or have problems making decisions to the point that it interferes with daily activities or requires supervision for their own safety.”
Service Access and Mental Health Services
The MEPS includes evaluation of whether participants have a usual source of care, defined as “a particular doctor’s office, clinic, health center, or other place that [the person] usually goes if [he or she] is sick or needs advice about [his or her] health.” In addition, detailed information is collected concerning health insurance coverage. In the current analyses, participants were classified into one of three groups—private insurance, public insurance, or no insurance—on the basis of their health insurance coverage at the start of the round preceding the initial antidepressant use. Information was also available concerning private prescription insurance coverage.
Participants in the MEPS are asked to report the type of care provided during each outpatient visit by selecting from among various response categories displayed on a flash card. Psychotherapy was defined as health care visits during the period of antidepressant treatment in which “psychotherapy/mental health counseling” was provided.
MEPS respondents who use medications are asked to record in a calendar/diary the names of all prescribed medications purchased or otherwise obtained, the number of times obtained, and the conditions associated with each medicine. Use of all prescribed medicines associated with each health care visit was reviewed during the MEPS interview. Psychotropic medications were classified by therapeutic class as antidepressants, anxiolytics, or antipsychotics, according to the National Drug Code
(26). For analytic purposes, antidepressants were subclassified into three groups: selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) (fluoxetine, sertraline, paroxetine, fluvoxamine, citalopram, venlafaxine, and venlafaxine extended-release), other newer antidepressants (mirtazapine, bupropion, and nefazodone), or tricyclic antidepressants and other older antidepressants, including trazodone, doxepin, and monoamine oxidase inhibitors.
Episodes of Care
The analysis was limited to data for adults age 18 years and older who initiated a new episode of antidepressant treatment for depression during the survey period. New episodes were defined by the absence of any treatment for depression during the preceding interview round. Data for adults who received treatment for depression in the first round were included only if the respondents indicated that their first use of an antidepressant medication occurred at least 45 days after the start of the round. To prevent right censoring, data for patients who initiated antidepressants within 90 days of completing the survey period were excluded.
Because of the focus on early treatment discontinuation, the analysis was further limited to data for respondents whose first antidepressant prescription was for 30 or fewer days. To examine associations with types of antidepressant medications, the analysis was restricted to data for patients who were treated with only one antidepressant during the study period. A preliminary analysis revealed that 93.8% of all initial antidepressant prescriptions for depression were for a supply for 30 or fewer days and that 73.9% of the patients who received antidepressants for depression were treated with only one antidepressant medication.
Various definitions have been used to define termination of an antidepressant treatment episode by using prescription data, including no evidence of a refill
(19); gaps of 9 months
(27), 90 days
(11), or 30 days
(28); and various proportions of prescribed pills
(15,
29). In the current study, gaps of greater than 30 days in the self-report prescription record were considered discontinuous treatment.
Analytic Plan
On the basis of the prescription data, the patients were first classified as discontinuing antidepressant medications during the first month (1 to 30 days) or continuing beyond this period (≥31 days). The primary analyses involved comparison of the sociodemographic, clinical, service access, and mental health service characteristics of these two patient groups. In addition, by using data from patients who continued antidepressant therapy for more than 30 days, an exploratory analysis was conducted to evaluate whether clinical characteristics and service access variables were differentially associated with continuing antidepressant treatment for more than 90 days.
The chi-square test was used to examine the strength of association between treatment duration group and sociodemographic, clinical, and other patient characteristics. Wald’s F tests were used to identify differences in means for continuous variables. Alpha was set at 0.05 (two-tailed). We used a logistic regression model to evaluate the effects of the sociodemographic, clinical, service access, and mental health service characteristics on the likelihood that patients would continue antidepressant therapy beyond the first 30 days of treatment. In this analysis, adjustment was made for patient age, sex, race/ethnicity, and perceived mental health status in order to examine the independent associations of each covariate. Among patients who continued antidepressants for more than 30 days, similar models were used to predict continuity of antidepressant treatment beyond 90 days. Separate models were used for each independent variable. The results are presented as adjusted odds ratios with 95% confidence intervals (CIs).
The Agency for Healthcare Research and Quality devised weights to adjust for the complex survey design and to yield unbiased national estimates. The sampling weights were also used to adjust for nonresponse and poststratification to population totals on the basis of U.S. census data. A complete description of the design, sampling, and adjustment methods is presented elsewhere
(22,
23). All statistical analyses were performed by using the SUDAAN statistical software package
(30) to accommodate the complex sample design and weighting.
Results
Continuity of Treatment
Approximately four of 10 patients (42.4%) who initiated antidepressant treatment for depression discontinued the antidepressant medication during the first 30 days of treatment. Among those who continued antidepressant therapy beyond 30 days, roughly one-half (52.1%) discontinued the medication during the subsequent 60-day period. Overall, only about one-quarter of the patients (27.6%) continued antidepressant therapy for more than 90 days.
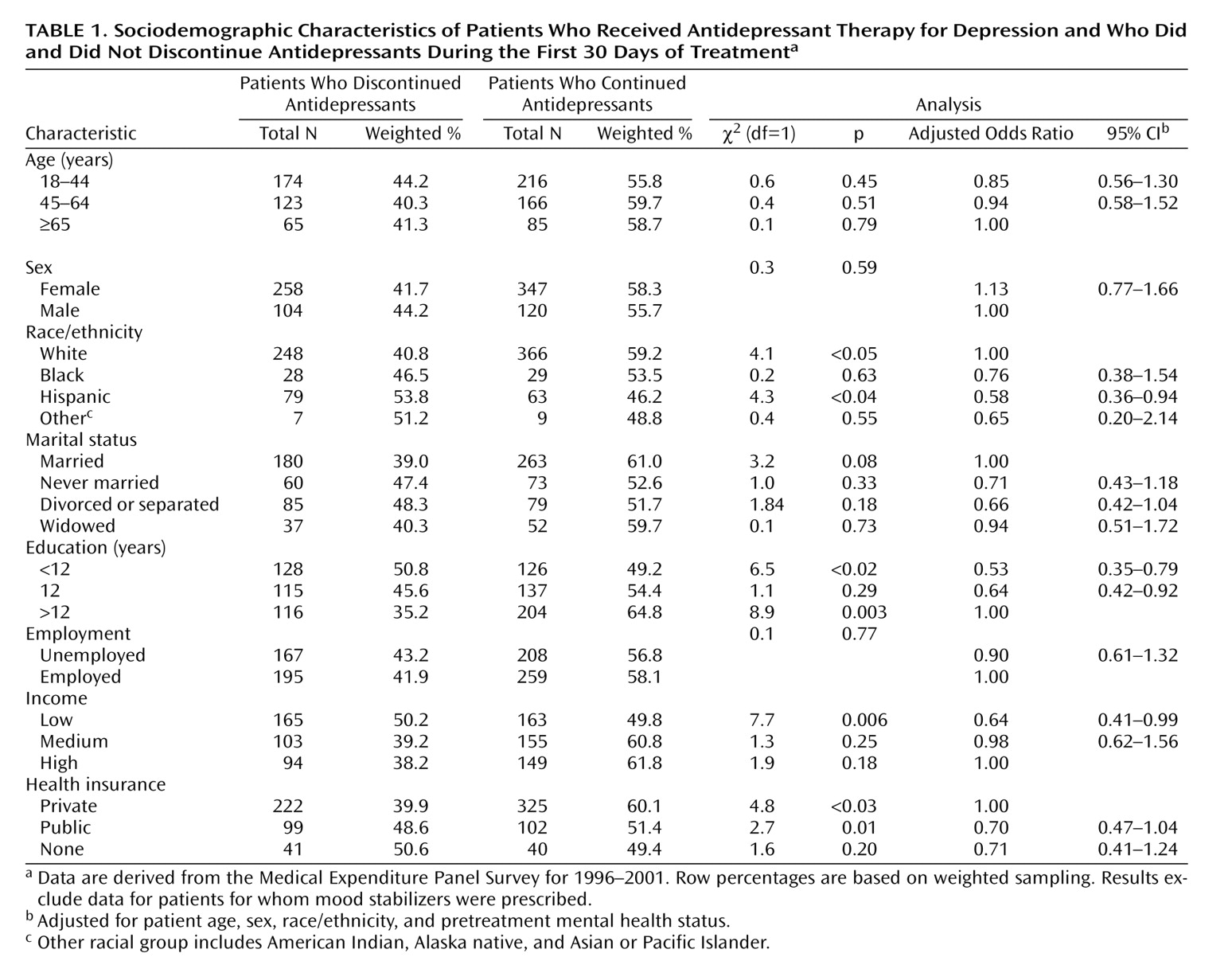
Sociodemographic Characteristics
Antidepressant discontinuation during the first 30 days of treatment was significantly more common among individuals of Hispanic ancestry (53.8%), compared with individuals of non-Hispanic ancestry (41.3%); patients with less than 12 years of education (50.8%), compared with those with more education (39.3%); and patients with low family incomes (50.2%), compared with those with medium or high family incomes (38.6%). By contrast, antidepressant discontinuation during the first 30 days was significantly less common among individuals who were white (40.8%), compared with nonwhite (51.2%); had completed more than 12 years of education (35.2%) rather than 12 or fewer years (48.0%); and had private health insurance (39.9%) rather than no health insurance or public health insurance (49.2%). After adjustment for age, sex, race, and pretreatment mental health status, Hispanic ethnicity, lower educational attainment (≤12 years), and low family income were significantly associated with discontinuation of antidepressants during the first 30 days of treatment (
Table 1).
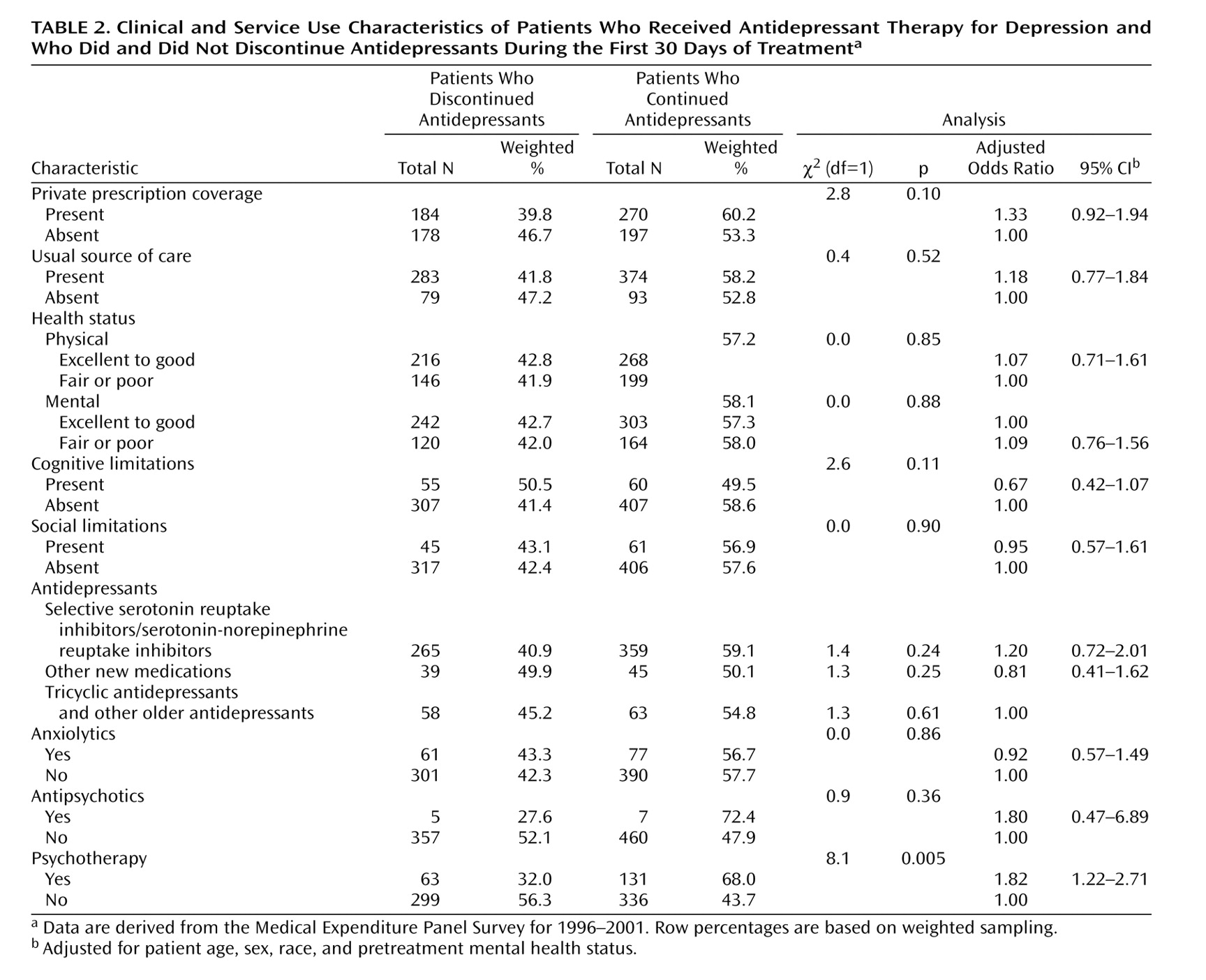
Clinical Characteristics
Patients who received psychotherapy were significantly more likely to continue antidepressants beyond 30 days than those who did not receive psychotherapy (
Table 2). Self-perceived physical and mental health status and limitations in cognitive and social function were not significantly related to continuing antidepressant therapy beyond 30 days.
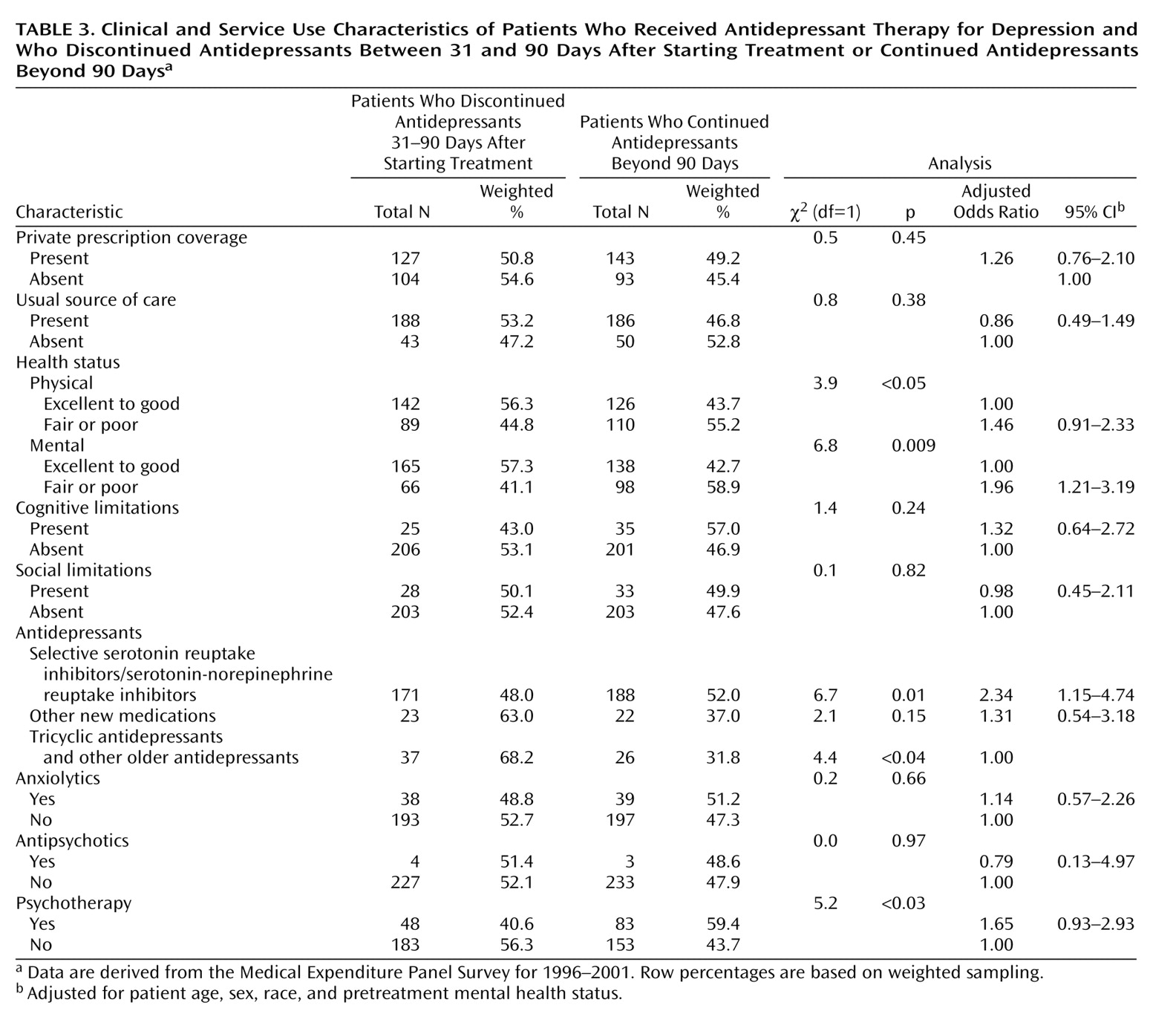
Longer-Term Antidepressant Continuity
Among patients who continued in treatment with antidepressant medications beyond the first 30 days, three clinical factors were associated with longer-term (90-day) antidepressant continuity. These factors were fair or poor perceived mental health status, treatment with an SSRI or SNRI antidepressant, and use of psychotherapy (
Table 3). After adjustment for patient age, sex, race, and perceived mental health status, the association of SSRI or SNRI treatment with longer-term antidepressant continuity remained statistically significant. Among patients who continued antidepressant medications beyond 30 days, patients treated with an SSRI or SNRI were an estimated 2.34 times more likely to continue beyond 90 days than were those treated with tricyclic antidepressants or other older antidepressant medications. Fair or poor perceived mental health status also remained significantly associated with longer-term antidepressant continuity in the multivariate model (
Table 3).
A great majority of patients in the SSRI/SNRI group were treated with an SSRI (89.8%) rather than an SNRI (10.2%). A separate regression analysis was performed to examine associations of SSRI, SNRI, and other newer antidepressant treatment with continuity of treatment beyond 90 days, with adjustment for patient age, sex, race, and perceived mental health status. In relation to treatment with a tricyclic antidepressant or other older antidepressant, treatment with an SSRI (odds ratio=2.31, 95% CI=1.13–4.71), but not an SNRI (odds ratio=3.00, 95% CI=0.82–10.95) or other newer antidepressant (odds ratio=1.31, 95% CI=0.54–3.18), was significantly associated with continuation of treatment beyond 90 days.
Discussion
Approximately four of 10 adults in the United States who initiate antidepressant therapy for the treatment of depression discontinue their medications during the first month of treatment. This finding from a nationally representative sample corroborates earlier observations from various treatment settings that early discontinuation of antidepressant medications is a common occurrence in the community treatment of depression
(5,
11).
Several correlated patient sociodemographic factors were significantly related to whether patients continued antidepressants beyond the acute phase of treatment. Hispanic patients and patients of lower socioeconomic status, as indicated by low family income and fewer than 12 years of education, were at an increased risk of early antidepressant discontinuation.
An earlier analysis of the 2000 MEPS data that combined data for new and ongoing treated cases reported that patient race/ethnicity and type of health insurance were not significantly related to adequate treatment of depression or bipolar disorder
(31). However, the effect of combining new treatment cases with the far more common ongoing cases probably obscured determinants of early antidepressant treatment discontinuation. Ethnic and economic disparities appear to be important not only in initial treatment seeking
(31,
32) but also during the critical early phase of treatment
(13,
33). The role of socioeconomic factors may be less apparent in later phases of care when treatment routines have become more established
(33).
Consistent with previous observational
(9,
11,
19) and experimental
(17,
20,
21) studies, we found that patients treated with SSRI or SNRI antidepressants are significantly more likely to continue their medications than are patients treated with tricyclic antidepressants and other older antidepressants. Significant effects of antidepressant selection on medication discontinuation were evident, not in the first month of treatment but during the following 2 months of treatment. It is possible that patients’ concerns related to medication tolerability increase in salience during the course of antidepressant treatment, although selection effects may account for this association.
We found that among patients who continued antidepressants beyond the first 30 days of treatment, poor perceived mental health status was significantly related to continuation beyond 90 days. Patients who perceive that they have a more serious mental health problem and who continue antidepressant therapy through the acute phase of treatment may have a relatively high motivation to continue antidepressant medications into longer-term maintenance treatment. In addition, health care professionals may provide more support and encouragement for long-term maintenance treatment to their more severely ill depressed patients.
Use of psychotherapy was also related to antidepressant continuity. The effects of psychotherapy on continuity of antidepressant treatment appear to be especially salient during the early phases of treatment. The combination of psychotherapy and pharmacotherapy is often a highly effective treatment for depression
(1). Although not all depressed patients may require such intensive treatment, one advantage of combined treatment may be greater continuity of the antidepressant therapy.
The study is constrained by several limitations. In the MEPS, data are collected from household informants who may not be fully aware of all of the services used by members of the household. Stigma and recall problems also threaten the validity of the survey data. Antidepressant treatment was measured with self-report diaries reviewed by survey interviewers rather than by pill counts, claims records, or electronic monitoring, which may yield more accurate information. However, self-report and claims data demonstrate good concordance for the antidepressant treatment of depression
(34). In contrast to the other patient characteristics, which were assessed before the start of antidepressant treatment, use of psychotherapy was assessed during the period of antidepressant treatment. As a result, for some patients psychotherapy may be a consequence of longer antidepressant treatment rather than a cause of longer treatment. Errors in measurement of the duration of antidepressant therapy may have been introduced by imputing the duration of the antidepressant prescriptions. The absence of data on the sector of care is another significant limitation. Although some evidence suggests lower rates of premature antidepressant discontinuation among patients who receive care from mental health specialists rather than primary care providers
(28), this finding may represent selection bias rather than a true causal relationship. Similarly, the association between newer antidepressants and continuity may be partially explained by selection bias that was not fully controlled in multivariate analyses. Errors in the reporting of diagnoses or a preponderance of relatively mild depression may help to explain the observed frequency of brief treatment episodes. Several clinical characteristics that may be important determinants of early antidepressant discontinuation, such as distressing side effects, stigma, personality factors, breakdown of the therapeutic alliance, and pessimism about the value of treatment, were not measured in the current study
(33). The analyses also excluded data for patients who switched antidepressants; these patients constituted approximately one-quarter (26.1%) of the total sample. Inclusion of the data for these patients would decrease the estimated rate of early antidepressant discontinuation. Finally, a substantial proportion of the sampled households did not participate in the surveys. Although we cannot be certain of the effect of survey nonresponse on the study findings, extensive statistical adjustments were made by the Agency for Healthcare Research and Quality for nonresponse.
The risk of early antidepressant treatment discontinuation is substantial, especially among socioeconomically disadvantaged individuals. In this nationally representative sample of adults initiating antidepressant treatment for depression, discontinuation during the first 30 days of treatment was significantly related to Hispanic ancestry, low total family income, less than 12 years of formal education, and absence of private health insurance. In addition to being related to well-known disparities in treatment seeking, sociodemographic factors are also related to continuity during the early phase of antidepressant treatment. As clinical
(8) and organizational
(35) efforts are made to improve the continuity of care for depression, priority should be given to the socioeconomically disadvantaged populations that are most vulnerable to early treatment discontinuation.