Obsessive-compulsive disorder (OCD) has been increasingly conceptualized as multidimensional, with a range of different subtypes identified
(1) . Recently, factor and cluster analyses have provided consistent evidence of distinct obsessive-compulsive symptom dimensions, including contamination/washing, doubt/checking, and symmetry/ordering
(2 –
6) . These symptom dimensions have been related to different clinical features, such as comorbidity
(2,
3,
7) . It has also been hypothesized that symptom dimensions may be affected by distinctive psychobiological mechanisms, whether neuronal or genetic, and so may have differential treatment response
(1,
3,
4,
6,
8 –
10) .
If OCD symptom dimensions do in fact reflect universal psychobiological mechanisms, then one would expect significant uniformity in the structure of symptom dimensions across time, geography, and cultures. With its unique culture, Japan provides a useful contrast to studies conducted in Western countries. In the current study, we factor analyzed the symptom checklist of the Yale-Brown Obsessive Compulsive Scale using data from a large group of Japanese OCD patients in order to examine whether symptom dimensions were stable across cultures.
Method
Subjects were outpatients who met DSM-IV criteria for OCD (N=343). Each subject was diagnosed using the Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P)
(11) . Information was obtained regarding demographic profile, family and medical history, and clinical features and course. Global functioning was assessed using the Global Assessment of Functioning (GAF) Scale. Ratings of OCD symptoms were obtained using the Japanese version of the Yale-Brown Obsessive Compulsive Scale
(12,
13) . Each of the 13 major symptom categories on the checklist, except for miscellaneous obsessions and compulsions, was scored as 0=absent, 1=present, or 2=predominant. The Yale-Brown Obsessive Compulsive Scale was then administered to assess current OCD symptom severity.
After pretreatment assessment, each subject was treated with a standardized combination of serotonin reuptake inhibitors (clomipramine, fluvoxamine, or paroxetine) and cognitive behavior therapy. Treatment was usually initiated with daily dosages of either 50 mg of clomipramine or fluvoxamine or 10 mg of paroxetine. If the medication was tolerated, dosage was gradually increased over 4 weeks to a maximum of 250 mg/day for clomipramine and fluvoxamine or 50 mg/day for paroxetine. Cognitive behavior therapy using exposure and response prevention was subsequently initiated with psychoeducational interventions and behavioral analysis. Atypical antipsychotics such as risperidone or olanzapine were added if subjects were nonresponsive to at least two trials of serotonin reuptake inhibitors combined with cognitive behavior therapy
(10) . Treatment response at 1 year was evaluated using change in Yale-Brown Obsessive Compulsive Scale total score.
Principal components analysis with a varimax rotation was conducted on the Yale-Brown Obsessive Compulsive Scale symptom checklist, in accordance with the original method
(2,
4) . The number of factors was determined using Kaiser-Guttman criterion; a scree plot and interpretability of the factors were also considered. To evaluate the structural integrity of these factors, Pearson correlations with Bonferroni correction were used for each symptom category. Pearson correlation coefficients were also used to examine the relation of symptom dimensions to clinical variables (e.g., age at onset, global functioning, and 1-year treatment outcome). Because of multiple testing, a lower level was set for significance (p<0.005).
Results
Subjects were men (N=142) and women (N=201) ranging from 15 to 68 years old (mean=30.4, SD=9.4). All subjects had primarily suffered from OCD for at least 2 years, with a mean duration of 7.8 years (SD=5.6). Mean age at onset was 22.6 years old (SD=7.4), mean duration of education was 12.9 years (SD=2.5), and mean GAF score was 49.6 (SD=7.5). Thirty-seven percent of subjects were married and 44% of subjects had lifetime comorbid major depression. At pretreatment assessment, mean Yale-Brown Obsessive Compulsive Scale total score and obsession and compulsion subscale scores were 26.9 (SD=4.8), 13.7 (SD=2.5), and 13.2 (SD=2.8), respectively. Fourteen percent (N=48) of subjects dropped out during the 1-year treatment period. In the remaining 295 patients, the mean decrease in the Yale-Brown Obsessive Compulsive Scale total score was 40.7% (SD=19.7).
All but 17 subjects (5%) with pure obsessions presented a mixture of obsessions and compulsions. Contamination obsession (48%) was the most common obsessive symptom, followed by obsession with symmetry or exactness (42%) and miscellaneous (38%) and aggressive obsessions (36%). Rates of hoarding, somatic, sexual, and religious obsession were 12%, 12%, 10%, and 8%, respectively. Both checking and washing compulsions were the most common compulsive symptoms (47%), followed by repeating rituals and miscellaneous compulsions (31% each) and ordering (22%), counting (14%), and hoarding compulsions (12%).
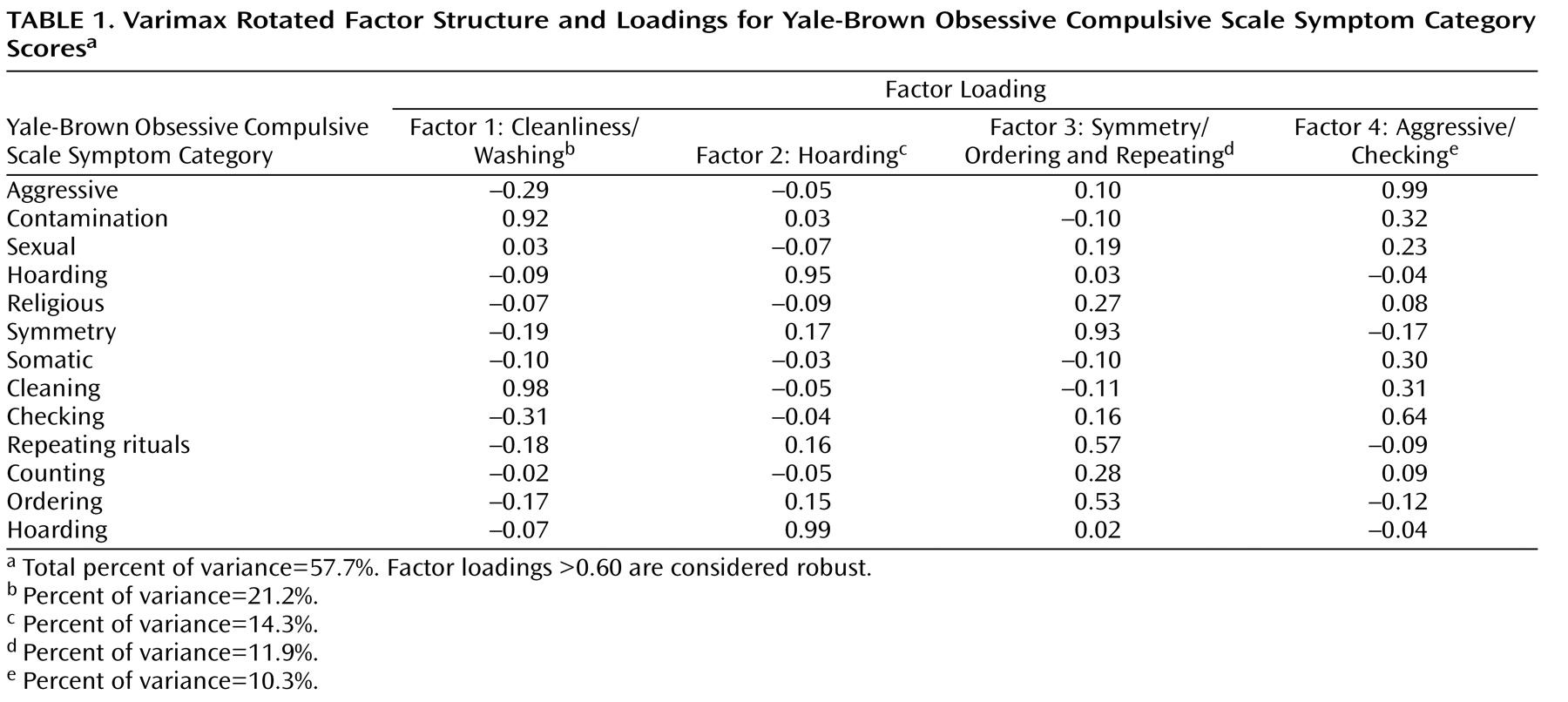
The principal components analysis of the 13 Yale-Brown Obsessive Compulsive Scale symptom checklist categories identified four factors accounting for 57.7% of variance: 1) contamination/washing, 2) hoarding, 3) symmetry/repeating and ordering, and 4) aggressive/checking (
Table 1 ). The first factor accounted for 21.2% of the variance and predominantly included contamination obsessions and cleaning compulsions. The second factor, accounting for 14.3% of the variance, included only hoarding obsessions and compulsions. The third factor included symmetry obsessions and repeating and ordering compulsions and had high factor loadings (>0.5), accounting for 11.9% of the variance. Aggressive obsessions and checking compulsions, the fourth factor, had high factor loadings as well (>0.6), accounting for 10.3% of the variance.
Pearson correlations demonstrated significant associations between the major Yale-Brown Obsessive Compulsive Scale symptom checklist categories (p<0.005). The most robust correlations (>0.6) were between 1) contamination obsessions and cleaning compulsions, 2) aggressive obsessions and checking compulsions, 3) hoarding obsessions and compulsions, and 4) symmetry obsessions and both repeating rituals and ordering compulsions. In addition, a relatively robust correlation (>0.4) existed between aggressive obsessions and cleaning compulsions and between somatic obsessions and checking compulsions. In these analyses, religious obsessions also exhibited significant correlations with both repeating rituals and counting compulsions.
Significant correlations (p<0.005) were found between the symmetry dimension score and age at onset (–2.26), duration of education (–1.79), GAF score (–2.50), pretreatment total score (2.52), and 1-year percentage improvement on the Yale-Brown Obsessive Compulsive Scale (–1.72). Statistically significant correlations were also observed between the hoarding dimension score and both the GAF score (–1.62) and 1-year percentage improvement on the Yale-Brown Obsessive Compulsive Scale (–2.23).
Discussion
To our knowledge, this is the first study to investigate OCD symptom structure in a large patient group from an Eastern country. A set of four symptom dimensions explaining 57.7% of variance emerged. The four dimensions were labeled 1) cleanliness/washing, 2) hoarding, 3) symmetry/ordering and repeating, and 4) aggressive/checking. These symptom dimensions are highly consistent with those obtained in previous factor and cluster analysis studies conducted in Western countries
(2 –
6), suggesting transcultural stability in the symptom structure of OCD and the involvement of universal psychobiological mechanisms in the pathogenesis of the disorder.
In this study, the symmetry dimension was significantly associated with both early age at onset and pretreatment severity on the Yale-Brown Obsessive Compulsive Scale. Both the symmetry and hoarding dimensions were significantly associated with decreased global functioning and poorer treatment outcome. These findings are again consistent with studies done in Western countries
(1,
3,
4,
10) and may help point to the nature of the underlying mechanisms of OCD. There is growing evidence that early-onset OCD is a unique subtype of OCD, characterized by greater occurrence of symmetry/ordering compulsions
(1), and that OCD patients with hoarding compulsions may have unique neuronal correlates and a poorer response to serotonin reuptake inhibitors
(4,
9) .
The results of this study suggest that the symptom structure of OCD, as factor analyzed using the Yale-Brown Obsessive Compulsive Scale symptom checklist, may be rather stable transculturally. Differential characteristics of clinical and treatment profiles of each dimension in this study may further validate the putative symptom dimensions from a cross-cultural perspective. However, some limitations of this study deserve mention. The analysis relied on categories of symptoms, rather than individual symptoms, and miscellaneous obsessions and compulsions were excluded from the analyses. In addition, somatic and religious concerns did not fall under any particular factor, making it difficult to compare the structure of these symptoms with previously obtained factor solutions
(6) . Additional studies with larger samples that include those treated in general rather than specialized settings and that focus on individual symptoms may further clarify the effect of cultural context on OCD symptom structure. Future psychobiological research in Japanese OCD populations, especially with regard to molecular, genetic, or neurobiological evidence, are needed to help delineate the precise and universal mechanisms of the different OCD symptom dimensions
(14) .