Can preschool children develop posttraumatic stress disorder (PTSD)? If so, are the DSM-IV criteria developmentally sensitive enough to diagnose the disorder in this group? Nine studies have addressed these questions, finding consistently that the answer to the former question is yes, and to the latter, no
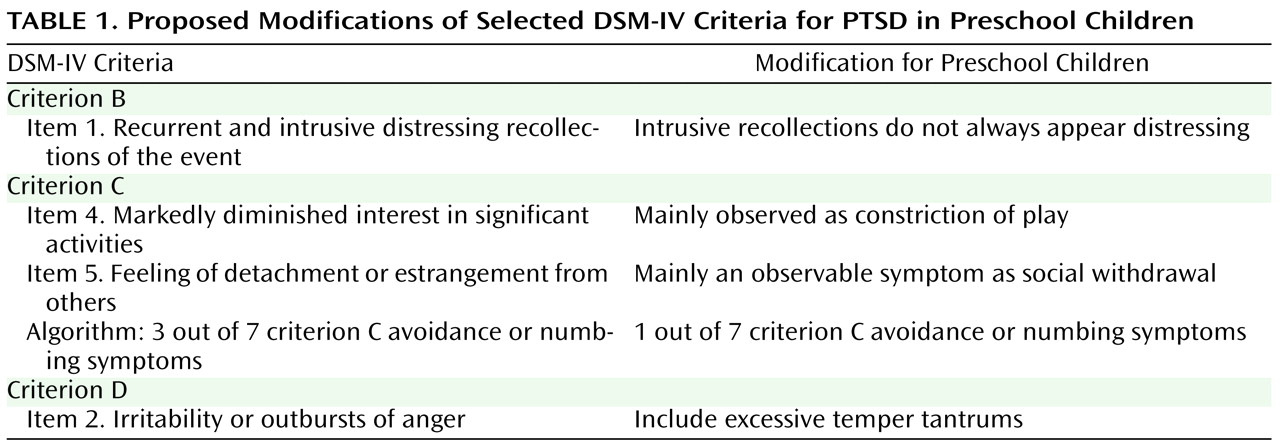
(1) . However, an empirically derived alternative set of criteria for preschool children appears valid for reliably diagnosing PTSD. The proposed alternative criteria include modifications in wording for four symptoms to make them developmentally sensitive to young children without changing the essence of the symptoms (
Table 1 ). Consensus was reached among experts to modify wording and to lower the requirement for criterion C (numbing and avoidance items) from three of seven symptoms to just one
(2) . Criterion C includes either symptoms that are highly internalized and difficult to detect if they are present in young children with emerging verbal capacities (e.g., avoidance of internal thoughts or feelings) or symptoms that are developmentally implausible at this age (e.g., sense of a foreshortened future). Note that lowering the threshold for criterion C has been suggested even for adults, because highly symptomatic and impaired adults could not be given the diagnosis if they had only two criterion C symptoms
(3) .
In this issue, Meiser-Stedman et al.
(4) assessed 60 children 2–6 years old and 49 children 7–10 years old 2–4 weeks after traumatic motor vehicle accidents and again 6 months later on both the DSM-IV criteria and the alternative criteria. At least six contributions of this study are worth highlighting.
First, this is one of the larger studies to date on this issue. The rate of PTSD diagnosis by the alternative criteria was 10.0%, compared with 1.7% by the DSM-IV criteria. The mean number of DSM-IV symptoms in children diagnosed with the alternative criteria was 10.0, indicating that these children were severely symptomatic even though fewer criteria were necessary to make a diagnosis using the alternative criteria. A mean of 10.0 symptoms is higher than in most adults diagnosed with PTSD
(5), and as prior studies have concluded, it seems implausible that children who have so many PTSD symptoms and impairment are unable to receive a DSM-IV diagnosis.
Second, in a prospective design, Meiser-Stedman et al. showed that 69% of the children diagnosed with the alternative criteria 2–4 weeks after the trauma retained the diagnosis 6 months later. These predictive validity data are another important reason for making developmental modifications in DSM criteria. This finding adds to preliminary longitudinal research suggesting that PTSD in children may be more unremitting than PTSD in adults. In contrast to adult studies, which typically show approximately 50% of patients improving naturally to some degree
(6), the first prospective longitudinal study of PTSD in preschool children showed that the mean severity did not decrease over a 2-year period
(7) . Similarly, a prospective study of 808 Australian schoolchildren (mean age=8.2 years) showed no decrease in stress symptoms 26 months after a destructive bushfire
(8) . In another study, 70% of 30 children 6–11 years old were still in the moderate to severe category of posttraumatic stress symptoms 21 months after surviving Hurricane Andrew
(9) . Unremitting PTSD takes on new salience in early childhood, a time of uniquely rapid brain development. Given speculation about potentially permanent alterations in the developing brain from early traumas, these preliminary data deserve attention.
A third contribution is Meiser-Stedman and colleagues’ inquiry into the developmental appropriateness of DSM-IV criteria for children 7- to 10-year-olds; theirs is only the second study to compare alternative and DSM-IV criteria for PTSD in the 7-to-10 age group. They found a rate of diagnosis of 18.8% by the alternative criteria, compared with 2.1% by DSM-IV criteria. Those diagnosed with the alternative criteria had a mean of 11.6 DSM-IV symptoms (by combined parent and child reports). Again, it seems implausible that children who have so many PTSD symptoms and impairment should be unable to receive a DSM-IV diagnosis.
Fourth, this is the first published study of acute stress disorder in preschool children; the authors found a rate of 1.6% in this age group, which is substantially lower than rates found in older populations. For comparison, the rates in the 7-to-10 age group were 3.9% by parent report, 22.9% by child report, and 29.2% by combined report. Since acute stress disorder requires the detection of dissociative symptoms, it is not clear whether the lower rate is due to underdetection or whether these symptoms do not develop as easily in preschool children.
Fifth, this was also the first study of preschool children to examine the predictive validity of acute stress disorder for later development of PTSD. With PTSD diagnosed by the alternative criteria at 6 months as the outcome measure, acute stress disorder was less predictive than simply making the diagnosis of PTSD with the alternative criteria 2–4 weeks after the trauma. Only one preschool child received a diagnosis of acute stress disorder, but six received a diagnosis of PTSD by the alternative criteria at 6 months, meaning that the diagnosis of acute stress disorder performed abysmally as a predictor of PTSD by the alternative criteria. For the 7-to-10 age group, however, a diagnosis of acute stress disorder based on combined parent and child reports was a slightly better predictor than the early diagnosis of PTSD by the alternative criteria, but still missed cases. Overall, acute stress disorder performed poorly as a predictor for PTSD, which is consistent with a review of studies on this subject
(10) .
Sixth, Meiser-Stedman et al. examined the often neglected issue of the accuracy of child reports versus parent reports versus combined reports. It should not be surprising, based on many studies with children, that parent-child agreement was poor (with values for Cohen’s kappa around zero for the diagnosis). There appears to be little that can be done about it practically, but this helps to quantify just how much information clinicians are missing by having access only to parent reports.
Clinical Relevance
Twenty-five years ago the question of whether children and adolescents could even develop PTSD was controversial
(11) . While that is no longer debatable, the question of younger children has become the latest focus of research. The data from this study fit with the consistent findings from prior studies that PTSD can be reliably detected in preschool children and that cases diagnosed by the alternative criteria are of high severity with functional impairment, and it suggests again that the alternative criteria are more developmentally sensitive and valid than the DSM-IV criteria. Longitudinal studies have indicated that diagnosed children do not simply “grow out” of stress symptoms and may have a more unremitting course than adults.
These findings are essential for justifying age-related modifications in criteria or even age-related subtypes of psychiatric disorders. Previous iterations of DSM criteria for PTSD have been published over the course of three editions, with few data available from children under age 18 and almost no data on children under age 12. DSM-V, which is currently in the planning stage, presents the first real opportunity to revise the criteria on the basis of studies with children and adolescents. The rigor and preciseness with which the diagnostic criteria have been examined in studies with preschool children, exemplified by the Meiser-Stedman et al. study, may even surpass what has been done for PTSD in adults. Only by ensuring that mental health professionals understand the developmental issues of PTSD in young children will we be able to detect the disorder in children and provide treatment. The needed changes seem clear.