Borderline personality disorder has a prevalence of 1%–2%
(1) and is associated with considerable morbidity and mortality, leading to substantial costs through premature death and high health care utilization
(2) . An estimated 69%–80% of patients with this disorder attempt suicide
(3,
4), and a higher percentage engages in nonsuicidal self-injurious behavior, which is itself a risk factor for suicide. The rate of completed suicide in this group is approximately 10%
(5) .
Until recently, borderline personality disorder was viewed as untreatable. Over the past 15 years, several studies have established the efficacy of different forms of psychotherapy in reducing core features of the disorder. Of the six psychotherapy approaches supported by empirical evidence
(6 –
17), dialectical behavior therapy has been the most studied. The first three of five published randomized controlled trials compared dialectical behavior therapy and treatment as usual and demonstrated its superiority in treatment retention and reducing suicidal behaviors
(6,
7,
18) . Two recent trials compared it with alternative rigorous psychotherapies; one demonstrated its superiority
(8) relative to psychotherapy delivered by experts, and the other found that it was generally equivalent to structured treatments for borderline personality disorder on the main outcome measures—depression, anxiety, global functioning, and social adjustment
(12) .
Given the growing empirical base, dialectical behavior therapy represents the current standard treatment for borderline personality disorder. However, more definitive information is needed regarding its efficacy relative to robust treatments delivered by clinicians with expertise in treating this patient population. There is also a need for large-scale replication studies conducted independently of the treatment developer. In this study, we compared dialectical behavior therapy and general psychiatric management, an active, manualized approach derived from APA recommendations
(19) including a combination of psychodynamically informed therapy and symptom-targeted medication management. We hypothesized that participants receiving dialectical behavior therapy would show greater reductions in the frequency and severity of suicidal and nonsuicidal self-injurious behaviors. This report presents clinical outcomes after 1 year of active treatment.
Method
This single-blind randomized controlled trial compared two 1-year manualized treatments for borderline personality disorder: dialectical behavior therapy and general psychiatric management. Both were delivered by clinicians with expertise in the treatment of this disorder. The former treatment was conducted at the Centre for Addiction and Mental Health, and the latter was offered at St. Michael’s Hospital, both University of Toronto teaching hospitals within the same health care system. Participants were enrolled between July 2003 and April 2006. The protocol was approved by each center’s research ethics board, and patients provided written informed consent prior to enrollment. Under the Canadian public health care system, participants did not pay for treatment.
For inclusion, patients had to meet DSM-IV criteria for borderline personality disorder, be 18–60 years of age, and have had at least two episodes of suicidal or nonsuicidal self-injurious episodes in the past 5 years, at least one of which was in the 3 months preceding enrollment. To maximize external validity, exclusion criteria were limited to having a DSM-IV diagnosis of a psychotic disorder, bipolar I disorder, delirium, dementia, or mental retardation or a diagnosis of substance dependence in the preceding 30 days; having a medical condition that precluded psychiatric medications; living outside a 40-mile radius of Toronto; having any serious medical condition likely to require hospitalization within the next year (e.g., cancer); and having plans to leave the province in the next 2 years.
Patients were assessed for DSM-IV diagnoses by assessors who were well trained on study instruments and blind to treatment assignment. Assessors were seven doctoral-level clinicians and one board-certified psychiatrist. Two standardized interviews were used: the Structured Clinical Interview for DSM-IV Axis I Disorders–Patient Edition
(20) and, to assess all axis II disorders, the International Personality Disorder Examination
(21) . High reliability was obtained for borderline personality disorder symptoms, with intraclass correlation coefficients ranging from 0.83 to 0.92. The Peabody Picture Vocabulary Test–Revised
(22) was administered to rule out low intelligence, using a cutoff score of 70. Assessors were polled after the treatment phase to ascertain whether they could correctly guess participants’ treatment assignment; they did not know treatment assignment for 86% of the cases, suggesting that blinding was largely maintained. The study coordinator, who was not blind to treatment assignment, collected data related to treatment history.
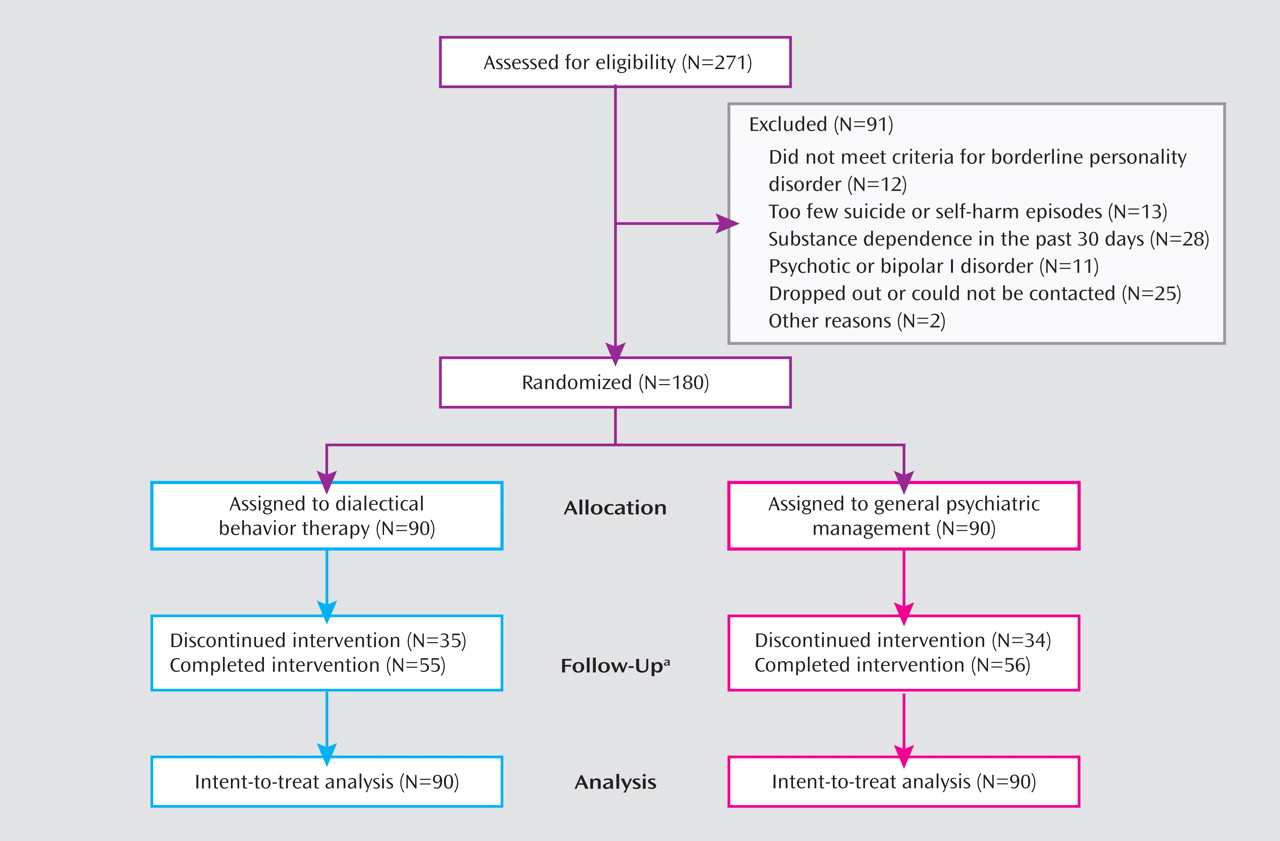
After baseline assessments, eligible participants were randomly assigned to treatment arms using a pregenerated block randomization scheme developed and held by the statistician, who prepared 45 sealed envelopes, each containing the group allocations in random order for four participants (see
Figure 1 ).
Treatment and Therapists
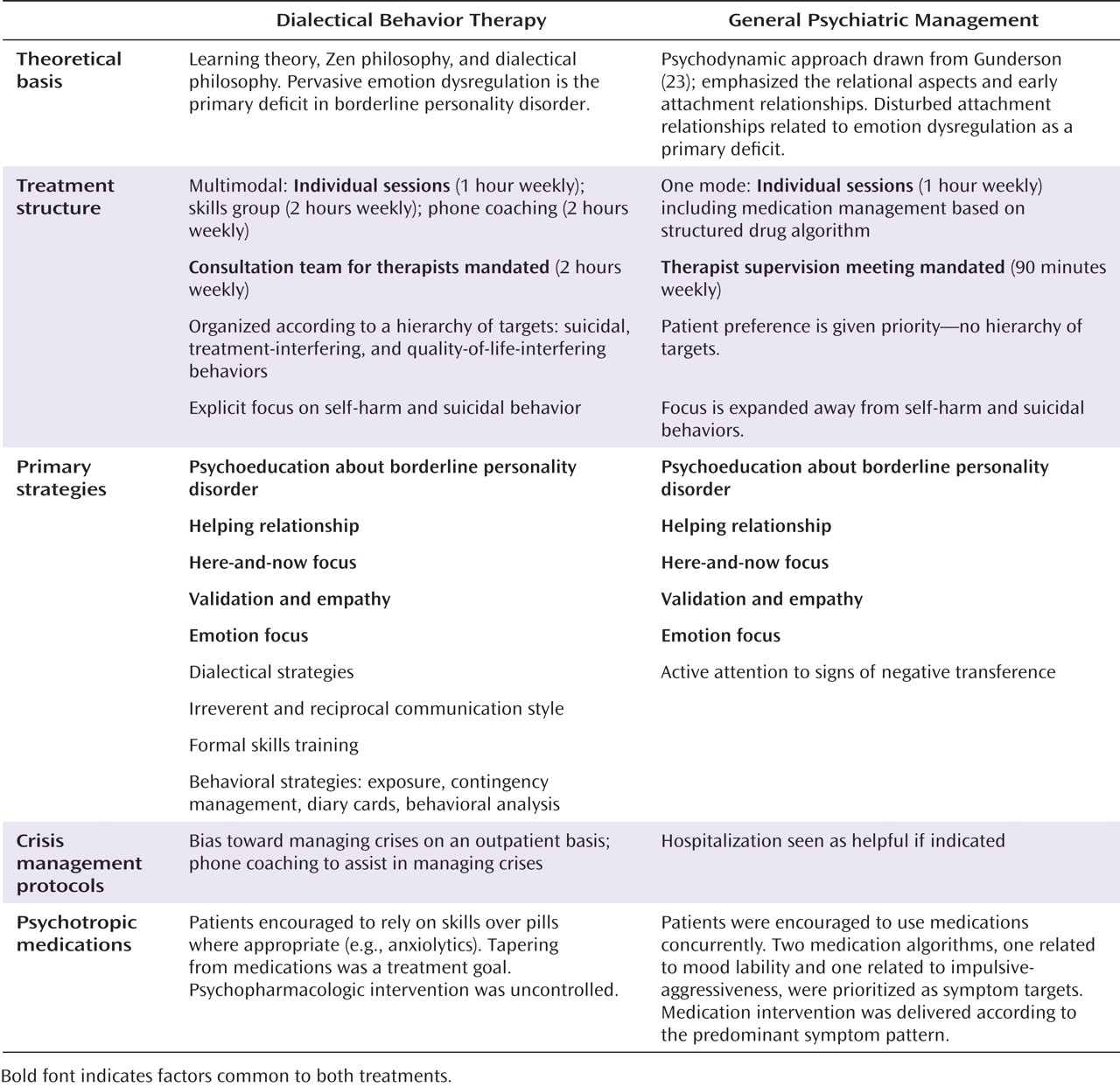
The essential elements of the treatments are listed in
Figure 2 . Dialectical behavior therapy consisted of the manualized cognitive-behavioral outpatient treatment developed by Linehan
(9,
10), the primary goal of which is to eliminate behavioral dyscontrol by helping patients develop more effective coping strategies. This therapy includes a diverse range of interventions, and its core strategies involve balancing validation with behavioral change. To maximize external validity, there were no restrictions on ancillary pharmacotherapy.
General psychiatric management was based on the APA Practice Guideline for the Treatment of Patients With Borderline Personality Disorder
(19) and manualized for this trial. This coherent, high-standard outpatient treatment consisted of case management, dynamically informed psychotherapy, and symptom-targeted medication management. Pharmacotherapy was based on the symptom-targeted approach but prioritized treatment of mood lability, impulsivity, and aggressiveness, as presented in the APA guideline. Consistent with routine psychiatric practice, participants were not prohibited from engaging in other psychosocial treatments with the exception of those that might overlap with dialectical behavior therapy (e.g., behavioral treatments).
Treatments were delivered by 25 therapists, all with a minimum of 2 years of clinical experience and a minimum of 1 year of experience treating borderline patients. There were no between-group differences in level of clinical experience (dialectical behavior therapy, mean=15.0 years [SD=9.58]; general psychiatric management, mean=14.2 years [SD=9.97]). Therapists included 11 psychiatrists (three and eight providing dialectical behavior therapy and general psychiatric management, respectively), five Ph.D.-level psychologists (four and one, respectively), six master’s-level clinicians (five and one, respectively), and three nurses (one and two, respectively). There were no between-group differences in the proportion of clinicians with doctoral-level degrees (M.D. and Ph.D.) versus other degrees, but there were significantly more physicians in the general psychiatric management condition (χ 2 =4.8, df=1, p=0.028).
Dialectical behavior therapists (N=13) had a minimum of 2 years of experience with the treatment. Two senior therapists, who had received intensive training in dialectical behavior therapy from Linehan and supervision from senior trainers from Linehan’s group, supervised therapists. The remaining 11 therapists received intensive training and/or other training workshops in dialectical behavior therapy. Over the course of the study, regular supervision was supplemented by consultation from international experts.
Therapists providing general psychiatric management were recruited because of their expertise, aptitude, and interest in treating individuals with borderline personality disorder. Therapists attended weekly group supervision facilitated by the developer of this approach and supplemented by consultation from international experts.
Modality-specific adherence scales were used to evaluate treatment fidelity. The dialectical behavior therapy global rating scale (M.M. Linehan, unpublished 1993 manuscript) was used to assess therapist application of strategies from a random selection of videotapes of sessions for all patient-therapist dyads. Scores on this instrument range from 1 to 5, with higher scores reflecting greater adherence to the dialectical behavior therapy model; scores <4 indicate that the rated session was not adherent, and scores ≥4 indicate that the session was adherent. Two independent raters who established reliability with Linehan’s team conducted ratings.
Adherence to general psychiatric management was rated on a 52-item self-report scale
(24) . Validity was demonstrated using two methods: concordance with ratings supplied by patients for the same therapy session rated by therapists (a total of 26 patient-therapist pairings) and two observer ratings of audiotaped sessions (a total of 23 sessions). Therapists completed the scale every 6 weeks for all patients.
Outcome Measures
The primary outcome measures were frequency and severity of suicidal and nonsuicidal self-injurious behavior episodes, as assessed by the Suicide Attempt Self-Injury Interview (M.M. Linehan et al., unpublished 1983 manuscript). This semistructured instrument has excellent interrater reliability ratings (ranging from 0.85 to 0.98)
(25) and has been used in several studies of dialectical behavior therapy
(7,
8,
18) .
Secondary outcome measures included diagnostic criteria for borderline personality disorder, psychiatric symptoms, anger, depression, interpersonal functioning, quality of life, health care utilization, and treatment retention. Measures included the Zanarini Rating Scale for Borderline Personality Disorder, a clinician-administered scale to assess DSM-IV borderline psychopathology
(26) ; the Symptom Checklist–90–Revised
(27), measuring general symptoms; the State-Trait Anger Expression Inventory
(28) ; the Beck Depression Inventory
(29) ; the Inventory of Interpersonal Problems, 64-item version
(30) ; and the EQ-5D thermometer
(31), which measures health-related quality of life. The Treatment History Interview (M.M. Linehan and H.L. Heard, unpublished 1987 manuscript) was used to obtain self-reported counts of the number of hospital admissions, days in hospital, emergency department visits, medications, and outpatient psychosocial treatments.
The Reasons for Early Termination From Treatment Questionnaire
(32) was administered to participants who terminated treatment prematurely to evaluate their reasons for discontinuation. Treatment retention was measured by the total number of weeks with at least one session and the number of weeks from the first to the last session attended. Patients were classified as having completed treatment if the time between the first and last sessions was at least 48 weeks. Patients who failed to participate in four consecutive scheduled sessions were categorized as dropouts.
Participants were compensated $10 per hour for follow-up assessments, which were conducted at baseline and every 4 months over the 1-year active treatment phase. A 2-year posttreatment follow-up phase is in progress.
Statistical Analysis
The power analysis was conducted using the effect size for suicidal behavior from Linehan’s original publication
(7), the only relevant study of dialectical behavior therapy available when this trial was designed. A minimally significant difference in outcomes between treatments was defined as a reduction of 20% or more in the rate of suicidal and nonsuicidal self-injurious behavior. Based on a power of 80% and assuming a 30% dropout rate and an alpha level of 0.05, a sample of 180 participants (90 per group) was required.
All results were analyzed using an intent-to-treat analysis (N=180). We also conducted a per-protocol analysis based on “treated” participants, defined as those who were in treatment for at least 8 weeks from initial session to last session. This included a total of 167 patients (dialectical behavior therapy, N=85; general psychiatric management, N=82).
The distributions of several outcome measures, such as self-harm, hospitalization days, and emergency department visits, were not normally distributed. A negative binomial distribution was selected to best represent these data for all analyses.
To test the adequacy of randomization, we conducted between-group comparisons of baseline characteristics on all measures, using t tests for continuous variables and chi-square tests for dichotomous variables. Differences in time to dropout from treatment (interval from first session to last session attended) were evaluated using a log-rank test.
The primary outcome measures and several of the secondary outcome measures were analyzed using a generalized estimating equation to account for the correlation in repeated measurement on individuals
(33) in the following form: log(μ) = μ
0 + β
1 condition + β
2 time + β
3 condition × time.
Mixed-effects linear growth curve models
(34) were used to analyze normally distributed secondary outcome measures. Both methods use full information, so participants with missing data were still included in the model. Each model was reanalyzed using preselected covariates that are known or theorized to affect the outcome. The best-fitting models were selected using deviance scores for generalized-estimating-equation and linear-growth-curve results. The results were compared with the primary models outlined above to determine whether including covariates caused meaningful changes in the overall findings.
Results
Baseline Characteristics
Of the 271 participants who were referred and screened, 91 were ineligible. The remaining 180 participants were randomly assigned to receive either dialectical behavior therapy (N=90) or general psychiatric management (N=90).
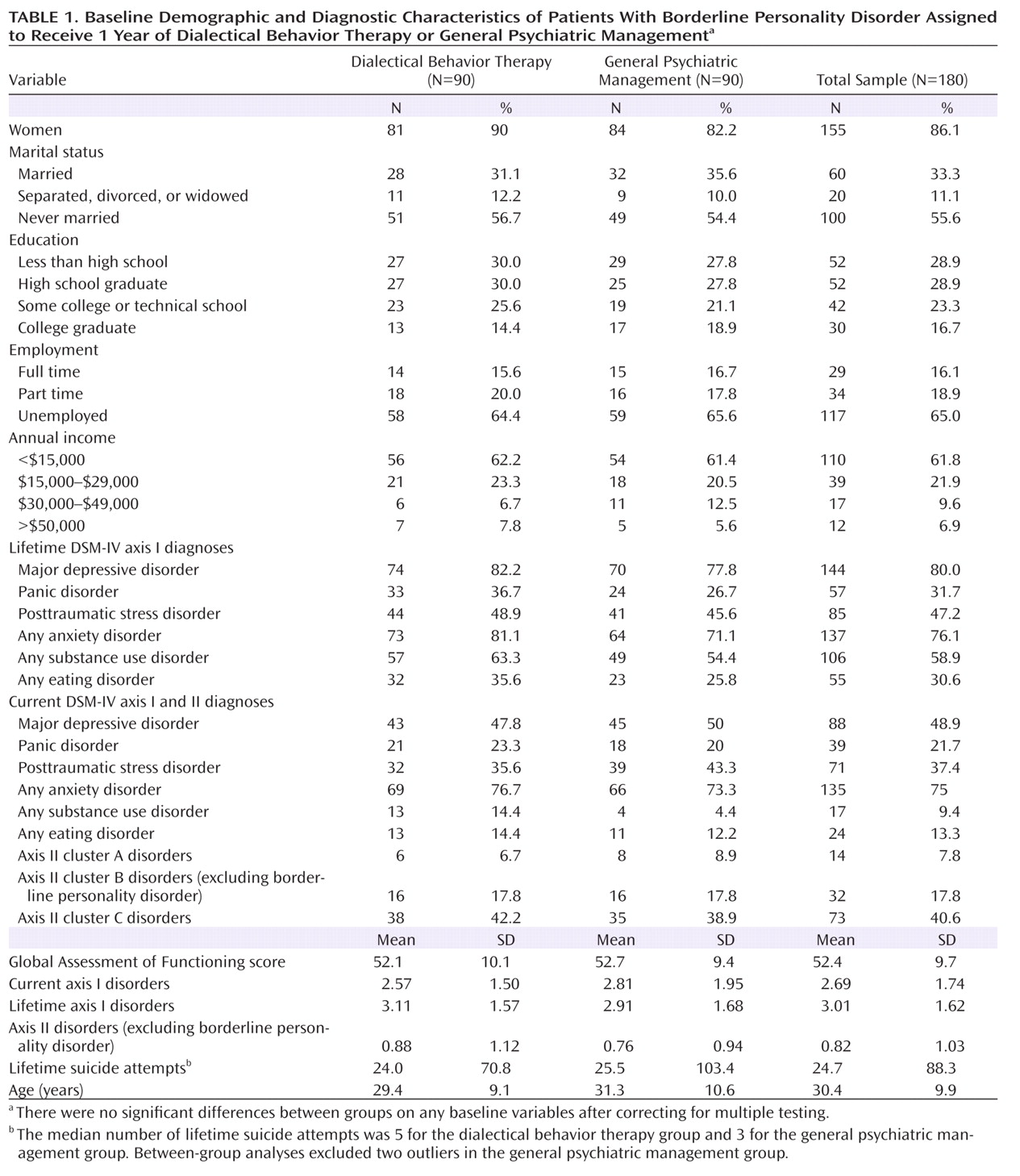
Demographic and clinical characteristics and suicidal behaviors are summarized in
Table 1 . After correction for multiple testing, there were no between-group differences on baseline demographic characteristics, diagnostic variables, or suicidal and nonsuicidal self-injurious behaviors.
Attrition and Treatment Implementation
Of the 180 participants, 111 (62%) completed 1 year of treatment. The average time between the first and the last session was 41 weeks (SD=16.9), with no significant between-group differences. In all, 35 (39%) patients in the dialectical behavior therapy group and 34 (38%) in the general psychiatric management group ended treatment prematurely. Based on survival analyses, there were no significant differences between groups in the timing of treatment dropouts. Patients in the dialectical behavior therapy group attended more weeks of treatment (i.e., weeks with at least one session) than patients in the general psychiatric management group (36 weeks [SD=17.57] compared with 27 weeks [SD=14.84]; p<0.001). There were no significant between-group differences in the mean number of individual sessions attended (dialectical behavior therapy, N=32 [SD=15.97]; general psychiatric management, N=31 [SD=27.05]). Patients assigned to dialectical behavior therapy attended a mean of 26 (SD=14.98) group therapy sessions.
At baseline, 145 patients (81.6%) reported that they were taking psychotropic medications (mean number of medications, 3.08 [SD=1.64]). Over the course of treatment, patients in dialectical behavior therapy averaged 1.84 (SD=1.44) medications, and those in general psychiatric management averaged 2.09 (SD=1.65), with no significant difference between groups. At baseline, there were no significant differences between groups in the use of non-study treatments (individual, group, case management, day treatment, or inpatient), although over the 1-year study period, the utilization of non-study treatments decreased significantly more in the dialectical behavior therapy group than in the general psychiatric management group (odds ratio=0.52, p=0.002). The mean number of non-study treatments over the treatment year was 0.32 (SD=0.49) for the dialectical behavior therapy and 0.54 (SD=0.62) for the general psychiatric management group.
A total of 83 patients in the dialectical behavior therapy group and 85 in the general psychiatric management group attended at least one postbaseline follow-up assessment. Participants completed an average of 2.52 (SD=0.89) follow-up assessments (dialectical behavior therapy group, mean=2.42 [SD=0.94]; general psychiatric management, mean=2.62 [SD=.83]), with no significant difference between groups.
A total of 69 patients discontinued treatment during the treatment year. Questionnaires on the reasons for termination were completed by 55%. The most commonly reported reasons were that individual sessions were not helpful (42%), that there were scheduling problems (32%) or transportation problems (32%), that group sessions were not helpful (29%), and that the problems improved (24%).
Adherence ratings were conducted on 90 patient-therapist dyads across 262 dialectical behavior therapy sessions. The mean score was 4.06 (SD=0.37), which was within the adherent range. Adherence to general psychiatric management interventions was supported based on a sample of 402 sessions comprising 65 of 90 patient-therapist dyads for which data were available. The mean adherence scores for essential interventions were significantly greater than the mean adherence score for proscribed dialectical behavior therapy items across all time points (early: t=14.93, df=62, p≤0.001; middle: t=12.77, df=51, p<0.001; late: t=13.25, df=48, p<0.001).
Outcome Analyses
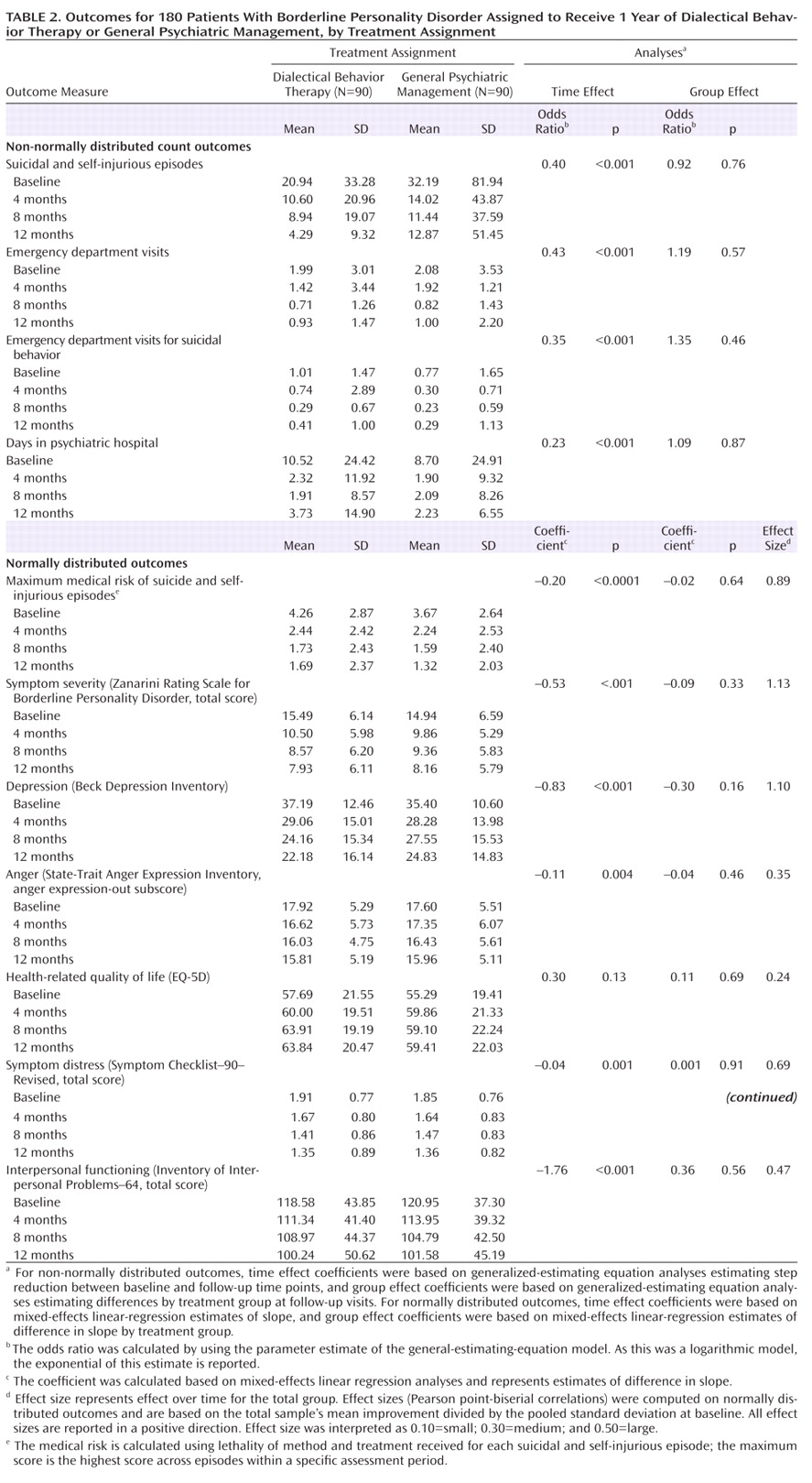
Patients in both groups made significant improvements on the majority of primary and secondary outcomes, as outlined in
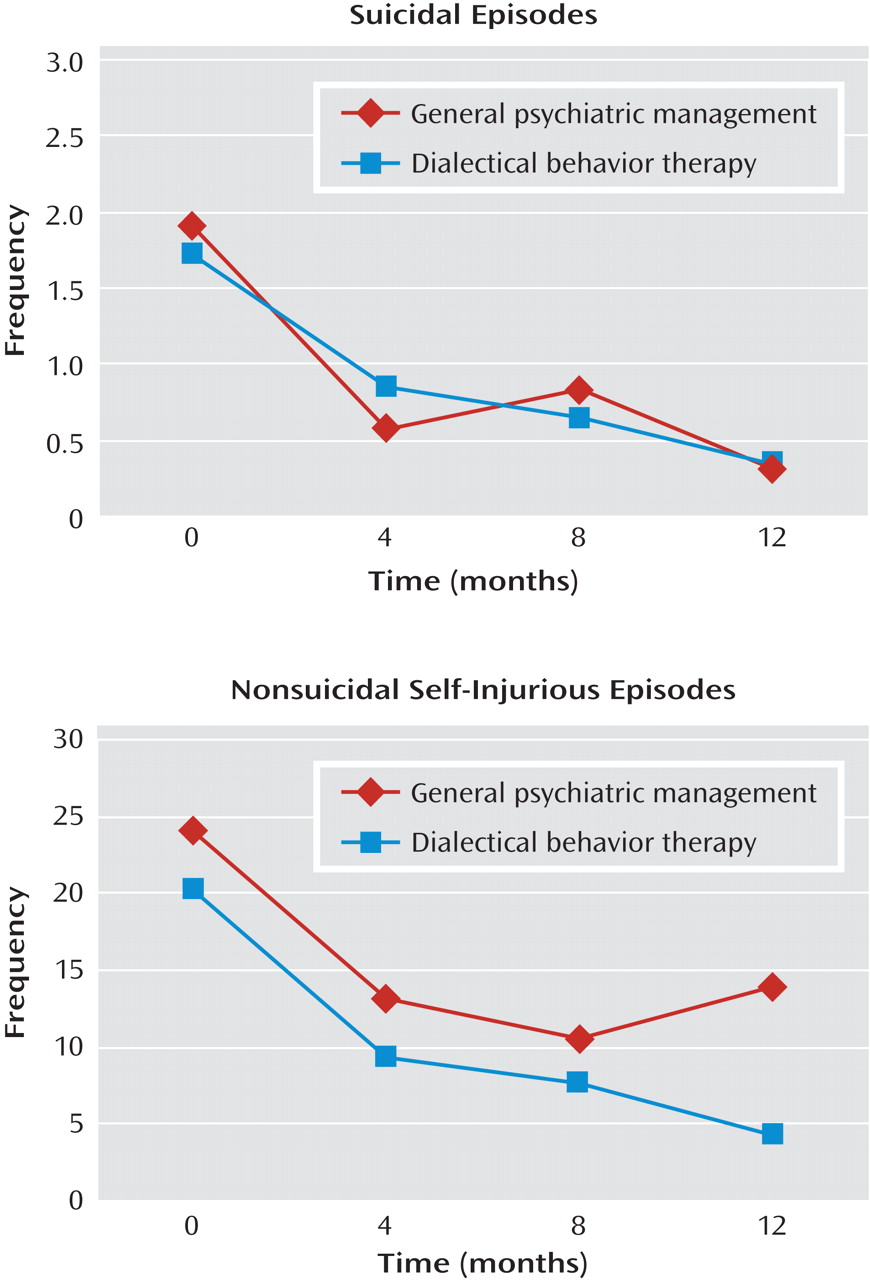
Table 2 . There were no deaths by suicide in either group. The mean numbers of suicidal and nonsuicidal self-injurious episodes over the treatment period are shown in
Figure 3 . Based on generalized-estimating-equation analyses, both groups showed statistically significant decreases in the frequency of suicidal episodes (odds ratio=0.23, p=0.01) and nonsuicidal self-injurious episodes (odds ratio=0.52, p=0.03) (these analyses exclude two outliers in general psychiatric management). There were no between-group differences in the frequency of suicidal episodes or nonsuicidal self-injurious episodes. Mixed-effects linear regression analyses revealed that those who had any suicidal or nonsuicidal self-injurious episodes experienced a significant decrease in the medical risk over time (slope=–0.20, t=–6.47, df=450, p<0.001), but there was no between-group difference (Δ slope=–0.021, t=–0.47, df=450, p=0.64).
Using mixed-effects linear growth curve analyses, significant decreases over the 1-year treatment period (but no between-group differences) were found for the following variables: borderline symptoms, depression, interpersonal functioning, symptom distress, and anger. On health-related quality of life (based on the EQ-5D thermometer), both groups reported improvements, but these changes were not statistically significant.
Based on generalized-estimating-equation analysis, participants in both groups showed statistically significant decreases in the total number of emergency department visits (odds ratio=0.43, p<0.0001), with no statistically significant differences between groups. Both groups demonstrated statistically significant reductions in the number of emergency department visits for suicidal behavior (odds ratio=0.35, p<0.0001), with no between-group differences. Adjusting for covariates did not alter any of the findings, nor did any analyses of patients who completed only 8 weeks of treatment.
Discussion
This trial demonstrated that 1 year of dialectical behavior therapy or general psychiatric management for the treatment of suicidal patients with borderline personality disorder brought about significant reductions in suicidal behavior, borderline symptoms, general distress from symptoms, depression, anger, and health care utilization, along with improvements in interpersonal functioning. Contrary to our expectations, dialectical behavior therapy was not superior to general psychiatric management with both intent-to-treat and per-protocol analyses; the two were equally effective across a range of outcomes. This is the largest trial comparing dialectical behavior therapy and an active high-standard, coherent, and principled approach derived from APA guidelines and delivered by clinicians with expertise in treating borderline personality disorder. These findings increase the range of viable treatment options for this disorder; effective treatment can involve specific forms of psychotherapy as well as specialized psychiatric management.
The study provides further evidence to dispel the myth that borderline personality disorder is untreatable and supports the thesis that this population can benefit from specific specialized interventions. It demonstrates that dialectical behavior therapy and general psychiatric management are both effective in bringing about change in a broad range of areas relevant to borderline functioning. Most outcome measures showed statistically significant improvement, with effect sizes ranging from moderate to large.
The study provides additional support for the efficacy of dialectical behavior therapy in treating borderline personality disorder, assessed on the basis of a wide range of outcomes. It also demonstrates the successful delivery of this therapy by clinicians working in a publicly funded health care setting in Canada, under circumstances typical of a real-world clinical setting.
The study is the first empirical evaluation of general psychiatric management. Evidence evaluating this approach is vital because psychiatrists frequently play a central role in the provision of care to this population. These results help legitimize the recommendations of the APA practice guideline on the management of borderline personality disorder and can inform the training of psychiatrists. However, additional studies of general psychiatric management are needed before strong conclusions can be drawn about its generalizability to psychiatric practice.
Several factors could account for the absence of differences in outcomes between treatments. While the delivery of dialectical behavior therapy may have been inferior to that in other trials, an analysis of adherence data suggests otherwise. The mean treatment fidelity ratings in this trial were within the range indicating adherence and were comparable to ratings recently reported by Linehan et al.
(8) . The treatment retention rate of 62% in the dialectical behavior therapy condition in our study was considerably lower than the 75% reported for the Linehan et al. trial
(8) but comparable to rates in other independent trials of dialectical behavior therapy (57% for Clarkin et al.
[12] and 63% for Verheul et al.
[18] ). Lower retention rates may be due to the availability of publicly funded treatment alternatives.
The failure to find treatment differences may be due to the superiority of general psychiatric management relative to the comparator treatments used in previous trials. It is possible that our study was not adequately powered to detect differences between dialectical behavior therapy and a highly active treatment. However, the effect sizes between groups were negligible, without any indication of trends toward differences, which suggests that significant differences found with a substantially larger sample would not justify altering clinical practice.
Factors common to the treatments may also account for the similar outcomes. While the treatments overlap in some areas (e.g., focusing on emotion, discouraging hospitalization), they differ in several ways (e.g., provision of structured sessions, skills training, behavioral analysis, dialectics, and target hierarchy). To check for contamination of dialectical behavior therapy into general psychiatric management, a random sample of general psychiatric management sessions (N=10) was rated on the dialectical behavior therapy adherence scale. Overall scores fell below adherence (<4.0), lending support to the idea that general psychiatric management was not a version of dialectical behavior therapy.
This study has some limitations. First, although general psychiatric management is a rigorous active treatment endorsed in APA guidelines, it has not been previously tested. Second, co-interventions were not rigidly controlled, in keeping with the goal of maximizing external validity. Third, the primary outcome measures—frequency and severity of suicidal and nonsuicidal self-injurious behaviors—were restricted to self-report and were therefore subject to responder bias. Finally, the study sample was predominantly female, without sufficient statistical power to analyze gender differences in the treatment effects.
Questions remaining for future research include identification of the mechanisms of action by which these treatments achieve their effects. There may be different pathways to change or common factors that account for the efficacy of these treatments. A better understanding of the specific and common factors that predict change can be used to enhance the efficacy of treatments.